 |
Q:
I have a patient who requires oral antiviral prophylaxis for recurrent herpes simplex keratitis. Are there any significant risks for viral resistance with chronic antiviral use?
“Antiviral prophylaxis has been used for decades in patients with herpes simplex keratitis. Prior to the availability of oral antivirals, topical antivirals were used,” explains Christopher J. Rapuano, MD, of Wills Eye Hospital in Philadelphia. It was common practice to use topical trifluridine the same number of times a day as the topical steroid. When oral acyclovir was FDA-approved in the 1980s, physicians began using it instead of the topical antiviral medications. When valacyclovir and famciclovir were later FDA-approved in the 1990s, the use of oral antivirals increased, Dr. Rapuano elaborates.
But it wasn’t until 1998, with publication of the Herpes Eye Disease Study (HEDS) that looked at the prophylactic use of oral acyclovir in eyes with herpes simplex ocular disease, when it became essentially the standard of care. The study found an approximate 50% decrease in recurrence of ocular herpes with the one year of 400mg acyclovir used twice daily, and with no rebound effect when it was stopped for six months.
Current Guidelines
While the dosages vary per patient, the current standard prophylactic dose of acyclovir is 400mg BID, valacyclovir 500mg QD and famciclovir 250mg one to two times a day; however, the length of prophylaxis has not been fully established. “HEDS showed effectiveness for one year, but many doctors will keep their patients on for much longer. Most surgeons who perform a corneal graft in an eye with herpes simplex keratitis will continue their prophylaxis for many years, if not for life,” declares Dr. Rapuano.
Clinicians must remember that while oral antiviral prophylaxis is effective, breakthrough herpes keratitis can still occur. HEDS demonstrated a 50% decrease in ocular herpes, not 100% elimination, Dr. Rapuano reminds. Having said that, when a patient on oral antiviral prophylaxis is either not responding to the antiviral medication or is getting frequent recurrences, the questions of compliance with medication use and of antiviral resistance should be considered.
Viral Resistance
Just like prolonged antibiotic use can promote resistance, so can prolonged antiviral use. Resistance of the herpes simplex virus (HSV) to oral acyclovir is thought to be rather low, with reports of 0.6% in immunocompetent patients. However, in immunosuppressed patients, the resistance rate jumps anywhere from 3% to 6%. Resistance is usually due to a mutation of the thymidine kinase gene, which is needed to convert acyclovir, valacyclovir, famciclovir and ganciclovir in order to inhibit viral replication. “In such cases,” Dr. Rapuano advises, “one can consider using high-dose IV acyclovir to overcome the resistance, but that can induce renal toxicity.” Interestingly, he notes, studies have not looked at alternating regimens of chronic antiviral medications to reduce resistance, but as these medications all have a similar mechanism of action, this approach may not be promising.
