 |
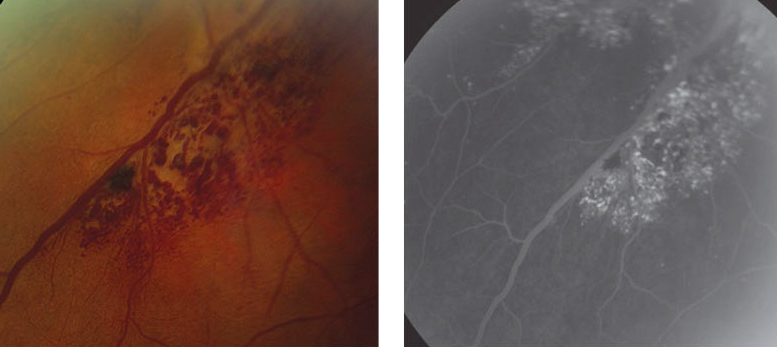
| Retinal venous malformations like this cavernous hemangioma, if presenting concurrently with neuro-ophthalmic abnormalities, may warrant neuroimaging, study says. Photo: Mark Dunbar, OD. Click image to enlarge. |
Sharing common developmental and signaling pathways, the brain and retinal vasculature are connected in a way that makes them susceptible to conditions of one structure impacting the other. An area of recent interest has been the question of whether retinal venous malformations (RVMs) are associated with cerebral vascular malformations (CVMs), as one previous study has suggested.
A new study’s researchers wanted to determine the prevalence of RVMs in patients with high-risk CVMs. To do so, patients diagnosed with cerebral cavernous or arteriovenous malformations were retrospectively reviewed who were evaluated by the ophthalmology service at Northwestern University.
Patients were divided into three categories by level of certainty: (1) dilated funduscopic examination (DFE), (2) fundus exam with any type of ocular imaging and (3) DFE with complete macular imaging. Recorded were ophthalmic exam abnormalities, ocular image findings and major CVM complications. Of the 156 patients included who underwent DFE, ocular imaging was performed on 56 patients and of those, 46 received complete macula imaging. No RVMs were seen for any group; however, cerebral hemorrhage or seizure occurred in 15% to 33% of patients and visual field defects or cranial nerve palsies occurred in 14% to 20% of patients.
Due to the common neuro-ophthalmic findings, the study authors recommend “neuroimaging for patients with RVMs and neuro-ophthalmic signs or symptoms,” they wrote in their paper for Journal of Neuro-Ophthalmology.
The authors discuss how their findings weaken the findings of the previous study by Pichi et al, which found RVM patients to have a 24% CVM prevalence. They explain that the difference here may lie in the MRIs obtained by the previous study, which were collected for indications besides RVM, so symptom presentation may have been a confounder for CVM presence.
They further elaborate that if there is a pathophysiological origin between the two conditions, RVM detection would be expected in CVM patients. An example of this is with phakomatoses, which show high association between retinal and cerebral findings, as with von Hippel-Lindau syndrome and Wyburn-Mason syndrome.
Reflecting on the high rate of neuro-ophthalmic findings but low RVM rate in high-risk CMV patients, the authors proposed an algorithm for treating patients diagnosed with RVM.
First, “if a patient with an RVM has any neurologic symptoms or abnormalities on their neuro-ophthalmic examination, neuroimaging is indicated to rule out CMV.” Patients aged 40 or younger are recommended neuroimaging “because it will provide the greatest benefit-to-cost ratio for these younger patients with RVMs, given their remaining life expectancy.”
For the middle bracket of patients—those aged 40 to 70—with RVMs, the authors recommend shared decision-making between the relevant eye doctor and their patient.
Finally, patients over 70 with RVMs are not indicated to undergo neuroimaging, since its highly likely that a high-risk CVM would have already been detected.
To distinguish affected young patients, the authors propose “MRI brain with and without contrast, including susceptibility-weighted imaging sequence and MR angiogram to detect high-risk CVMs in young patients with RVMs.”
Chan KS, Daulton MR, Reddy VD, McComb EN, Lavine JA. Prevalence of retinal venous malformations in patients with cerebral cavernous or arteriovenous malformations. J Neuro-Ophthalmol. August 16, 2023. [Epub ahead of print]. |

