 |
A 62-year-old Caucasian male with a 15-year history of bilateral glaucoma presented as a new patient having just moved to the area. His last visit to his previous eye doctor was approximately nine months earlier, at which time he was apparently told that everything was stable and to make sure he was seen by a glaucoma doctor once he settled.
His chief complaints were chronic and progressively worsening red eyes, the left moreso than the right, which tended to worsen as the day went on. He reported this was a long-term issue and felt as though his symptoms were aggravated after he administered his glaucoma medications. He reported good compliance with his medications.
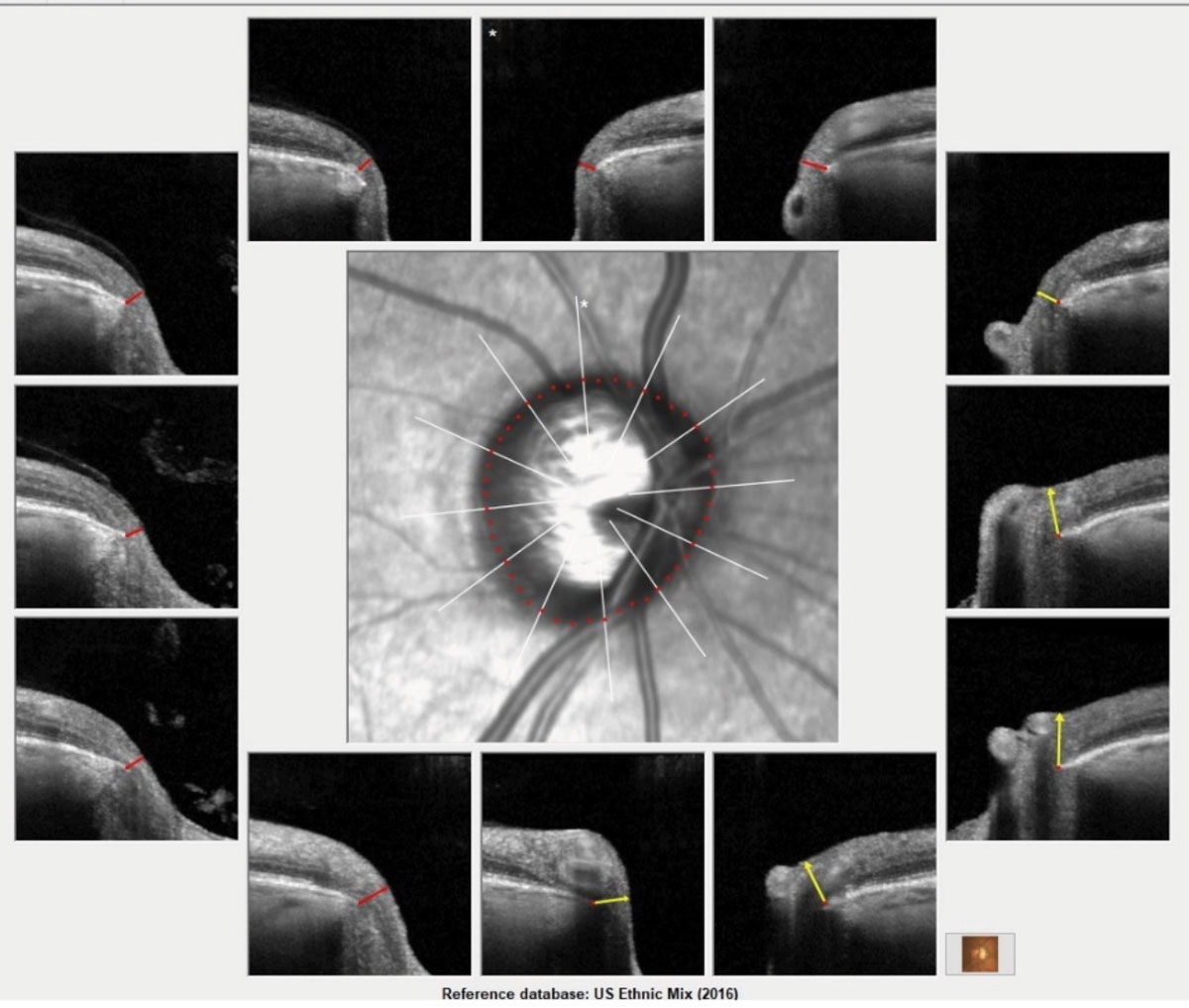 |
| Bruch’s membrane opening overview image of the patient’s right eye. Note the thinned neuroretinal rim OD from 6 o’clock to 12 o’clock, consistent with moderately advanced glaucoma. Click to enlarge. |
Examination
At this visit, his glaucoma medications included: brimonidine 0.2% QAM OU, Alphagan P (brimonidine tartrate, Allergan) QD mid-day OU, 1% pilocarpine HS OU and generic latanaprost HS OU. His systemic medications included atorvastatin 20mg QOD, bupropion 100mg QD, gabapentin 300mg BID and Proventil (albuterol, Merck) PRN. He reported no allergies to medications. Significant in his ophthalmic history were two laser treatments to his right eye approximately six years ago and one session to his left eye at about the same time. He reported the laser surgery was for his glaucoma.
