Contact Lens Close-upThe August issue of Review of Optometry is our 47th annual contact lens report, where we help you use new and old techniques to improve your fitting skills. |
The standard approach to contact lens correction of irregular astigmatism today and for the foreseeable future is to prescribe a non-flexing rigid gas permeable (GP) lens design, whether that be a corneal contact lens, scleral lens, hybrid lens or piggyback system. However, these lens designs do not work in all cases, either due to poor physical fit or comfort or various other reasons. Perhaps, the patient or practitioner is not satisfied with their performance, finds the lenses inconvenient, their size intimidating or application and removal challenging. Custom soft contact lens designs can serve as a viable alternative for these cases. Learn how and when to prioritize these lenses as an option when fitting patients.
Anticipate Keratoconus
The potential sources of irregular astigmatism are injury, surgery and disease. Of course, one of the more common corneal conditions that can lead to irregular astigmatism is keratoconus. Early in the condition, patients are often frustrated with spectacle lenses and standard mass-market soft lenses that do not provide adequate visual acuity. However, these patients are often fairly functional and not overly motivated to try traditional specialty lenses such as corneal GP and scleral lenses. This can be a great time to consider custom soft lenses to provide improvement in visual acuity since these lenses often center well, provide limited movement and offer stable visual acuity and adequate comfort.
