 |  |
In this month’s column, we are breaking from the usual format of spotlighting particular procedures to talk about an interesting debate going on cataract surgery circles right now.
We’ve all had the following questions asked by patients: What is a cataract? Who do we go to for surgery? What should we expect for the procedure? Which IOLs should we consider? But how many of you have had the discussion with patients about them having both eye surgeries performed at the same time? Most probably haven’t; however, this is a consideration we could potentially hear about in the future.
Immediate sequential bilateral cataract surgery (ISBCS) is a surgical protocol performed on both eyes on the same day but as separate procedures to minimize infection risk.1 Although rarely performed in the United States and somewhat controversial worldwide, ISBCS is being performed due to its potential benefits and patient satisfaction. In our experience, we’ve had a handful of patients undergo ISBCS due to health and systemic safety considerations.
While we optometrists don’t perform the procedure, it’s important for us to educate patients when doing referrals for cataract surgery, as well as stay in the loop about trends, conversations and controversies in cataract surgery. Here, we will discuss the pros and cons of ISBCS and the issues at stake.
 |
|
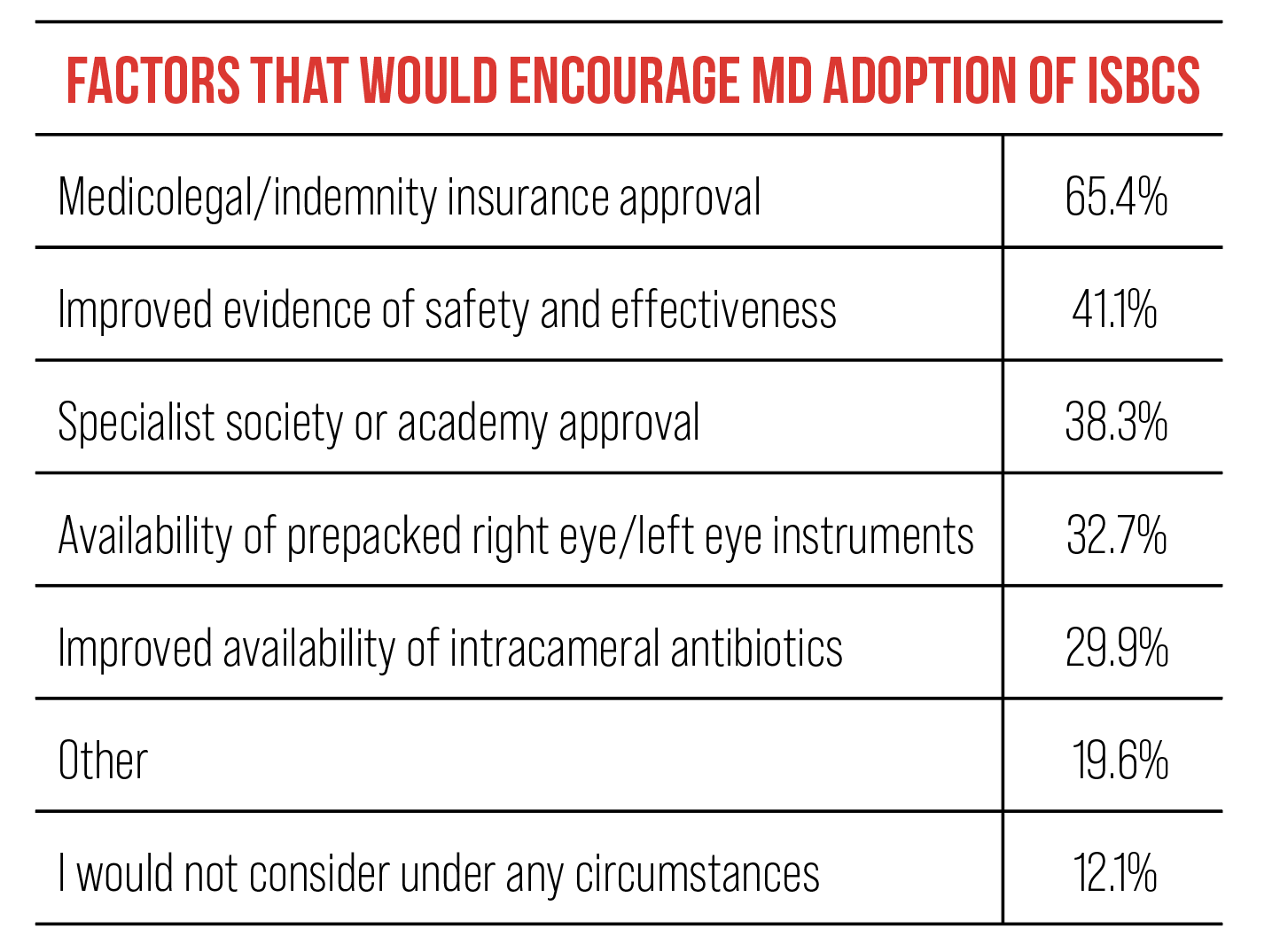
Adapted from Rush SW, Guerrero Criado AE, Kezirian GM, Durrie D. Immediate sequential bilateral cataract surgery: opinions among refractive surgeons in the United States and a comparative analysis with European consultants. J Ophthalmol. 2022:8310921. Click image to enlarge. |
Why ISBCS Should Be Considered
