 |
Congenital anomalies of the optic disc may occur in isolation or as part of a larger systemic syndrome. These malformations include optic nerve hypoplasia, optic pit, coloboma, morning glory disc anomaly (MGDA), tilted disc, peripapillary staphyloma, megalopapilla and optic nerve drusen.1-3 Visual impairment is one of many side effects these patients could experience. Concurrent neurologic and systemic features help identify and predict possible outcomes, which may be life-threatening.
Case Report
A 58-year-old Caucasian female presented with complaints of bilateral blur, worse at near, in each eye. Her health history was positive for Moyamoya disease (MMD) and related cerebrovascular accident. Distance acuities with correction measured 20/20-2 OD and OS. Dilated fundus examination revealed MGDA with an enlarged nerve head, retinal excavation, glial tissue and anomalous retinal vessels, all in the right eye. Fundus examination of the left eye was unremarkable.
Central retinal photography and OCT results were consistent with MGDA in the right eye. The patient was informed on the importance of continued care and scheduled for a return visit to undergo central threshold perimetry. Her ocular status will continue to be monitored on a biannual basis with appropriate refractive, structural and functional ophthalmic evaluation.
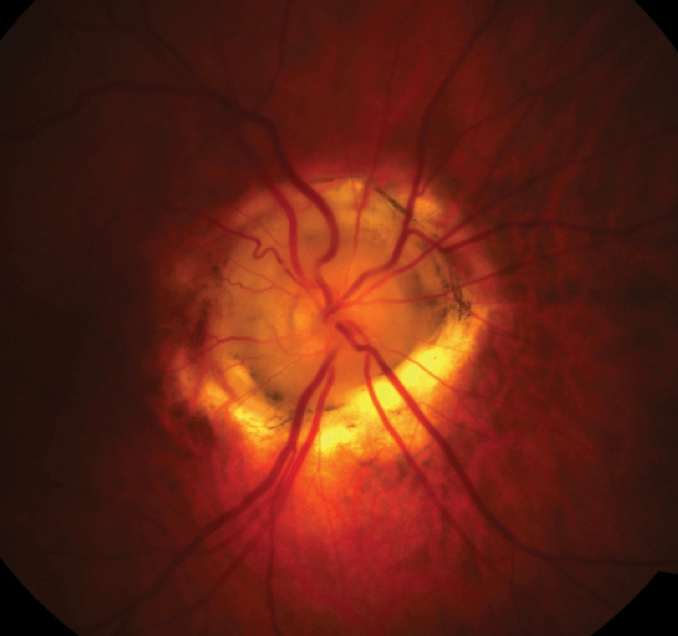 |
| Fig. 1. Enlarged, excavated optic nerve with glial tissue and anomalous retinal vessels. Click image to enlarge. |
Flowery Fundus
Named for its resemblance to the morning glory flower, MGDA is an uncommon optic disc anomaly (Figure 1). An embryonic developmental alteration of the lamina cribrosa and posterior sclera causes this defect.1-4
MGDA may present on its own or in association with systemic or intracranial vasculapathies, such as MMD, which occurs in up to 50% of patients with the anomaly.2-4 It appears as a large optic disc with funnel-shaped excavation of the surrounding retina, annular pigmentation around the nerve head, a characteristic glial tuft and an abnormal retinal vascular pattern that presents in a spoke-like fashion around the disc (Figure 2). MGDA is usually sporadic and hasn’t been linked to a specific genetic defect.