 |
|
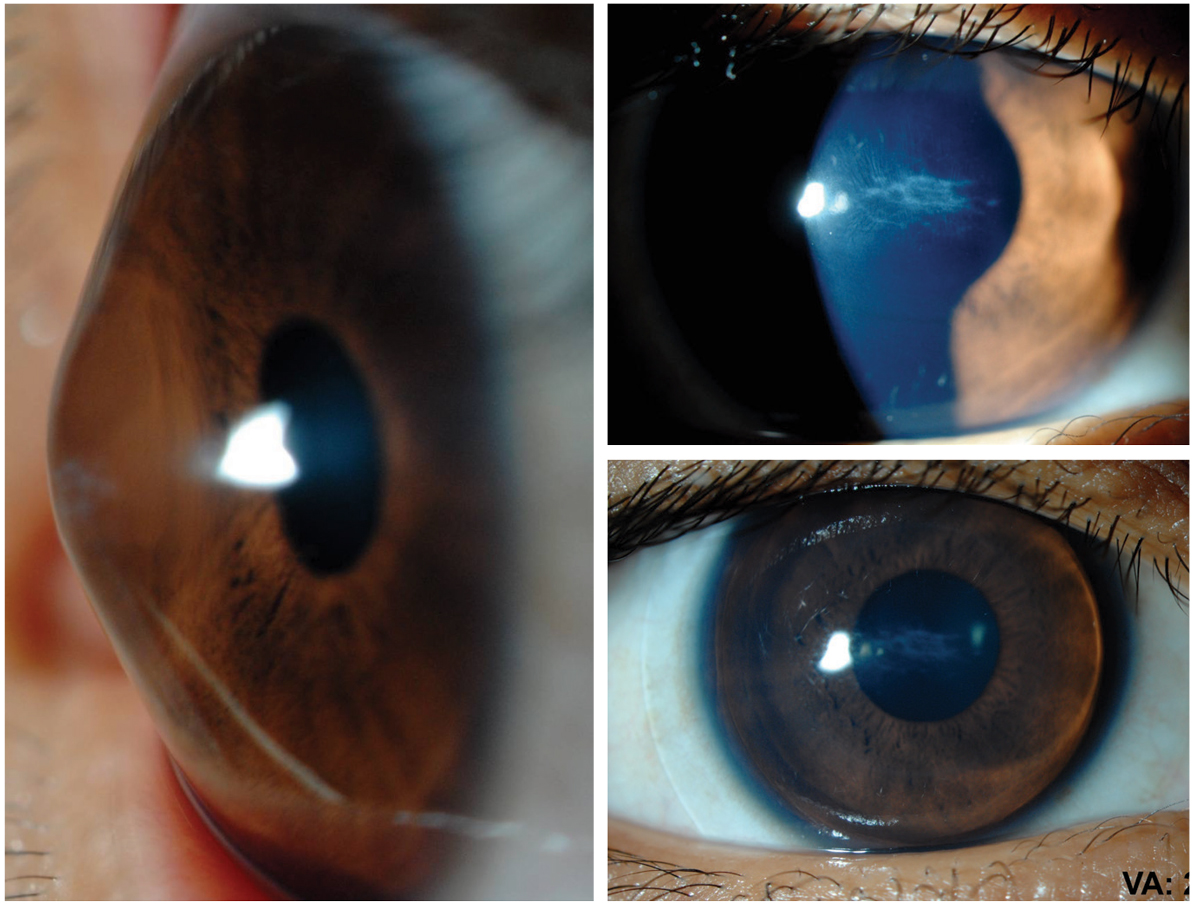
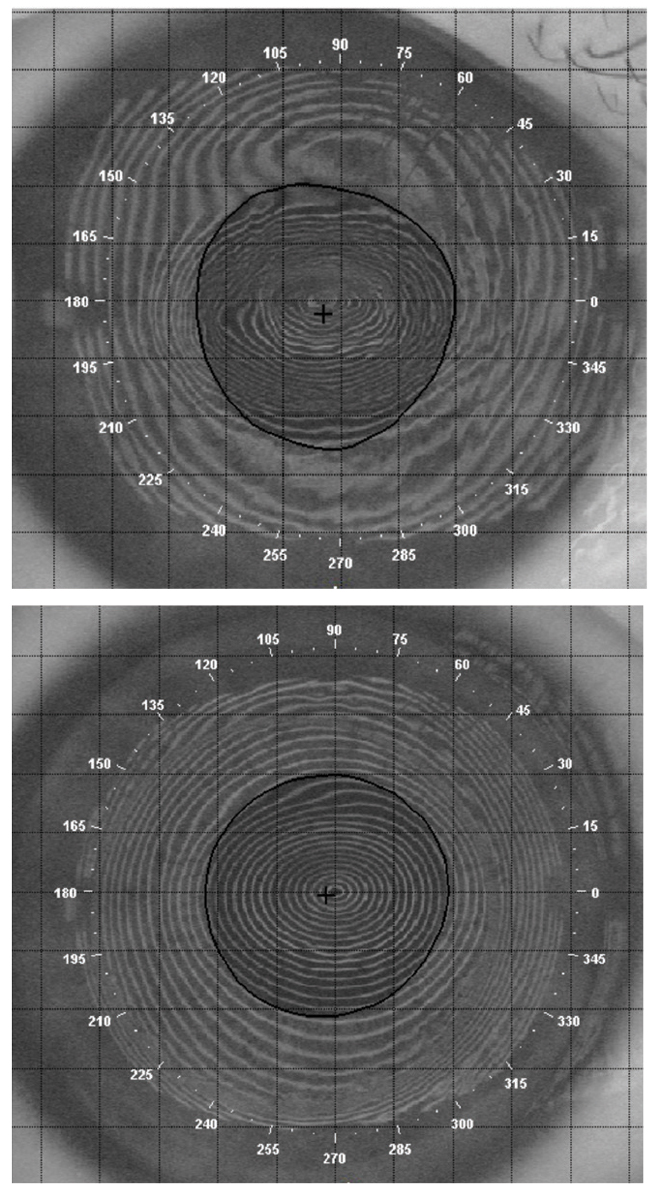
Figs. 1 and 2. A custom soft lens may allow for a stable fit and significant improvement in patient comfort for an individual who has failed with other options. Click image to enlarge. |
If keratoconus progresses, it leads to higher and higher amounts of corneal irregularity. As the cornea is further disrupted by this irregularity increasing, a corneal scar may result and limit best-corrected visual acuity regardless of the contact lens design chosen. In these more advanced stages, the central corneal curvature may steepen to the point that designing a corneal rigid contact lens may be too challenging and the forgiveness of fit that a soft lens provides may be warranted.
In the case of severe keratoconus, a custom soft lens may provide the same level of vision as a corneal GP or scleral lens has, as the patient’s vision is more limited by the corneal scar than the irregularity. This may allow for a stable fit and significant improvement in comfort (Figures 1 and 2). Another benefit to providing a custom soft lens to a patient with severe keratoconus who has failed in other lens modalities is that this option may help that person avoid or delay corneal transplantation.
