
A 46-year-old Hispanic female presented for an eye exam complaining of decreased vision at near. She says she traditionally purchases over-the-counter reading glasses but worried that these spectacles may be harming her eyes.
She reported no complaints about her distance vision and was in excellent systemic health. Her family and ocular history was unremarkable.
On examination, her uncorrected visual acuity in each eye was 20/20 at distance and J3 at near. Confrontation visual fields were full to careful finger counting, and her pupils were equally round and reactive, without an afferent pupillary defect. The anterior segment examination of both eyes was unremarkable.
 |
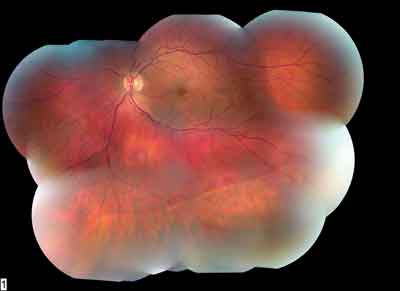 |
| 1. Montage images of the peripheral retina in the patient"s right eye. Of interest are two demarcation linesone pigmented, the other nonpigmented. | 2. The left eye has a similar pigmented demarcation line to the one in the right eye, but it was located too far anteriorly to be photographed. |
1. What do the changes in her retinas represent?
a. Lattice degeneration with atrophic retinal hole.
b. Retinal detachment.
c. Peripheral retinoschisis.
d. Both b and c.
2. Which statement is true regarding the retinal findings?
a. They are mostly unilateral.
b. They almost always are bilateral.
c. They can be either unilateral or bilateral.
d. This patients findings are not significant.
3. What do the pigmentary changes in the right eye represent?
a. Horseshoe retinal tear.
b. Atrophic retinal hole.
c. Retinal detachment.
d. Inner wall hole.
4. What is the correct diagnosis for this patient?
a. Lattice degeneration O.U. with atrophic retinal hole O.D.
b. Rhegmatogenous retinal detachment.
c. Peripheral retinoschisis.
d. Combined retinoschisis and retinal detachment.
5. How should this patient be managed?
a. Close follow-up with no surgery.
b. Retinal detachment surgery.
c. Laser photocoagulation.
d. Cryotherapy.
For answers, see below.
Discussion
The fundus photos represent a computer-generated montage of our patients peripheral retinas. Of interest are two demarcation lines in the peripheral retina of the right eyeone pigmented and one nonpigmented; the latter is located more posteriorly. The nonpigmented demarcation line is similar to the demarcation line seen in the left eye. The left eye has a similar pigmented demarcation line to the right, but it was too far anterior to be photographed.
The nonpigmented demarcation lines represent degenerative retinoschisis. Peripheral retinoschisis results from a splitting between the outer plexiform and inner nuclear layers of the retina.
Retinoschisis is often mistaken for retinal detachment, which results from a separation of the sensory retina from the retinal pigment epithelium (RPE). But, retinal detachments can be present anywhere in the retina, while peripheral retinoschisis more commonly appears inferotemporally, followed by superotemporally.1
Also, peripheral retinoschisis is usually bilateral. If you suspect a patient has a peripheral retinoschisis but you only see it in one eye, you probably missed the schisis in the second eye.
If this is the case, scleral depression may be helpful to confirm the diagnosis, ensure that the patient doesnt have retinoschisis in the second eye and ensure that the patient doesnt have combined retinoschisis and retinal detachment, which our patient did.
Clinically, degenerative retinoschisis appears as a smooth, well-circumscribed, nonmobile elevation of the inner retina that extends posterior from the ora serrata. A retinal detachment also can present as a well-circumscribed elevation of the retina. However, retinal detachments generally appear more sharply circumscribed and more mobile, especially on scleral depression. A retinal detachment typically collapses under the area of scleral depression, while a retinoschisis moves in accordance with the area of the retina that is being depressed.
Retinoschisis is very clear and transparent, allowing for the choroidal detail below the schisis to be easily seen. In fact, this transparency of the schisis cavity makes the condition difficult to detect on clinical examination.
By contrast, retinal detachments are not as transparent, and because of the anatomy of the detachment, choroidal detail is lost. Also, in those patients who have more longstanding (or chronic) retinal detachments, a pigmented demarcation line can be seen at the junction between attached and detached retina. This alone may be helpful in distinguishing between the two conditions, as retinoschisis is not associated with changes in the RPE; as only the outer layers of the retina are in contact with RPE.
So, how do we explain the pigmented demarcation line seen in this patients right eye (and in the left eye, though not seen in the photograph)? Our patient actually has a combined retinoschisis and retinal detachment.
Combined retinoschisis and retinal detachment occurs in up to 6% of eyes that have retinoschisis.1 These detachments typically are associated with outer wall holes within the schisis.1 In reality, both inner and outer wall holes may be necessary for a retinal detachment to occur, although usually only an outer layer break can be identified. Outer wall breaks are necessary to allow fluid to enter the subretinal space.
Outer wall holes may be single or multiple, and they may be small or large. They appear as retinal holes with smooth, rounded margins and rolled edges. These rolled edges are the hallmark of outer wall holes. Inner holes are rare and harder to diagnose due to the variations in the thickness of the inner retinal layer.
So, how should we manage this patient? Traditionally, combined retinoschisis and retinal detachments warranted treatment. However, in a published natural history series of 218 eyes (123 patients) with asymptomatic retinoschisis who were followed for nine years, none of the cases progressed during the follow-up period.1
The researchers concluded that in asymptomatic patients, this type of detachment is usually benign and rarely progressive. So, we can monitor these patients for progression at six weeks, three months and then every six to 12 months.1,2
Degenerative retinoschisis without retinal detachment generally is a benign condition and can be followed at six- to 12-month intervals. Posterior extension is rare. For patients whose disease progresses, vitrectomy with scleral buckling is the treatment of choice.
Because our patient had excellent visual acuity and minimal symptoms, we decided to observe her. So far, she has remained stable. We told her that she could use the over-the-counter reading glasses to address her reading complaints, but that she could not substitute these glasses for regularly scheduled eye exams.
Answers: 1) D; 2) B; 3) C; 4) D; 5) A
1. Byer NE. Long-term natural history study of senile retinoschisis with implications for management. Ophthalmology 1986 Sep;93(9):1127-37.
2. Wilkinson CP. Prevention of retinal detachment. In: Ryan SJ, ed. Retina, Vol.IIISurgical Retina. 3rd ed. St. Louis: Mosby, 2006: 2107-19.

