 |
|
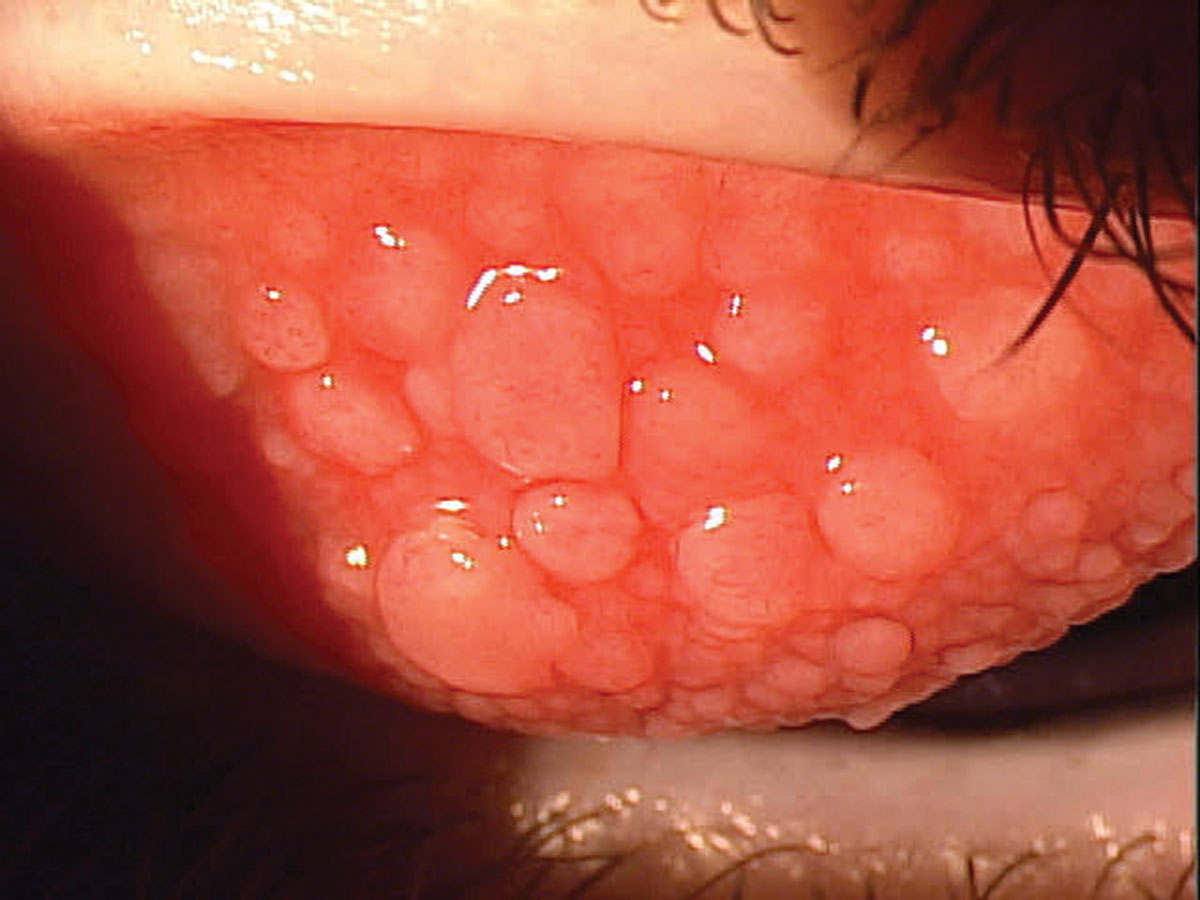
Identifying possible clinically relevant allergens provide information that may aid in managing VKC. Photo: Paul Karpecki, OD. Click image to enlarge. |
More than half of vernal keratoconjunctivitis (VKC) patients have allergic sensitivities, a recent literature review found. While not all cases of this severe ocular allergic disease follow a seasonal pattern, VKC is still suspected to be an immunologically mediated hypersensitive reaction to environmental allergens. The review study shed more light on the prevalence of VKC with allergy.
The authors identified 33 eligible cross-sectional studies for qualitative analysis with a total of 2,122 VKC patients. They reported that, overall, the most prevalent positive allergen tests were inhaled allergens such as house dust mites and pollen. Of the 33 studies, 29 were eligible for quantitative analysis, and the researchers calculated the prevalence of allergen-positive patients to be 58%. Pooled estimates on sensitization showed estimates of 51% for the conjunctival provocation test, 69% for total tear immunoglobulin E (IgE), 59% for specific tear IgE and 58% for the skin prick test.
One of the studies included in the meta-analysis sampled patients’ house dust and measured their specific IgE for dust mites monthly for one year. From June to September, an increase in tear IgE was observed, reflective of increased mite levels in summer months. Subsequently, flares of VKC may be correlated with the temporal change of the summer months due to mite prevalence.
Dust mites, though, are just one of many allergens that VKC patients display sensitivity to. VKC patients’ tears reflect other specific IgE levels for grass and tree pollen, as well as for cat and food allergies. These specific IgE, along with total IGE levels, were significantly higher in VKC patients compared to controls, but displayed similarity of levels with other allergic and atopic conditions.
|
For more on clinical management of VKC, please see this recent article. |
Sensitization to allergens of VKC patients also seems to be related at least partly to geography. The researchers “observed a clear pattern of geographic differences in sensitization, which at least to some extent may also be reflected in the variation in testing panels,” they wrote in their paper. Despite differences in testing panels and prevalent allergens by region, geography still impacted the rate of variation in positive tests for more universal triggers.
The authors concluded that identifying clinically relevant allergens—e.g., house dust mites and pollen—can offer additional information and direction when managing VKC, such as environmental allergy-avoidance or allergy-specific treatment. “However,” they wrote in their paper, “it should be noted that this may only be relevant for a proportion of the patients, and when planning testing and informing patients and parents, it’s important to understand that about 40% of the patients do not have any allergies.”
For VKC patients, it is advised to re-test for allergies if the severity of their symptoms becomes worse, or upon suspicion of a new allergy. Taking these measures can lead to helpful treatment, such as allergen-specific immunotherapy for house dust mite or pollen allergies, which has reduced ocular allergic symptoms.
Roed Rasmussen ML, D’Souza M, Topal DG, et al. Prevalence of allergic sensitization with vernal keratoconjunctivitis: a systematic review with meta-analyses. Acta Ophthalmol. July 18, 2022. [Epub ahead of print]. |