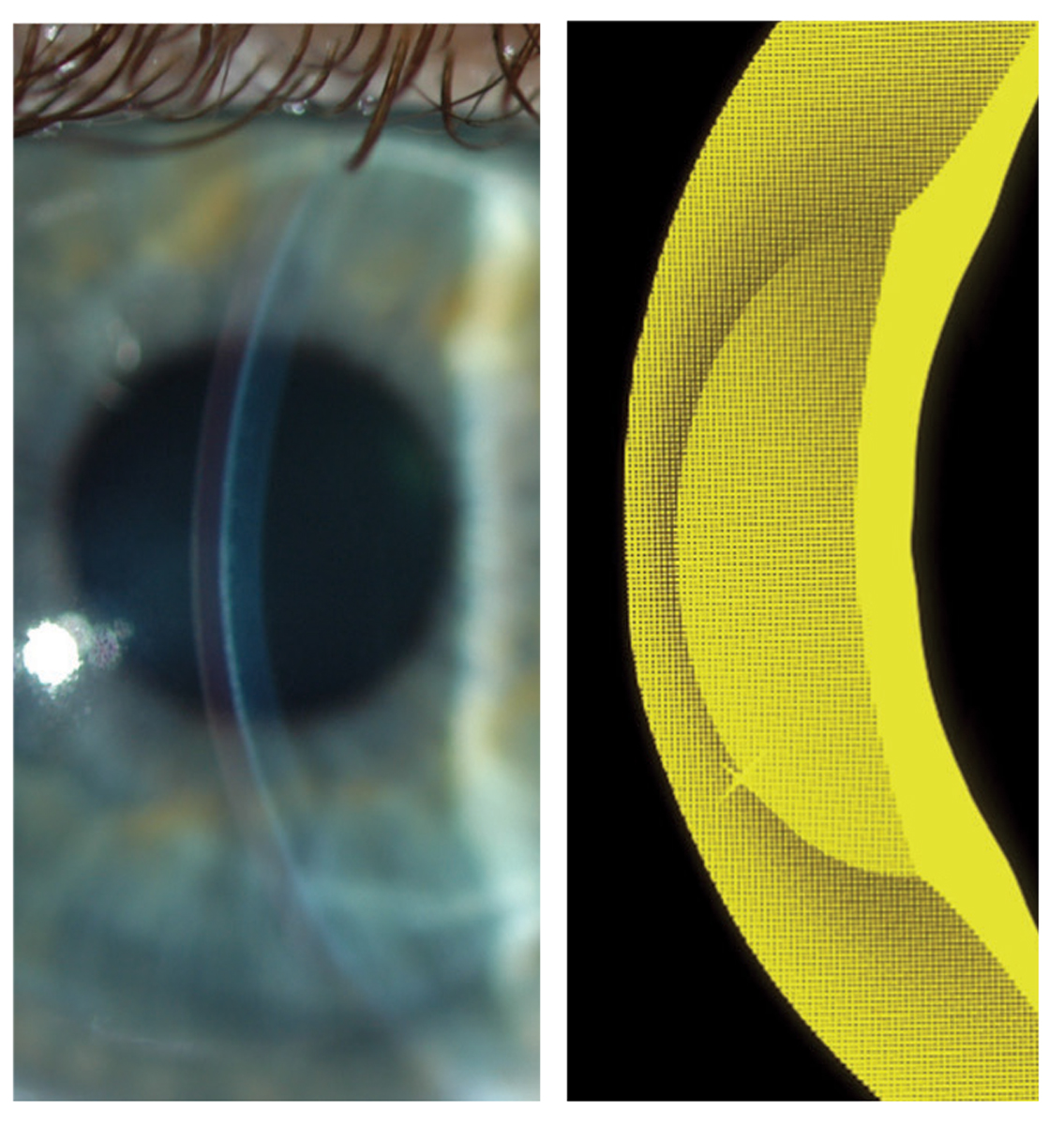
What has been covered here so far related to keratoconus are options and rationale for the patient with mild and severe forms of keratoconus as it relates to custom soft lenses and the decision-making around them. Patients in the moderate category may still benefit from these lenses as evidenced by a case discussed here where the patient presented with keratoconus with 12.00D of irregular corneal toricity over their visual axis. After a thickened custom soft lens was placed on the eye, the corneal distortion was dramatically decreased along with the amount of astigmatism from 12.00D to 5.00D, and the contact lens provided the patient 20/20 visual acuity (Figures 3 and 4).
