 Q. What are most clinicians doing today to assess the cornea for contraindications (such as loss of rotational symmetry and corneal thinning) prior to recommending refractive surgery? Are there any circumstances where you might recommend surgery in a person older than 30 who has signs of mild (forme fruste) keratoconus?
Q. What are most clinicians doing today to assess the cornea for contraindications (such as loss of rotational symmetry and corneal thinning) prior to recommending refractive surgery? Are there any circumstances where you might recommend surgery in a person older than 30 who has signs of mild (forme fruste) keratoconus?
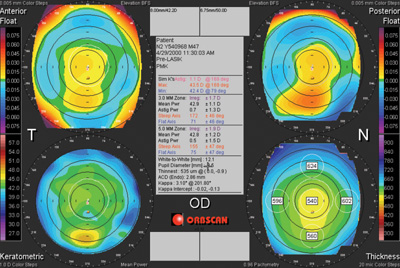
A. Some corneas are better suited for refractive surgery than others. The first step in determining whether a patient is a good candidate for the procedure is a thorough review of corneal topography. Corneal topography can be used to predict one of the most serious, yet rare, complications of refractive surgery: corneal ectasia.
“The most significant risk factor for ectasia is an irregular topography,” says Eric Donnenfeld, MD, who practices in Long Island, NY. “Preoperative topography is the standard of care in all LASIK and PRK surgeries and, as in the past, direct visualization of the topography looking for skew deviation provides very valuable information.”
“Now, however, software evaluates the topography, and can combine information from the posterior corneal surface and pachymetry to warn clinicians about risk factors for keratoconus,” adds Dr. Donnenfeld. “I particularly look at the pachymetric maps on the Pentacam or Orbscan, looking for the pachymetry distribution.”
 |
|
| This patient exhibited forme fruste keratocomus on Orbscan (Bausch + Lomb).
|
“Based upon these retrospective studies, a number of factors have been recognized to increase the risk for developing post-refractive ectasia, including higher degrees of myopia, preoperative corneal curvature over 47D, preoperative central corneal thickness (CCT) of less than 500μm, residual stromal bed thickness less than 250μm, abnormal or asymmetric topographic patterns or patients under 25 years,” explains Dr. Qazi.
It is imperative to know when surgery should be avoided. Pay special attention to corneal thickness before suggesting refractive surgery. “In normal eyes, the cornea is thinnest centrally and thickens symmetrically to the periphery,” says Dr. Donnenfeld. “When the thinnest point on the cornea is inferiorally/nasally displaced, this sends up a red flag that the patient may be at risk. In patients with irregular corneas in which I am able to obtain a quality wavefront aberrometry, I have a detailed and documented conversation with the patients, and will often suggest a wavefront PRK with concomitant riboflavin UV crosslinking.”
“In the past, the recommendation for cases of forme fruste keratoconus was to avoid refractive surgery, as even cases with surface ablation have been reported to develop late-onset ectasia,” says Dr. Qazi. “An additional screening tool to assist in this decision can be application of devices (i.e., Ocular Response Analyzer, Reichert or Corvis ST, Oculus) that measure the biomechanical response of the cornea to an external air pulse stimulus.”
“If there are irregularities in corneal indentation, then keratorefractive surgery, including surface ablation, should be avoided,” he adds. “Collagen crosslinking has been combined with photorefractive ablation in known cases of keratoconus, and thus can be considered as a prophylactic measure in forme fruste keratoconus as well.”