 |
|
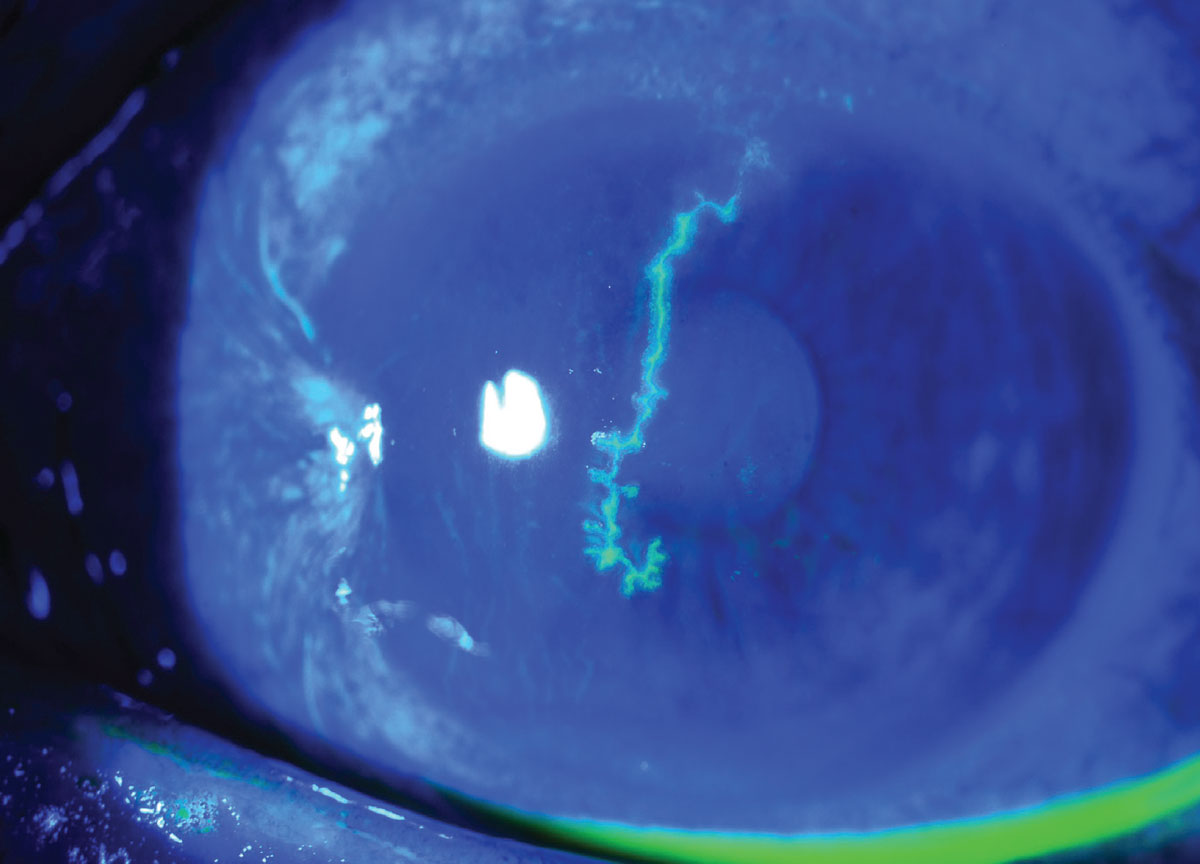
A 54-year-old man with a history of a pterygium in this eye presented with a large central HSV dendrite. It was treated with oral valacyclovir and resolved. He has been maintained on prophylactic oral valacyclovir to prevent recurrences, especially as this dendrite was so large and central. Click image to enlarge. |
There are some antiviral drugs that do not rely on thymidine kinase phosphorylation, including foscarnet and cidofovir, Dr. Rapuano adds. Foscarnet is currently indicated for cytomegalovirus (CMV) retinitis and mucocutaneous acyclovir-resistant HSV. It is only available as an IV medication and has numerous side effects, including renal abnormalities. Cidofovir, typically used for CMV retinitis, is also an IV medication that can be used when foscarnet is unsuccessful in acyclovir-resistant patients. Unfortunately, it has even more side effects than foscarnet, reportedly including renal failure after just one or two doses. Consequently, these drugs are generally reserved for severe herpes simplex infections. One can consider using topical trifluridine (but this is quite toxic to the corneal surface) to vidarabine (not commonly available), which may be effective.
Dr. Rapuano summarizes that resistance to the commonly used prophylactic antiviral medications for HSV keratitis is rare in immunocompetent patients, but not as rare in immunosuppressed patients, so antiviral resistance should be kept in mind when considering this population. High-dose IV acyclovir, IV foscarnet or IV cidofovir can be considered in severe cases. “The good news is that new therapies, including RNA peptides, cationic peptide therapy and interferon alpha-2b, are being investigated to treat acyclovir resistant HSV,” he says.
Dr. Shovlin, a senior optometrist at Northeastern Eye Institute in Scranton, PA, is a fellow and past president of the American Academy of Optometry and a clinical editor of Review of Optometry and Review of Cornea & Contact Lenses. He consults for Kala, Aerie, AbbVie, Novartis, Hubble and Bausch + Lomb and is on the medical advisory panel for Lentechs.
1. Acyclovir for the prevention of recurrent herpes simplex virus eye disease. Herpetic Eye Disease Study Group. N Engl J Med. 1998;339(5):300-6. 2. Esra N, Hollhumer R. Herpes simplex virus-related conjunctivitis resistant to aciclovir: a case report and review of the literature. Cornea. 2021;40(8):1055-8. 3. Moshirfar M, Kelkar N, Peterson T, et al. The impact of antiviral resistance on herpetic keratitis. Eye Contact Lens. 2023;49(3):127-34. |