Currently, an estimated 3.5 million patients have cataract surgery each year in the US, with the vast majority of them being performed in the context of delayed sequential bilateral cataract surgery (DSBCS).2 This protocol is the standard of care in the US we’re all familiar with. Nonetheless, with the growth and aging of our population, the need and demand for cataract surgery will continue to increase; however, the supply of surgeons available is not adequate. Across a future 15-year time span, researchers report that the total ophthalmology supply is projected to decrease by 2,650 full-time ophthalmologists, equating to a 12% decline. Meanwhile, the total demand is projected to increase by 24%, or 5,150 full-time ophthalmologists, representing a supply and demand mismatch of 30% workforce inadequacy.3
 |
|
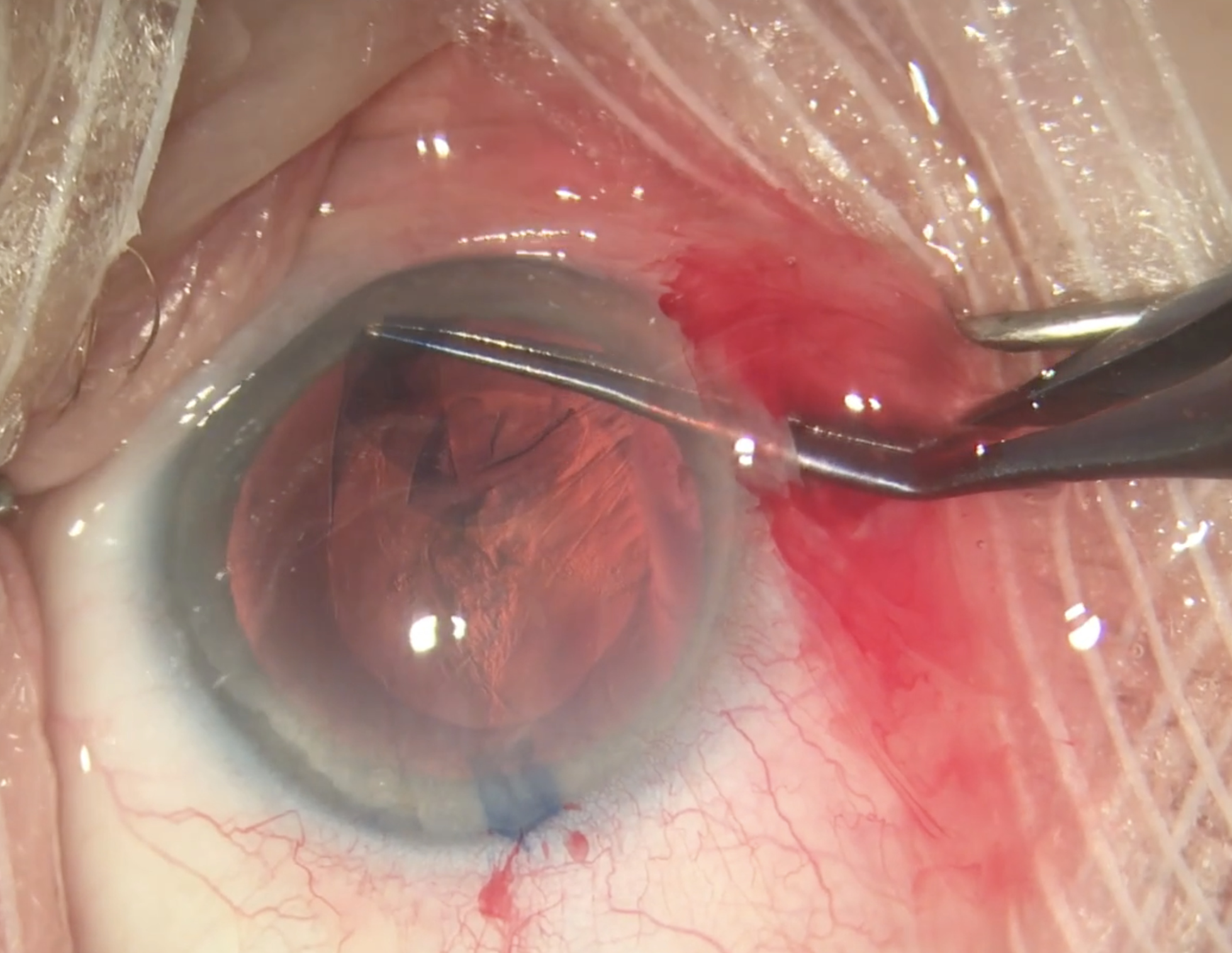
Today’s highly predictable and safe cataract procedures are laying the groundwork for an eventual shift to same-day bilateral surgery. Photo: Christina Tran, BS, and Leonid Skorin, Jr., DO, OD. Click image to enlarge. |
Evolution of Cataract Surgery
Cataract surgery has changed dramatically over the last four decades, but many of our general policies and even practice patterns have been slower to adapt. Decades ago, cataract surgery was much more involved and thus carried more complications and a longer recovery time. Initial precautions were based around intracapsular cataract extraction, where the entire lens and capsule were both removed through relatively large incisions that required suturing. For this reason, we often wanted a significant period of time to elapse to ensure the first eye was stable before considering surgery on the other eye.
