 |
A 62-year-old female presented to the office with a chief complaint of floating spots in the right eye of four weeks’ duration. Her systemic and ocular histories were unremarkable for treatable disease. She denied taking medications and reported no allergies of any kind.
Diagnostic Data
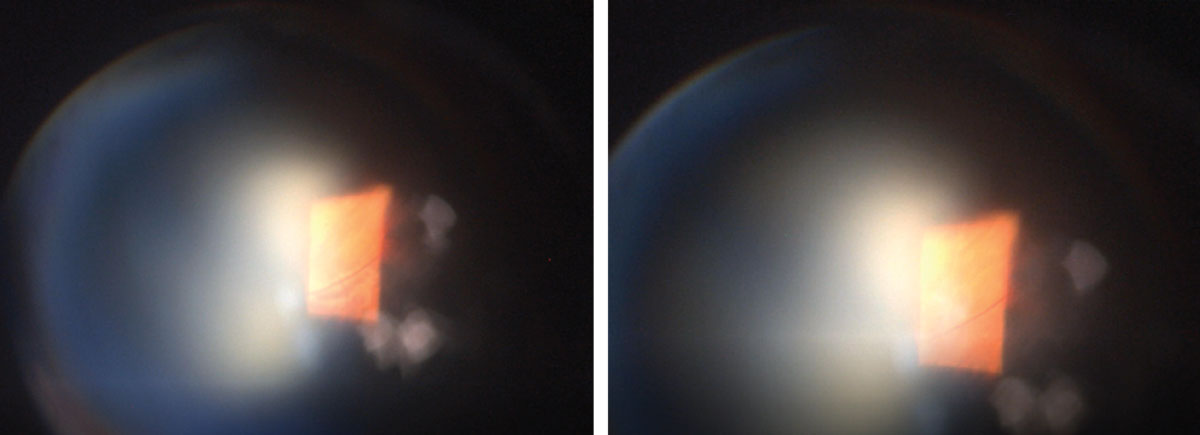
Her best-corrected visual acuity was 20/20 at distance and near OU. Her confrontation fields were full-to-finger-counting. Pupils were equal and normally reactive with no afferent defect. Refraction uncovered hyperopia with presbyopia OU. Biomicroscopy demonstrated normal anterior segment structures with intraocular pressures measuring 16mm Hg OD and 17mm Hg OS. The photographs illustrate the pertinent posterior segment finding.
Additional studies included photodocumentation and three-mirror evaluation with and without scleral depression.
 |
|
What might these unusual fundus images reveal about our patient? Left: lesion with off-axis 90° view. Right: lesion with digital pressure applied to the globe. Click image to enlarge. |
Ophthalmic ultrasonography may also be helpful in confirming the diagnosis. If uncertain, the clinician may opt for a referral to retinology, where further tests may include deep field optical coherence tomography, additional ultrasound testing, color doppler flow imaging or retinal angiographic testing.
Diagnosis
The diagnosis here is vortex vein varix. Elevated lesions of the peripheral retina raise concerns for sight-threatening pathologies such as retinal detachment, choroidal melanoma and benign conditions such as choroidal nevus and vortex vein varix.1,2
Vortex veins are convergences of choroidal veins that are evenly distributed throughout the mid-peripheral fundus. There are typically at least four vortex veins present, although commonly there are more.3 Rarely, this vessel can have an anomaly known as a varix, where it becomes distended or enlarged, causing the overlying retinal anatomy to take on an elevation that mimics a space-occupying lesion. This phenomenon is often misidentified and makes up 1% of “pseudomelanoma” referrals.1
A varix is a distended or enlarged vein that can occur anywhere throughout the body.4-6 They are most commonly seen in lower leg extremities (10% to 30% of the population) and are the most common sign of lower extremity chronic venous disease.4-6 The etiology is thought be related to irregularities of venous wall architecture, contractile insufficiency of smooth muscle in the venous wall or changes in venous tone that make the vein distendable.4
Due to the dynamic nature of a vortex, ampulla varices may stem from kinking of the extrascleral vortex vein or obstruction by oblique muscles.1,2 Although they are not correlated, venous varices may also occur in the orbit, where they can cause orbital pain, proptosis, optic nerve compression and spontaneous orbital hemorrhage.7 Vortex vein varix exhibit the pathognomonic characteristic of disappearing upon application of light pressure to the globe.1
Differential diagnosis is based on recognition of color, shape and its dynamic nature. The pathognomonic sign is shrinkage with application of light digital pressure, raising of head posture or change in position of gaze (visualized through ultrasonography or three-mirror Goldmann contact lens).2,8 The lesion should increase in thickness when gaze is in the direction of the lesion and decrease in thickness when gaze is directed away from the lesion.2,9 Ultrasonography is also useful in observing the thickness changes in the different positions of gaze. The overall acoustic characteristic is solid.9,10
There is no management for these phenomena. They are benign. They do not break, bleed, leak or remodel. They never lose function. Photodocumentation is appropriate and ophthalmic ultrasonography may be helpful in confirming the diagnosis. If the diagnosis is tenuous, a referral to retinology can be completed; the retina specialist may complete deep-field OCT, ultrasound testing, color doppler flow imaging or retinal angiographic testing.
Dr. Gurwood thanks Nick Karbach, OD, for contributing this case.
Dr. Gurwood is a professor of clinical sciences at The Eye Institute of the Pennsylvania College of Optometry at Salus University. He is a co-chief of Primary Care Suite 3. He is attending medical staff in the department of ophthalmology at Albert Einstein Medical Center, Philadelphia. He has no financial interests to disclose.
1. Patrick KA, Shields CL. Vortex vein simulating choroidal melanoma. Retina Today. 2013;10:43-45. 2. Levy J, Yagev R, Shelef I, Lifshitz T. Varix of the vortex vein ampulla: a small case series. European Journal of Ophthalmology. 2004;14(3):424-7 3. Vahdani K, Kapoor B, Raman VS. Multiple vortex vein ampulla varicosities. BMJ Case Reports. 2010;2010:bcr0820103223. 4. Meissner MH. Lower extremity venous anatomy. Seminars in Interventional Radiology. 2005;22(3):147-156. 5. Evans CJ, Fowkes FG, Ruckley CV, Lee AJ. Prevalence of varicose veins and chronic venous insufficiency in men and women in the general population: Edinburgh Vein Study. Journal of Epidemiology and Community Health. 1999;53(3):149-153. 6. Chiesa R, Marone EM, et al. Chronic venous disorders: correlation between visible signs, symptoms, and presence of functional disease. J Vasc Surg. 2007 Aug;46(2):322-30. |

