 |
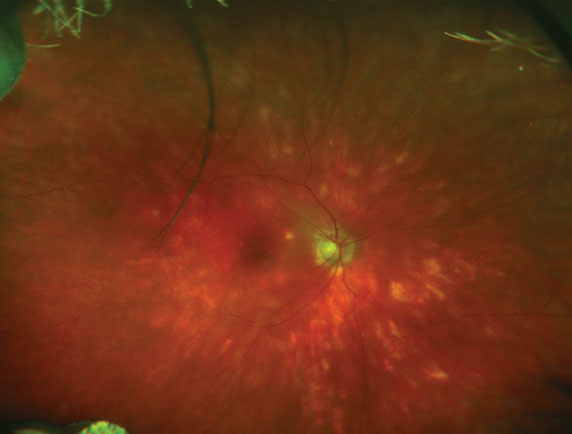
| Chorioretinitis (see here from another cause) can manifest in patients with systemic fungal infection. Photo: Ellen Butts, OD. Click image to enlarge. |
If your patient has a Candida bloodstream infection (BSI), it’s important to maintain suspicion for ocular candidiasis (OC), which can complicate Candida BSI. Among OC cases, Candida albicans is the most common finding. Candida BSI is associated with serious underlying medical conditions and high mortality, including ICU patients, those with major abdominal surgery procedures and neutropenia. Many patients suffer from Candida colonization in catheters, which then transfers to the gut and bloodstream.
In general, antifungals improve the prognosis of BSI patients, but choice of treatment and timing of first-line medication on OC risk aren’t completely understood yet. However, a recent study reported that early treatment initiation is key for reducing endophthalmitis risk.
The researchers included all Candida BSI patients (n=304) at the Oulu University Hospital in Finland. Patients who had a clinical condition appropriate for ocular examination including biomicroscopy (n=103) were analyzed for Candida and yeast species, antifungal medications, echocardiography, underlying diseases and other clinical properties.
Of the 103 patients, 33 (32%) were diagnosed as having OC, with Candida albicans as the most common finding (88%) in this cohort. Here are some of the other study findings:
The presence of persistent candidemia increased the risk of OC.
94% of OC patients were diagnosed with chorioretinitis.
48% of OC patients were diagnosed with endophthalmitis.
Early antifungal treatment decreased endophthalmitis risk.
Echinocardin lowered OC risk in patients with central venous catheters or abdominal malignancies.
The researchers explained that candidemia patients are often severely ill, and though an ophthalmological consultation is recommended for these patients, it isn’t always feasible. Incidence of OC in candidemia may range from 3% to 27%, they noted. “In our study, ocular examination was completed for the selected patients due to their critical condition. The examined patients appeared to be of younger age and healthier compared with those who were not examined. Patients at intensive care units, those with alcohol-related conditions or poor prognosis, for example, were less frequently examined.”
“We also found that patients whose blood cultures remained positive for Candida albicans during antifungal treatment were at OC risk. Importantly, a shorter duration in persistence of candidemia was seen in echinocandin-treated patients with central venous catheters. It’s known that echinocandins can be active against Candida biofilm.” They believe such activity against the biofilm may protect a candidemia eye from developing complications.
While their findings were consistent with other studies, demonstrating that Candida albicans is the most prevalent fungal isolate among OC patients, they noted that observed selection bias in patients who received ocular exams may have influenced their results.
The investigators concluded that early treatment is key for reducing endophthalmitis risk. “Those who received either fluconazole or echinocandin within 12 hours had a lower number of endophthalmitis when compared with cases with a delay of more than 12 hours. However, a delay in antifungal treatment wasn’t associated with an increase in chorioretinitis when the entire study population was considered. In addition, no advantage of fluconazole, a drug of choice in intraocular Candida albicans infections, was seen.” They recommend a low intraocular concentration of first-line echinocandin in patients with central venous catheters or abdominal malignancies.
“Interestingly, none of the patients without Candida albicans who received echinocandin developed OC,” they added. “This is in line with a recent study that reported no increased ocular involvement in patients with Candida BSI initially treated with echinocandins.”
Hautala N, Köykkä H, Siiskonen M, et al. Effect of first-line antifungal treatment on ocular complication risk in Candida or yeast blood stream infection. BMJ Open Ophthalmol. September 16, 2021. [Epub]. |