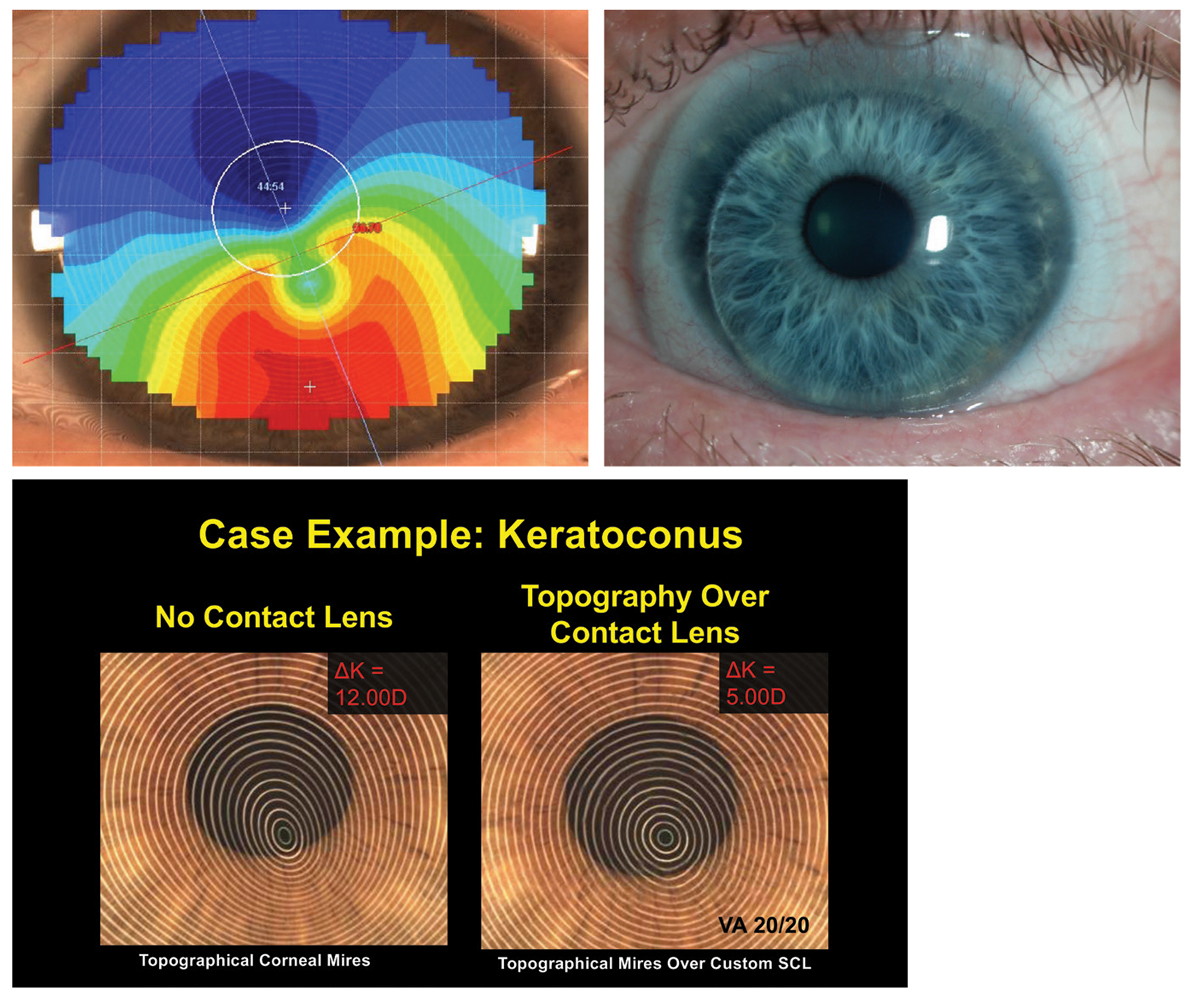 |
| Figs. 3 and 4. Note the thickened custom soft lens that has decreased the corneal distortion in this patient with irregular corneal toricity over the visual axis. Click image to enlarge. |
The Right Choice
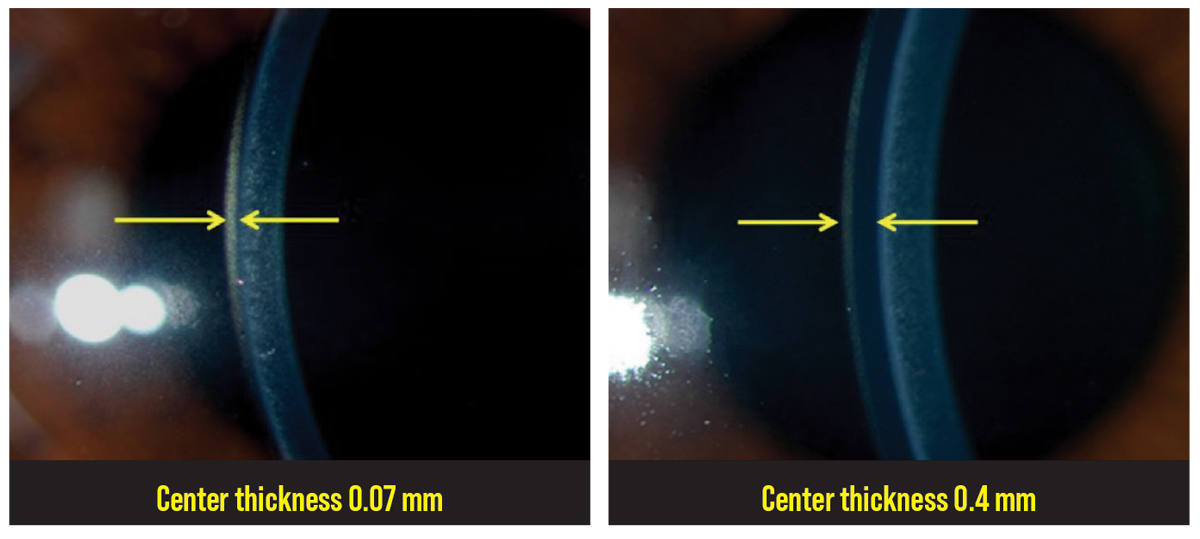
Custom soft lenses are able to be used in patients who have irregular astigmatism due to the increased central thickness of the lens. As the contact lens thickness is increased over the area of the optic zone, it begins to approach the non-flexing nature of GP lens material. However, this does not eliminate the irregular astigmatism like a GP material does. Instead, it converts irregular astigmatism to be more regular in nature, and the necessary toric lens power can be placed on the front surface of the contact lens to optimize the patient’s vision (Figures 5 to 7).
The effect of masking the irregular astigmatism begins around 0.2mm, and if there needs to be more irregular astigmatism–correcting ability, the lens can be additionally thickened from 0.2mm to 0.3mm and then from 0.3mm to 0.4mm and so on. To understand how much irregular astigmatism correction the custom soft lens is providing, perform keratometry (either manually or via corneal topography) over the top of the contact lens and analyze the mires reflecting back. If significant amounts of irregularity are present, increasing the central thickness may be warranted.
 |
|
Fig. 5. Custom soft lenses can be used in patients who have irregular astigmatism due to the increased central thickness of the lens. Click image to enlarge. |