Hand-in-hand Vasculopathy
MMD was first described in Japan in 1957.5 It predominantly affects people of Asian descent—the highest incidence falls among Japanese and Korean patients.5,6 The annual incidence of MMD is 0.086 per 100,000 people in the United States compared with 3.16 to 10.5 per 100,000 people in Japan.6,7 Although the etiology of MMD is unknown, the East-West ethnicity discrepancy suggests a strong genetic predisposition.7
The age of onset follows a bimodal distribution, with an initial peak occurring in children between five and 10 years of age and a second peak affecting adults in their fourth or fifth decade of life.6
The clinical presentation of MMD differs between children and adults. Children mainly exhibit ischemic symptoms, the most common being a transient ischemic attack (TIA), which is usually recurrent.6,8 Adults usually present due to an ischemic stroke or an intracranial hemorrhage secondary to fragile collateral vessel rupture, which can ultimately result in acute transient or permanent symptoms secondary to brain ischemia.5,6,9 Patients report symptoms that include headaches, seizures, hemiparesis, sensory impairment and aphasia/dysarthria and may experience severe disability or even mortality.7,9,10
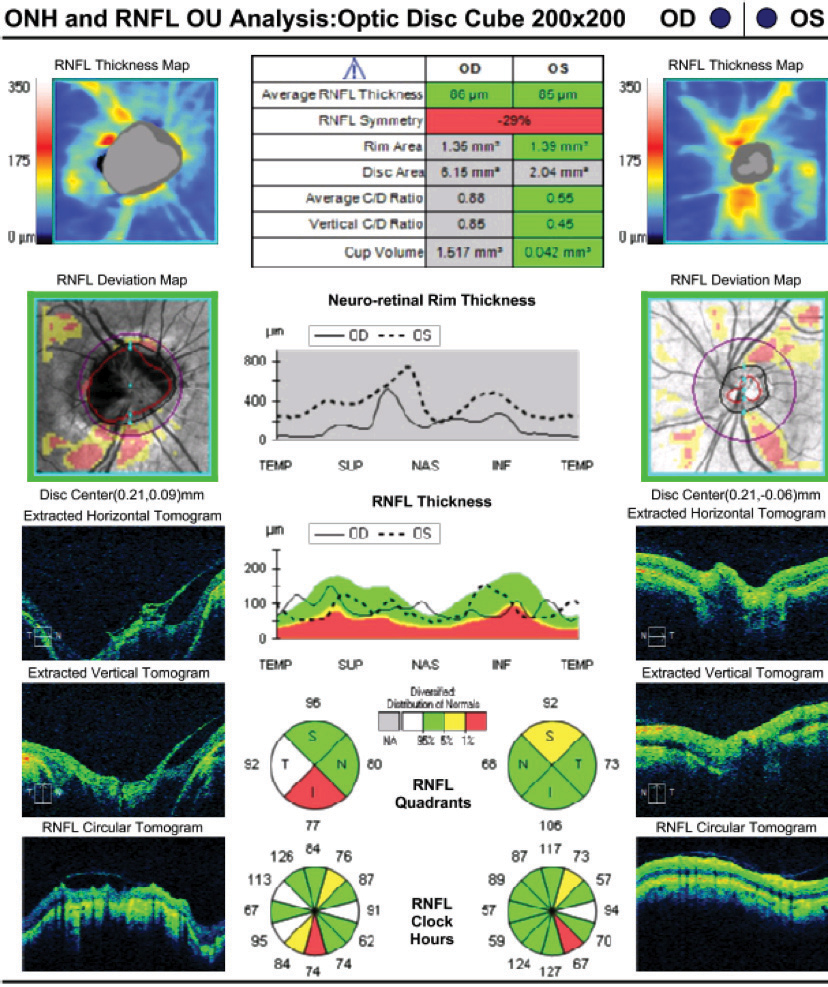 |
| Fig. 2. OCT revealing enlarged disc area of the right optic nerve and excavation. Click image to enlarge. |
Moyamoya angiopathy typically presents with various cerebrovascular manifestations that include TIA, ischemic stroke, hemorrhagic stroke, seizures and headaches.10,11 The angiopathy can present as the sole manifestation of MMD or exist in association with other factors, such as Down syndrome, autosomal-dominant thoracic aortic aneurysm, head tumor radiotherapy, sickle cell disease and neurofibromatosis, in which case it is referred to as Moyamoya syndrome.8,10,11 It can result in progressive stenosis and occlusion of the internal carotid artery (ICA) and/or the proximal portion of the anterior cerebral and middle cerebral arteries.