A giant leap occurred once extracapsular cataract extraction with phacoemulsification became popular, but even early versions of this were considerably more complication laden that what we are accustomed to now. Conventional cataract surgery has become dramatically safer and more predictable because we disrupt much less tissue, use less and more precise intraocular energy, and spend very little time in the eye.
Current cataract surgery is typically performed through an incision that’s less than 3mm in length and rarely requires suturing. Typical cases are often completed in under eight minutes after the primary incision is made. Energy applied through phacoemulsification is kept to a minimum and very precise. Although there is always variability in the human population, it is common for patients to have no pain and functional vision the next day.
Rates of sight-threatening complications have become so low that, often, realistic odds of a complications cannot be given. More relevant to this discussion is the occurrence of a complication in one routine eye, which is rarely predictive of the same complication occurring in the other. (These considerations are all assuming that the patient does not have significant preoperative risk due to pre-existing conditions. If that is the case, ISBCS would not be a consideration.)
The question is: Are we at a point that we can reasonably consider ISCBS from a safety standpoint? Considering the current safety and predictability of cataract surgery, it would seem so.4,5 Safety, although of paramount importance, is not the only consideration when contemplating how to deliver care to cataract patients, especially when considering our mission to the community or society as a whole. Same-day bilateral surgery would allow more people to receive surgery sooner, while also saving money in the healthcare system. For each individual patient, the approach is faster, more convenient and entails fewer visits.
Cons of ISBCS include medicolegal concerns, the inability of the surgeon to handle refractive surprises (by altering the surgical plan on the second eye due to unexpected refractive response to the first), sight-threatening complications such as endophthalmitis and decreased reimbursement.
The majority of the US refractive cataract surgeons in a recent survey indicated that ISBCS should not be the standard of care in routine cases, with the prevailing reason being concerns about decreased physician reimbursement and potential medicolegal issues, not safety.6 But sentiments may change in time as those issues are addressed.
Dr. Cunningham is the director of optometry at Dell Laser Consultants in Austin, TX. He has no financial interests to disclose. Dr. Whitley is the director of professional relations and residency program supervisor at Virginia Eye Consultants in Norfolk, VA. He is a consultant for Alcon.
1. Kessel L, Andresen J, Erngaard D, et al. Immediate sequential bilateral cataract surgery: a systematic review and meta-analysis. J Ophthalmol. 2015;2015:912481. 2. Miller KM, Oetting TA, et al. Cataract in the adult eye PPP. American Academy of Ophthalmology. November 2021. Accessed February 14, 2024. www.aao.org/preferred-practice-pattern/cataract-in-adult-eye-ppp-2021-in-press. 3. Berkowitz ST, Finn AP, Parikh R, et al. Ophthalmology workforce projections in the United States, 2020 to 2035. Ophthalmology. 2024;131(2):133-9. 4. Lacy M, Kung TH, Owen JP, et al. Endophthalmitis rate in immediately sequential versus delayed sequential bilateral cataract surgery within the Intelligent Research in Sight (IRIS) Registry Data. Ophthalmology. 2022;129(2):129-38. 5. Ahmed IIK, Hill WE, Arshinoff SA. Bilateral same-day cataract surgery: an idea whose time has come #COVID-19. Ophthalmology. 2021;128(1):13-4. 6. Rush SW, Guerrero Criado AE, Kezirian GM, Durrie D. Immediate sequential bilateral cataract surgery: opinions among refractive surgeons in the United States and a comparative analysis with European consultants. J Ophthalmol. 2022:8310921. |