Clinical experience has shown that the maximum irregular astigmatism–correcting ability is reached at a center thickness of 0.5mm, as the soft lens does not seem to be able to mask additional amounts of irregularity beyond 0.5mm. The industry standard central thickness of a soft lens designed for irregular astigmatism is 0.4mm. Of note, this increased thickness is just in the area over the central optic zone and does not extend over the carrier/haptic portion of the contact lens (Figure 8).
Lens Design in Keratoconus
Custom soft lenses for keratoconus early in the condition may be designed with similar or nearly identical base curves and diameters to those used in standard soft lenses; however, as the disease progresses and the cornea steepens, an alternate lens design may be needed. These custom soft lenses specific for keratoconus are designed with a two-part construction: one part with the central base curvature and the second part being the fitting curve that is sometimes referred to as the peripheral haptic or supportive portion of the contact lens (Figure 9).
The central base curve is determined by first assessing the patients central keratometry (K) values, determining an average K by adding the flat and steep K together and dividing that by two. Then, convert the mean K number from diopters to millimeters and add a fit factor of 1.0mm to arrive at the initial recommended base curve value.
Example: Step 1—Central Ks 55.00D @ 084 / 61.50D @174. Step 2—Mean K (55.00 + 61.50 = 116.5) ÷ 2 = 58.25 D. Step 2 Convert diopters to millimeters radius of curvature = 5.79mm. Step 3—Add fit factor of 1.0mm: 5.8mm + 1.0mm = 6.8mm.
Initial recommended central base curve to be ordered: 6.8mm. The fitting curve is ordered with a more traditional soft lens curve value, e.g., 8.3mm or 8.6mm. As these lenses are often ordered with toric powers, the recommended overall diameters ordered are between 14.0mm to 14.5mm.