Moyamoya, a Japanese word that translates to “puff of smoke,” refers to a network of abnormal, thin, fragile collateral vessels that are evident on cerebral angiography and resemble a smoke cloud.5,6,10 These vessels develop at the base of the brain, adjacent to the site of occlusion secondary to chronic brain ischemia.1,6,10,11
Make the Diagnosis
Diagnosing MMD requires visualization of at least one ICA and/or its branches as well as the network of collateral vessels.6,7 Radiologic assessment, therefore, is an important factor in detecting MMD. MRI/MRA may be sufficient to diagnose the disease when findings are bilateral; however, unilateral cases require catheter angiography.7,9,12
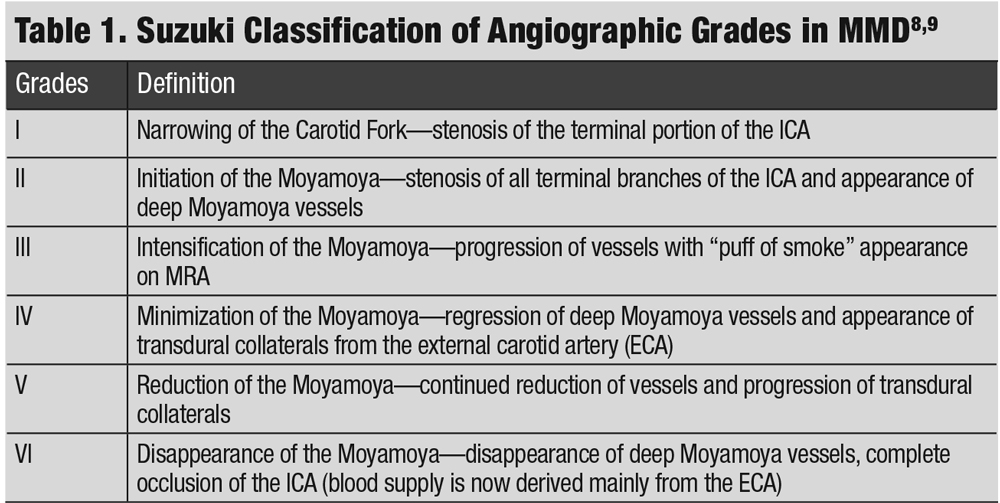 |
| Click table to enlarge. |
Treat and Manage
The course of MMD spans from clinical silence for several years to rapid progression.5,7 Its severity can be classified into six stages based on Suzuki’s classification, which highlights the angiographic evolution of the disease (Table 1).8,9 A management plan is decided accordingly.
There is no curative treatment for arterial occlusion regression or Moyamoya vessel prevention. Due to the more progressive nature of the disease in the pediatric population, treatment is geared toward preventing irreversible brain damage.8,12 Treatment is strongly recommended for symptomatic adults since the stroke rate is estimated at 10% to 15% per year compared with 3% in asymptomatic patients.7,9,11,12
The mainstay of treatment in symptomatic patients with ischemic MMD is surgical revascularization.9,12 The goal is to improve cerebral blood flow and prevent infarction. Direct or indirect bypass has been shown to improve blood flow and decrease ischemic events postoperatively.12 Post-op complications may include permanent neurologic deficits secondary to ischemic or hemorrhagic stroke. These can be caused by several factors, largely depending on the patient’s hemodynamic status.7,12 Treating hemorrhagic MMD is more controversial and remains unspecified.
Patients who present with MGDA or another optic nerve anomaly may have other neurological signs and symptoms that a fastidious history can help reveal. When these signs and symptoms are present, the clinician should order neuroimaging to assess the vascular and structural integrity of the brain and work hand-in-hand with neurology and neurosurgery specialists to decrease the risk of mortality from potential cerebrovascular events.
Dr. Hehar is an instructor at the Pennsylvania College of Optometry.
| 1. Ponnatapura J. Morning glory syndrome with Moyamoya disease: a rare association with role of imaging. Ind J Radiol Imag. 2018;28(2):165. 2. Kalra VB, Gilbert JW, Levin F, et al. Spectrum of MRI findings in morning glory syndrome. Neurographics. 2014;4(1):56-60. 3. Ellika S, Robson CD, Heidary G, et al. Morning glory disc anomaly: characteristic MR imaging findings. Am J Neuroradiol. 2013;34(10):2010-4. 4. Nezzar H, Mbekeani JN, Dalens H. Morning glory syndrome with carotid and middle cerebral artery vasculopathy. Optom Vis Sci. 2015;92(12):e437-41. 5. Fukui M, Kono S, Sueishi K, et al. Moyamoya disease. Neuropathology. 2000;20 Suppl:S61-4. 6. Kim JS. Moyamoya disease: epidemiology, clinical features, and diagnosis. J Stroke. 2016;18(1):2-11. 7. Guey S, Tournier-Lasserve T, Hervé D, et al. Moyamoya disease and syndromes: from genetics to clinical management. Appl Clin Genet. 2015;16(8):49-68. 8. Deepa J, Muthusamy K, Bandla B, et al. Ocular features and visual outcome in children with Moyamoya disease and Moyamoya syndrome: a case series. J Clin Diagn Res. 2016;10(5):NR01-4. 9. Suzuki J, Kodama N. Cerebrovascular “Moyamoya” disease. Arch Neuro. 1969;20(3):288. 10. Bersano A, Guey S, Bedini G, et al. Research progresses in understanding the pathophysiology of Moyamoya disease. Cerebrovasc Dis. 2016;41(3-4):105-18. 11. Rupareliya C, Lui F. Moyamoya Disease. In: StatPearls. Treasure Island (FL): StatPearls Publishing; January 3, 2019. 12. Kim T, Oh CW, Bang JS, et al. Moyamoya disease: treatment and outcomes. J Stroke. 2016;18(1):21-30. |