He also reported previously trying a series of different glaucoma medications, in an attempt to better control his IOP and minimize the irritation that most of his glaucoma medications caused. Most important was his recollection that he did not tolerate Lumigan (bimatoprost, Allergan) and also had significant issues with dorzolamide on a TID basis, as well as Simbrinza (brinzolamide/brimonidine tartrate, Novartis).
Systemically, he had mild chronic obstructive pulmonary disease (COPD), recurring migraines and hypercholesterolemia. Entering uncorrected visual acuities were 20/20 OD and 20/20 OS. Minimal hyperopic presbyopic refractive error was found upon refraction and was correctable to 20/20 OD, OS, OU.
A slit lamp exam revealed moderate conjunctival and episcleral hyperemia in both eyes. We also noted concurrent mild conjunctival chemosis and fine papillae on the palpebral conjunctiva OU. Angles were wide open on slit lamp estimation. Applanation tensions were 28mm Hg OD and OS at 4:20pm. Pachymetry was 555µm OD and 561µm OS.
The patient was dilated, and his crystalline lenses were clear. Stereoscopic examination of his optic nerves was remarkable for cup-to-disc ratios of 0.8x0.85 OD and 0.65x0.65 OS. The neuroretinal rim temporally of the right eye was quite thin and eroded. The left was also thin, with a well-perfused remaining rim.
His macular evaluations were essentially unremarkable, with lack of foveal reflexes bilaterally, and fine retinal pigment epithelium granulation consistent with his age. The retinal vasculature was characterized by mild arteriolarsclerotic retinopathy, consistent with his history of hypercholesterolemia. His peripheral retinal exams were unremarkable.
While he was dilated, we took the opportunity to obtain stereo optic nerve images.
At this point, it was clear that two important items needed attention. First, as the patient relayed in his history, he has been bothered with irritated eyes for several years, which can certainly be exacerbated by the glaucoma medications. Secondly, he has moderately advanced glaucoma OD>OS, and I was not convinced that IOPs of 28mm Hg were an adequate target IOP. So, we determined that we needed to obtain better IOP control and better patient comfort.
Treatment
I didn’t immediately replace all his glaucoma medications. That might send the message that I have no faith in his previous doctor, who I don’t know, but who the patient has trusted for many years. Also, he presented with a history of having tried many medications and having various reactions to them, so trying something new can be a shot in the dark insofar as selecting one that won’t cause problems; it seems as though most do cause him problems. At this stage of the disease, we need to be careful not to let the IOP get further out of control while we hunt for that perfect combination of therapies. And lastly, his eyes are already chronically inflamed and introducing any new is not likely to diminish those symptoms. For these reasons, my management plan in cases such as these is to take things slowly. When only one thing at a time is changed, it’s easier to see the effects.
There were a couple of interesting things about his current medication regimen, including the use of pilocarpine as well as two forms of brimonidine.
I chose to have him discontinue the generic brimonidine, increase the Alphagan P to BID, continue the pilocarpine and continue the latanaprost. From a glaucoma medication perspective, the only thing I did was to get him off the higher concentration of brimonidine and substitute that for an additional dose of Alphagan P. But I also chose to help facilitate reduction of his inflammation, and hopefully reduction of his symptoms, by adding a steroid. My go-to steroid in cases like this is fluorometholone because it is a potent anti-inflammatory agent, but one that does not penetrate well into the anterior chamber, reducing the likelihood of an IOP increase. The steroid was prescribed BID for two weeks. The patient was asked to return in a month for threshold field testing, gonioscopy, Heidelberg retinal tomography (HRT 3, Heidelberg) and OCT imaging of both optic nerves and macular ganglion cells.