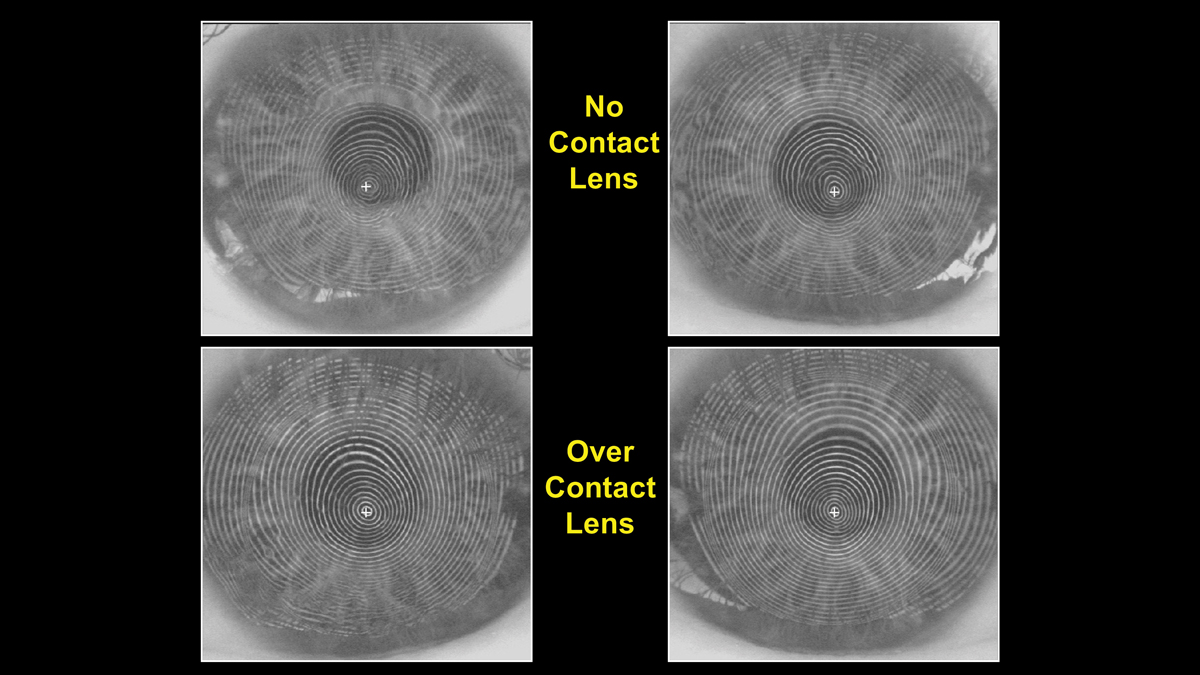 |
Fig. 6. Videokeratoscopy helps demonstrate how custom soft lenses can be used for irregular astigmatism. Click image to enlarge. |
 |
| Fig. 7. The thickened contact lens, as seen with topography, converts irregular astigmatism to be more regular in nature, and the necessary toric lens power can be placed on the front surface of the contact lens to optimize the patient’s vision. Click image to enlarge. |
Other Possible Hurdles
Another corneal ectasia similar to keratoconus is pellucid marginal degeneration. With this condition, the ectasia is often near the inferior limbus. This results in the inferior cornea migrating forward, creating a significant elevation to that region as well as high amounts of against-the-rule astigmatism within the central cornea. The significant corneal elevation inferiorly creates a challenging environment for a corneal GP to be supported by the cornea itself due to the amount of asymmetry present.
