 History
History
A 45-year-old white male presented complaining of ocular discomfort in the right eye and double vision for the previous seven days.
His systemic history was noncontributory. His ocular history was significant for retinal detachment repair in the right eye eight years ago. Finally, he reported no allergies or recent trauma, and he was not taking any medications.
Diagnostic Data
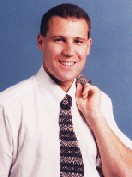
The patients best-corrected visual acuity was 20/20 O.U. at distance and near. An external examination of the individuals right eye demonstrated the findings illustrated in the photograph.
Cover testing produced approximately 10 prism diopters of right hyperdeviation at both distance and near. His pupils appeared normal, without evidence of any afferent defect. All other external testing was normal.

Except for the conjunctival injection seen in the photograph, biomicroscopy revealed normal and healthy anterior segment structures. Intraocular pressures measured 16mm Hg O.U.
The dilated fundus exam revealed healthy optic nerves, vasculature and maculae with attached retinae in both eyes.
Your Diagnosis
How would you approach this case? Does this patient require additional testing? What is your diagnosis? How would you manage this patient? What is the likely prognosis in this case?
Thanks to Jeffry Gerson, O.D., at the
Discussion
The diagnosis in this case is episcleritis secondary to an extruding scleral buckle. Nearly 10 years earlier, the patient had scleral buckling surgery in his right eye for an acute rhegmatogenous retinal detachment. The initial surgery was a success, with complete retinal reattachment and maintenance of good vision.
The extruding buckle interacted with the extraocular muscles to cause intermittent diplopia and episcleral inflammation. The photograph shows the MIRAgel implant, from Mira Inc., perforating through the conjunctiva.
Scleral buckling, or indentation, was pioneered in the early 1950s and still remains a viable procedure for retinal reattachment.1 Although other procedures, such as pneumatic retinopexy and primary vitrectomy, have gained popularity, scleral buckling is still the standard by which the alternatives are judged, thanks to its success rate of nearly 90%.2
The purpose of a scleral buckle is to push, or buckle, the sclera inward, causing contact with the retina. This relieves traction on the retina, and causes the tear to settle and close. But, this operation alone will not cause the tear to seal itself. So, either cryotherapy or laser photocoagulation is performed to create scarring around the tear and prevent future redetachment.
Because the apposition of the RPE to the neurosensory retina causes a change in the hydrodynamics of the vitreous, drainage of subretinal fluid may not be necessary.3 Drainage of subretinal fluid is sometimes required, however, when there is a bullous detachment, and approximation is not obtainable by buckle alone.
Since the encircling pressure of the band essentially elongates the eye, increase in myopia can be a side effect of surgery. Some surgeons may employ vitrectomy to eliminate the RPE traction; this technique requires substantial skill, but it generally produces favorable results.4
Buckling materials are usually either solid silicone rubber bands or sponges. They come in a number of shapes and sizes. The most appropriate buckling material is determined by the location and extent of the retinal break.
The MIRAgel implant was introduced in 1981. Not only is the MIRAgel implant both soft and elastic, but it also has the ability to contain and, upon implantation, to release antibiotics.
But, seven to 11 years after initial surgery, some patients who received MIRAgel implants reported complications.3 Alteration of the materials chemical composition likely causes it to swell over time. At worst, this complication resulted in extrusion of the device.5
Though this complication is uncommon, it is estimated that up to 1% of the implants may extrude and require removal.6 In most cases, however, a secondary infection precipitates the extrusion. Extrusion can be observed by external examination, and confirmed by slit lamp exam.7 Scleral buckles generally need to be removed when there is exposure, infection, motility disturbance, or intrusion. Depending on the circumstances surrounding the dissection and surgical procedure, removal of a scleral buckle carries a rate of redetachment ranging from 4% to 23%.2,7
Patients that have an extruding implant accompanied with a secondary infection run a greater risk of redetachment than those that suffer an extrusion alone.6,7 Patients with a history of smaller initial detachments and less vitreous traction have a reduced risk of complication.7
Promptly refer the patient to a retinal specialist for evaluation of removal. Topical antibiotics, lubricants and cold compresses can be used to provide prophylaxis and comfort. In severe cases, consider cycloplegia and oral analgesics. Since surgical removal is likely, avoid topical steroidal and nonsteroidal preparations.
1. Schepens CL, Okamura ID, Brochhurst RJ, et al. Scleral buckling procedures. V. Synthetic sutures and silicone implants. Arch Ophth 1960 Dec;64:868-881.
2. Schwartz SG, Kuhl DP, McPherson AR et al. Twenty-year follow-up for scleral buckling. Arch Ophthal 2002;120:325-329.
3. Kearney JJ, Lahey JM, Borirakchanyavat S et al. Complications of hydrogel explants used in scleral buckling surgery. Am J Ophthal 2004 Jan;137(1):96-100.
4. Martinez-Castillo V, Zapata MA, Boixadera A, et al. Pars plana vitrectomy, laser retinopexy, and aqueous tamponade for pseudophakic rhegmatogenous retinal detachment. Ophthalmology 2007 Feb;114(2):297-302. Epub 2006 Oct 23.
5. Le Rouic JF, Bettembourg O, DHermies F, et al. Late swelling and removal of Miragel buckles: a comparison with silicone indentations. Retina 2003 Oct;23(5):641-46.
6. Roldan-Pallares M,
7. Shields CL, Demirce H, Marr BP, et al. Expanding MIRAgel scleral buckle simulating an orbital tumor in four cases. Ophthal Plas Reconstr Surg 2005 Jan;21(1):32-8.