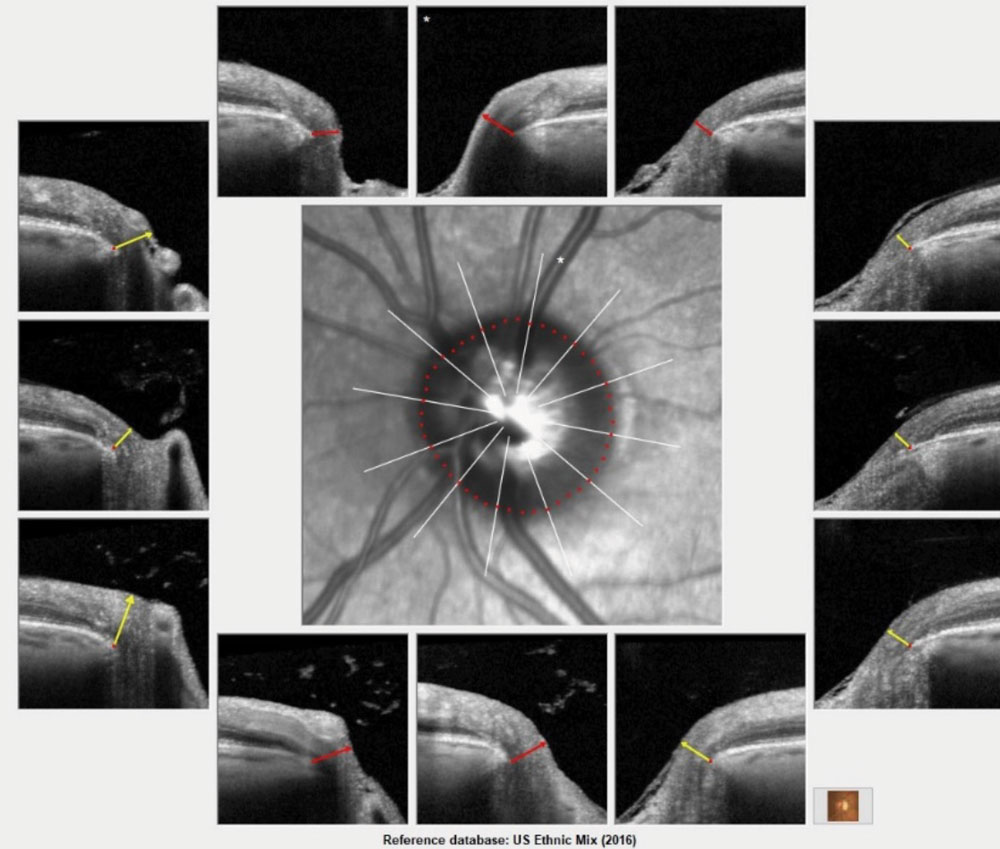 |
Bruch’s membrane opening overview of the patient’s left eye demonstrating moderate glaucomatous optic neuropathy. Click to enlarge. |
Follow Up
The patient complied and returned as requested. At this visit, he reported mild reduction in his irritation while on the steroid, but a gradual increase since its cessation. IOPs at this visit were 37mm Hg OD and 33mm Hg OS. We began the slow process of altering glaucoma medications and walking a fine line with topical steroids to reduce inflammation.
Of course, also on the table is surgical intervention. But keep in mind the patient already underwent SLT twice in his right eye and once more for his left. iStent inject (Glaukos) would offer some IOP reduction, but the patient had clear natural lenses, and currently the implantation of iStent inject devices is limited to implantation during cataract surgery. Surgical intervention with tube, shunt or trabeculectomy is also an option, but one I would reserve if absolutely necessary.
At the completion of this visit, I asked him to restart the flurometholone BID and hold at that dosage until the next visit, decrease the Alphagan P to QD, and add Vyzulta (latanoprostene bunod, Bausch + Lomb) to the regimen. While he was still taking the latanaprost, the Vyzulta gives an additional mechanism of IOP reduction beyond the uveoscleral outflow of other prostaglandins.
My choice in doing this was rather simple; I wanted to see how much of an IOP decrease we would obtain, if any, with the addition of the Vyzulta, knowing full well that his IOPs are now higher than they were before he was put on a steroid. To complicate things further, I was asking him to continue with the steroid for the next few weeks.
Imaging of the nerve and macula correlated to the clinical findings of more advanced disease in the right eye and the visual fields matched the clinical and imaging findings with an arcuate defect noted.
At a subsequent visit, IOPs were 15mm Hg OD and 12mm Hg OS, but he reported that his eyes did not feel much better. While we are making progress on IOP reduction, we are not yet making progress on the discomfort. The addition of the Vyzulta gave us a significant reduction in IOP, which in turn clears the way for further reduction in his other glaucoma medications. Most likely, the biggest contributor to the irritation he’s been experiencing is the brimonidine, though the pilocarpine probably also plays a role. Since he was down to using the Alphagan P only once daily, the next logical step was to discontinue it while maintaining all his other medications. He did this and, in a follow up one month later, reported significant improvement in symptoms. His IOPs at this visit were 16mm Hg OD and 14mm Hg OS. We were finally seeing the light at the end of the tunnel.