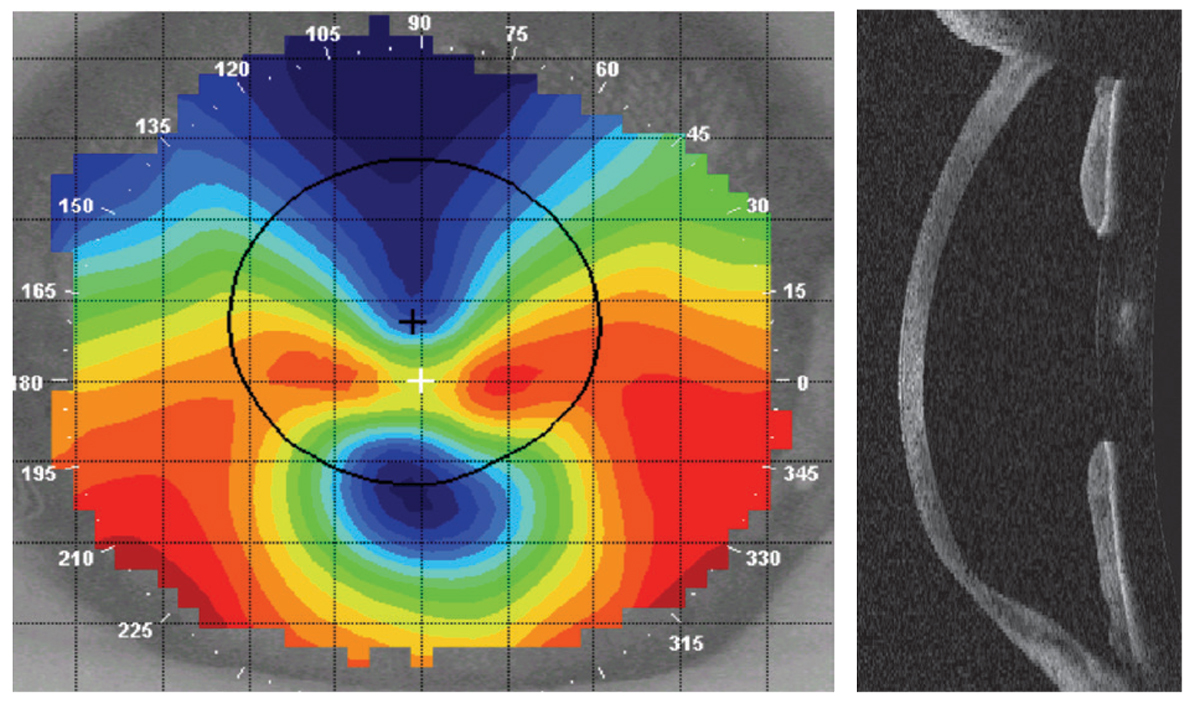
Thankfully, though the amount of against-the-rule astigmatism present in the central cornea is high, it is often fairly regular over the pupil and visual axis as demonstrated by the axial display of the corneal topographer (Figure 10). This sets up a scenario where custom soft lenses may be employed to correct the high amount of astigmatism, mask some of the irregularity with an increase in central lens thickness and provide enough steepness and depth to cover the ectasia.
Other sources of irregular astigmatism are corneal injury and surgery. The amount of irregularity these events can cause varies widely. If the injury or surgery is unilateral and results in irregularity that is not able to be successfully managed with standard spectacles and soft contact lenses, a custom soft lens may be an excellent choice as the other contact lens options such as corneal GP lenses, scleral lens, hybrids and piggyback systems may not be tolerated by the patient in one eye alone. A custom soft contact lens may offer the patient the comfort and stability they need to adapt to wearing a contact lens unilaterally.
If the patient has undergone previous myopic refractive surgery, the central cornea is relatively flatter and lower in height than the surrounding steeper midperipheral cornea. This oblate shape is just the opposite of the normal prolate profile of the human cornea. The standard off-the-shelf soft lens mimics the normal cornea by having a prolate shape. If these lenses are used in the post-myopic refractive surgery cornea, the lens will often vault in the center and provide variable vision with each blink. Custom soft lenses, however, can be ordered with reverse geometry to better align the post-myopic refractive surgery cornea and not provide the excessive central clearance standard that off-the-shelf lenses do and provide clearer and more consistent vision instead. These lenses have a similar two-part construction to their back surface like lenses for keratoconus; however, instead of being designed steeply in the center, the lens is significantly flatter centrally than peripherally.
The central base curve is designed by first identifying the flat K, then converting from diopters to millimeters radius of curvature and then adding an additional fit factor of 0.4mm to arrive at the initial recommended base curve radius.
Example: Step 1—central flat K 37.25D. Step 2—convert diopters to millimeters radius of curvature = 9.05mm. Step 3—add fit factor of 0.4mm: 9.05mm + 0.4mm = 9.4mm base curve.
The surrounding fitting curve is selected of some normal value (example: 8.3mm or 8.6mm), as this portion of the ocular surface is not altered by the history of refractive surgery.
