 |
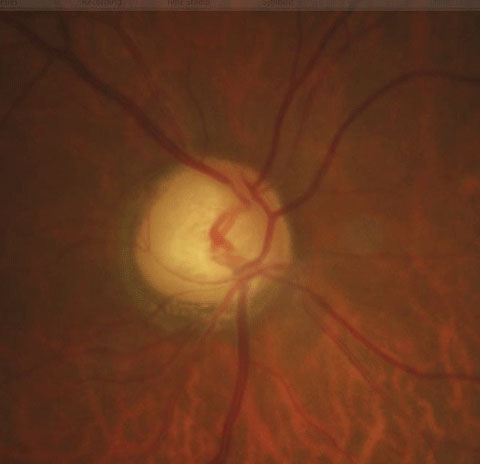
| Though stereoscopic evaluation and OCT are standard techniques when assessing glaucoma, ophthalmic ultrasound may also yield important clues, study finds. Photo: Justin Cole, OD, and Jarett Mazzarella, OD. Click image to enlarge. |
Paying close attention to the optic nerve’s structure is key in diagnosing glaucomatous optic neuropathy and following up with patients, but there’s still some debate about the effectiveness of diagnostic methods on measurement. Standardized A-scan ultrasound’s reliability and validity have been confirmed in previous studies; B-scan ultrasonography and computed tomography or MRI of the optic nerve calculate diameter but don’t always yield standard measurements. Researchers say this may be a possible source of bias and errors in evaluation. They recently evaluated optic nerve pial diameter (ONPD) on standardized A-scan and investigated the relationship between ONPD and structural and vascular changes on SD-OCT and OCT-A. They found that A-scan provided a “reliable and objective examination” of the ONPD and revealed important information about axonal damage.
The team enrolled 126 eyes of 63 primary open-angle glaucoma (POAG) patients and 124 eyes of 62 healthy controls in the prospective study. Each subject underwent A-scan ultrasound to evaluate ONPD and SD-OCT to assess ganglion cell complex (GCC) and retinal nerve fiber layer (RNFL) thickness, as well as optic nerve head (ONH) morphology. OCT-A was used to measure the vessel density of the radial peripapillary capillary plexus.
The researchers reported that ONPD demonstrated a statistically significant reduction in the POAG group compared with controls. POAG patients also showed significant impairment of parameters assessed with both OCT devices compared with controls. Optic nerve analysis of the POAG group showed significantly lower rim area values and increased cup-to-disc ratio and cup volume. The researchers also noted significant correlations between ONPD and radial peripapillary capillary plexus in POAG patients, as well as a significant correlation between ONPD and structural SD-OCT parameters and between ONPD and visual field parameters.
“According to the vascular theory, the optic nerve blood flow damage due to both increased IOP and vascular risk factors (vascular dysregulation, local vasospasm and nocturnal hypotension) could lead to an axonal ischemia,” the researchers wrote in their paper. They noted that this was also demonstrated by reduced radial peripapillary capillary on OCT-A, “determining an impairment of GCC and RNFL thicknesses with consequent ONPD reduction.”
“Since there is a close neurostructural and vascular interconnection between the retina and central nervous system, the use of standardized A-scan ultrasound together with SD-OCT and OCT-A could demonstrate the relationship between anatomical damages of the optic nerve and the neurodegenerative processes involved in glaucoma,” they continued.
They concluded that A-scan ultrasound measurements of ONPD have significant correlation with structural and vascular glaucomatous changes measured on SD-OCT and OCT-A. “These results confirm the diagnostic reliability of the ultrasound evaluation in glaucoma optic neuropathy,” they said. They pointed out that ocular echography is still a valid and “indispensable diagnostic technique” despite new diagnostic methods.
Montorio D, Cennamo G, Breve MA, et al. Correlation between the optic nerve pial diameter and radial peripapillary vascular changes in primary open-angle glaucoma. Graefe’s Arch Clin Exp Ophthalmol. October 21, 2021. [Epub ahead of print]. |