As you can imagine, the plan now was to ultimately wean off the steroid, but also with the possibility of eliminating the pilocarpine. So, true to form, I chose to only change one thing at this visit: eliminate the pilocarpine.
Six weeks later, the patient reported continued reduction in irritation. Clinically, the papillae were greatly reduced, as was the episcleral hyperemia OU. IOPs were 16mm Hg OD and 18mm Hg OS. He was only taking the Vyzulta HS OU and the flurometholone BID OU. The patient was asked to slowly taper off the steroid, using it in both eyes QD for one month then QOD for another month before discontinuing. He was asked to return in four months. He did so and by that visit, he was only taking the Vyzulta. His IOPs were 14mm Hg OD and 15mm Hg OS, and his eyes were clear, white and asymptomatic.
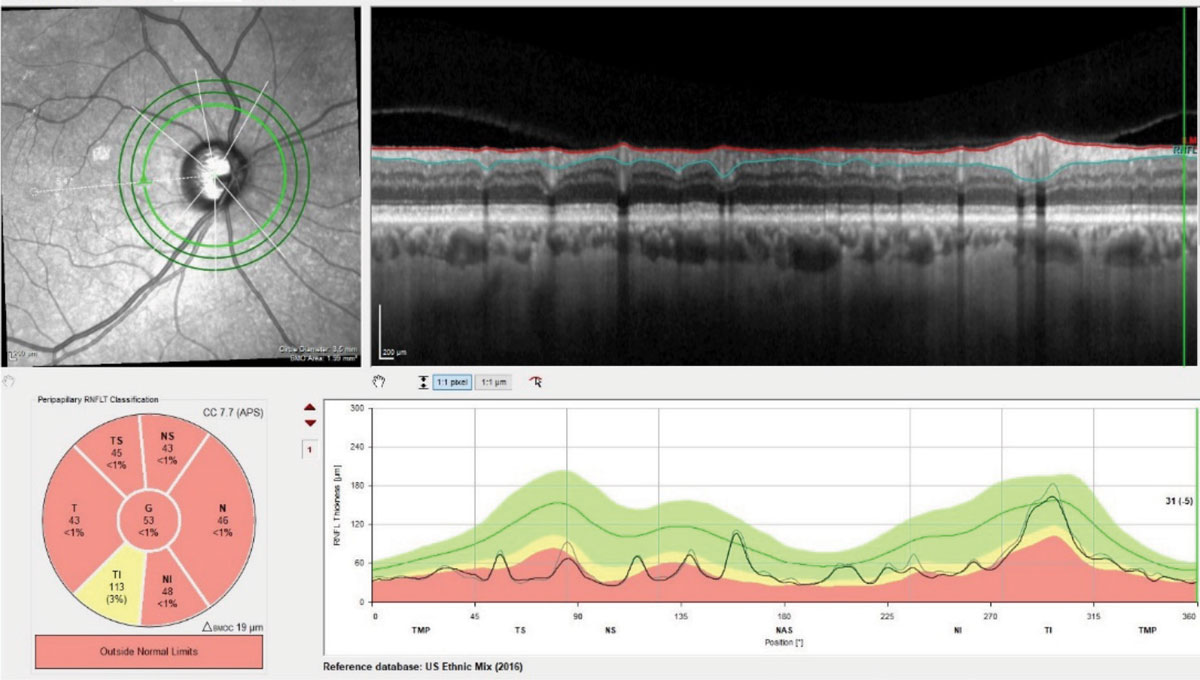 |
| Three RNFL diameter circle scans of the patient’s right eye. Note the stability of the innermost RNFL circle scan of the most recent visit compared with the baseline visit obtained 18 months earlier. Where there is a difference between the scans, the thickness differences overlay major perioptic retinal blood vessels. Click to enlarge. |
Slow and Steady
When sorting through a case like this, where better IOP control and better ocular comfort are needed, take it slowly. Begin changing things, but do it one step at a time. This way you can see the effects of that one change. By doing so, it makes your treatment path much clearer. While it may take longer to do it this way, it’s easier to formulate a plan. Your initial reaction may be to clean house, but sometimes doing that too abruptly leads to confusion as to how to proceed, loss of confidence in you as the doctor and, worst of all, further damage to the patient’s eyes. Ultimately, we cleaned house, but we did it in an organized and methodical fashion.