 |
|
Fig. 8. The maximum irregular astigmatism correcting ability is reached at a center thickness of 0.5mm, which is over the central optic zone and does not extend over the carrier/haptic portion of the lens. Click image to enlarge. |
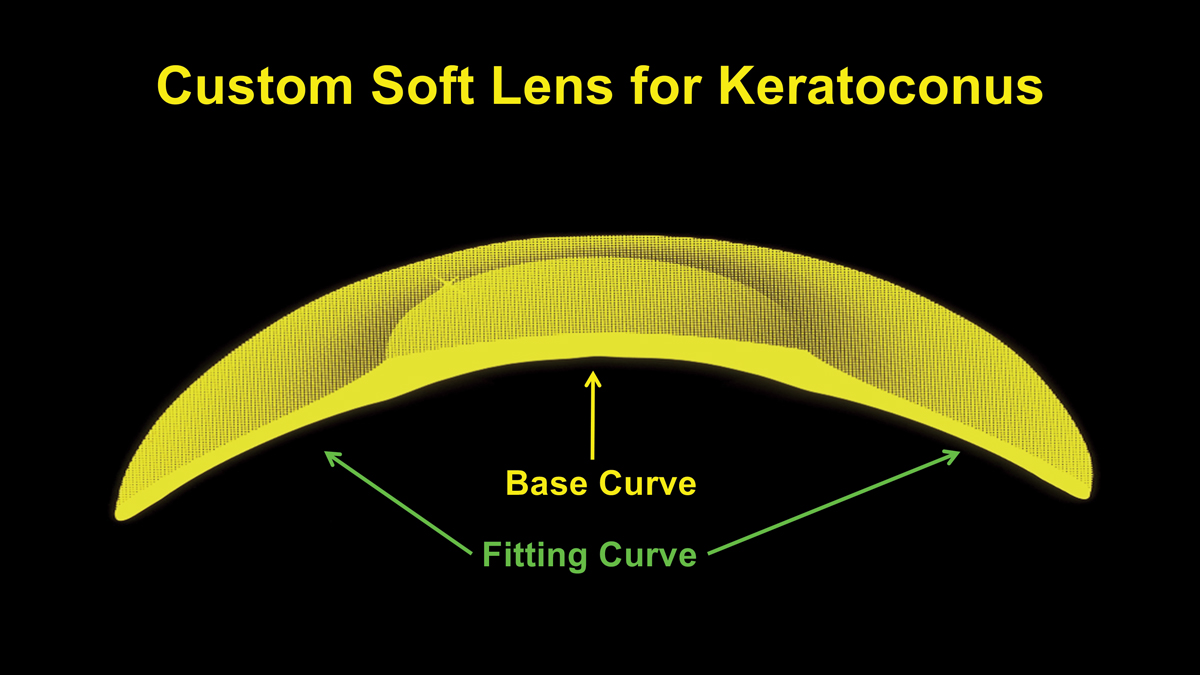 |
Fig. 9. The central base curve and the fitting curve make up the design of a custom soft lens for keratoconus. Click image to enlarge. |
Lens Care and Handling
Due to the custom nature of soft lenses for irregular astigmatism, the recommended replacement schedule is often quarterly and open-eye daily wear only. As these lenses need to last longer than their traditional off-the-shelf counterparts, care and handling and recommended lens care products are of critical importance.
The impact of nightly rubbing and rinsing with the recommended lens care product can aid in the process of keeping the lens free of significant deposition. Either multipurpose or peroxide systems can be used with these customs soft lenses. When a patient asks what the ideal lens care products are to use with a specific custom soft lens, the consultation department at the manufacturer can provide its recommendations around the specific soft lens material and design.
 |
|
Fig. 10. A corneal topographer helps demonstrate that, though the amount of against the rule astigmatism present in the central cornea is high in a patient with pellucid marginal degeneration, it is often regular over the pupil and visual axis. Click image to enlarge. |
Additionally, an isopropyl alcohol solution may be needed to clean the lenses with its additional deposit-removing property in order to optimize lens comfort longer into the wearing cycle. If an isopropyl alcohol solution is recommended, the patient will additionally need to ensure that they have thoroughly rinsed the lens with saline to remove all the isopropyl alcohol before storing the lens in solution for overnight disinfection.
Takeaways
Patients who have a history of irregular astigmatism are often visually frustrated and even debilitated with spectacle lenses and standard soft lenses and will require some specialty lens management. There are many wonderful products in the marketplace to optimize lens fit and visual potential. Custom soft lenses are a wonderful example of a product capable of providing a stable lens-to-ocular surface fit profile with good centration, limited movement to optimize comfort and a central optical profile capable of exceptional vision. For the patient with irregular astigmatism, these lenses provide the patient and practitioner another significant and reliable tool to optimize fit, vision and comfort.
Dr. Lampa is a professor at the Pacific University College of Optometry. He is a fellow of the American Academy of Optometry. He is a consultant/advisor to SpecialEyes and has received honoraria or travel expenses from Art Optical, ABB Optical, Contamac and Medmont.

