 |
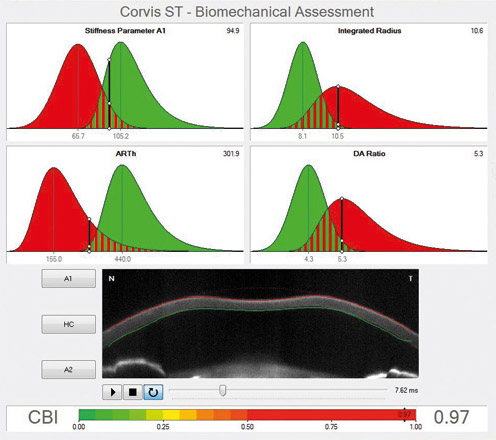
| Researchers found that the absolute value, not the change vs. baseline, in stress-strain index at one month of latanoprost treatment was the parameter able to predict the future risk of progression. Photo: Oculus. Click image to enlarge. |
Biomechanical parameters of the eye have been proven clinically relevant, both in IOP measurement and in risk profiling of glaucoma patients. Assessing corneal biomechanics may offer an indirect measurement of the lamina cribrosa/posterior sclera rigidity, and thus behave as a surrogate for the optic nerve susceptibility to glaucomatous damage. A team of researchers from Spain and Greece believed that understanding the effects of prostaglandin analogs on the biomechanical behavior of the eye is important and may confer information about the risk of future glaucoma progression. Using the Corvis Scheimpflug tonometer (Corvis ST) from Oculus, the team found that a higher value in the stress-strain index after one month of prostaglandin analogs is found in eyes that progress. Reduced values for “highest concavity” parameters, which suggest increased scleral stiffness, were also found in progressing eyes.
The study examined 63 newly diagnosed and treatment-naïve open-angle glaucoma (OAG) patients at baseline and one month after beginning monotherapy with topical prostaglandin monotherapy. Mean age was 64.63, where 47 eyes were nonprogressing and 16 eyes were progressing according to the event analysis performed by the Humphrey device.
There were no significant differences in IOP, central corneal thickness or Corvis ST parameters between the two groups at baseline. Nevertheless, at one month, the SSI index was 1.60 vs. 1.80 in nonprogressing vs. progressing eyes, respectively. Highest concavity parameters were different between the groups at one month suggesting an increased scleral rigidity in the progressing group. There was no significant difference in IOP between groups at one month.
“These findings are clinically important since the estimated risk for progression can guide clinical decision-making, frequency of monitoring, as well as the threshold for more aggressive treatment,” the researchers wrote in their paper.
“It is expected that those eyes that are less stiff at one month, irrespective of their starting point, are the ones less likely to progress,” they added. “It is also understood that this difference is evident as quickly as one month after starting latanoprost drops, therefore it represents a fast response of the eye to the drug.”
The team also proposed that it is possible that those who reach a low stress-strain index at one month, either because they start from a lower stress-strain index at baseline or because they demonstrate a larger decrease in stress-strain index from baseline due to treatment, are more protected against VF progression.
“Our results provide evidence supporting the clinical relevance of measuring corneal biomechanics and the possible role of these parameters in assessing the risk of progression in newly diagnosed ocular hypertension and POAG,” the study concluded. “In addition, softening the eye wall may as well be proposed as a new glaucoma therapeutic target.”
Martinez-Sánchez MI, Bolívar G, Dastiridou A, et al. Predictive value of dynamic corneal response parameters evaluated with Scheimpflug high-speed video (Corvis ST) on the visual field progression in prostaglandin treated ocular hypertension and open-angle glaucoma patients. Ophthalmol Ther. September 21, 2023. [Epub ahead of print]. |

