The current paradigm for glaucoma detection involves comprehensive history, an ocular examination and many ancillary tests to identify structural and functional optic nerve damage signs. Since no litmus test exists for glaucoma, it falls to clinicians to synthesize and interpret multiple types of information; naturally, this can lead to issues of inconsistencies or disagreements even among glaucoma experts.
Of importance, there’s a lack of consensus on the definition of what constitutes clinically significant glaucomatous optic neuropathy (GON). New research published in Translational Vision Science & Technology aims to close this gap. Researchers evaluated the ability of OCT alone to detect established glaucoma from an OCT-based reading center for glaucoma.
Included in the investigation were eyes of 70 consecutive patients with established glaucoma (either moderate or severe as followed by the International Classification of Diseases) and 20 consecutive healthy individuals with no evidence of GON or visual field loss. After standardized quality assessment by a reading center, 33 eyes were excluded for media opacity, poor image quality or epiretinal membrane. The remaining 147 eyes included 86 with established glaucoma and 36 from controls.
Based on the OCT report alone and applying an evaluation method developed at Columbia University, the presence or absence of GON in each eye was determined by two masked graders, the researchers explained in their paper. Of the 86 glaucomatous eyes, only one was missed, but the other eye of the same patient was correctly classified as GON. As such, the sensitivity was 100% at a patient level. No healthy eyes were classified as GON, either. Based on these observations, a reading center applying the standardized Columbia method for evaluating images can correctly detect established glaucoma in a real-world clinical setting with both high sensitivity and specificity.
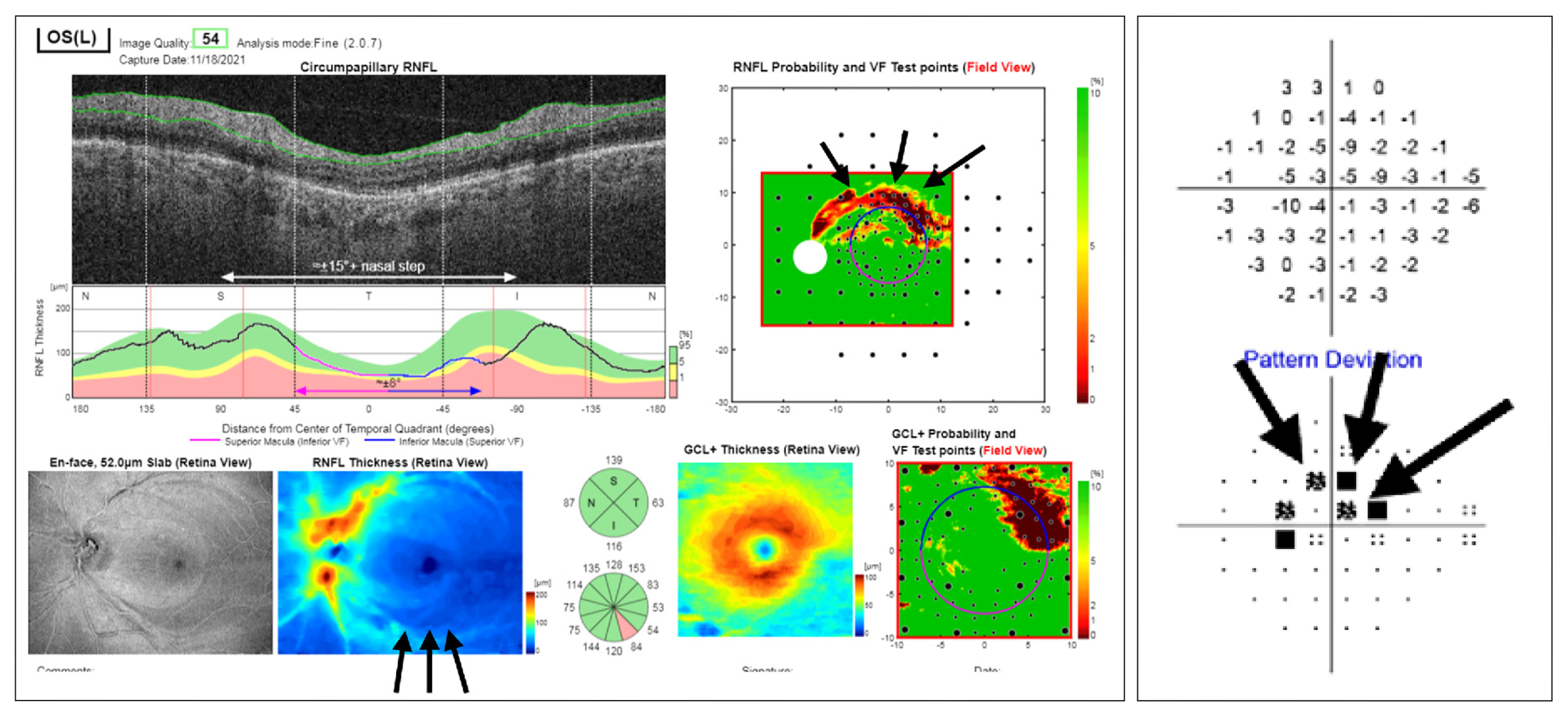 |
| Application of this screening method might help providers who are not glaucoma specialists to determine who should and should not be referred for further evaluation and need for treatment. The OCT report is composed of probability and thickness maps for the RNFL and GCL as well as circumpapillary RNFL B-scan and thickness plot, all of which are used for classification by the Columbia method. In this case, there is an arcuate-like inferior hemiretinal defect that corresponds to the superior arcuate defect on the 24-2 visual field (black arrows). Photo: Leshno A, et al. Transl Vis Sci Tech. 2024;13(1)4. Click image to enlarge. |
The study authors contemplate that “possible applications of this technique include validation of inclusion or exclusion criteria related to the presence of GON for clinical trials, or screening out individuals who do not have clear evidence of GON. In addition, it can be used for detection of patients at risk of functional visual field loss and blindness (i.e., ‘established glaucoma’ at the time of diagnosis).”
They continue that the performance of a reading center applying the Columbia method alone to identify these eyes has multiple advantages. One is that no eyes with moderate to severe visual field loss were missed. Since these patients are likely at risk of severe vision loss and blindness, missing any eyes like this would present a problem. Another advantage is that all patients with GON were judged as having at least one eye categorized as such. In other words, no patients in this cohort would have been missed using this method for screening, as the method detected all patients with established glaucoma in at least one eye.
For clinical application, the authors posit that “the high sensitivity and specificity found here highlights the potential of the [reading center] to enable timely referral of individuals with established glaucoma as well as avoiding unnecessary visits of those who are found to be healthy.”
Leshno A, Tsamis E, Hirji S, et al. Detecting established glaucoma using OCT alone: utilizing an OCT reading center in a real-world clinical setting. Transl Vis Sci Technol. 2024;13(1):4. |

