 |
Q:
I recently had a keratoconus patient develop corneal hydrops. What are the risk factors? I can’t identify any except for his corneal thinning.
Hydrops can be very difficult to predict, especially because there are no universally agreed upon risk factors for its development.1 There are many different cases of hydrops with patients of differing demographics and even corneal thicknesses, explains Julie Song, OD, a Cornea and Contact Lens resident at SUNY’s College of Optometry. At this point, decreased corneal thickness is considered a risk factor, but there is no agreed-upon minimum thickness that would indicate that a patient will develop corneal hydrops.
Risks
Literature points to several potential risk factors. One such factor is vernal keratoconjunctivitis, which can potentially cause patients who have keratoconus to rub their eyes more than usual and exacerbate their condition and corneal thinning, Dr. Song notes.2-5 Other potential risk factors include asthma and atopic dermatitis.2-5
The associated conditions of dry eye disease and ocular allergies with comorbid asthma or atopic dermatitis can also exacerbate keratoconus if not properly treated, she continues. Such patients are more likely to develop hydrops from constant eye rubbing, which further increases the severity of keratoconus by thinning the cornea. Decreased best-corrected acuity associated with corneal thinning is another prevalent risk factor commonly seen in patients who develop corneal hydrops.6
Furthermore, patients with developmental disabilities are also potentially more likely to develop hydrops.2-5 This risk factor is difficult to measure but can be correlated with the prevalence of keratoconus in this population.
 |
|
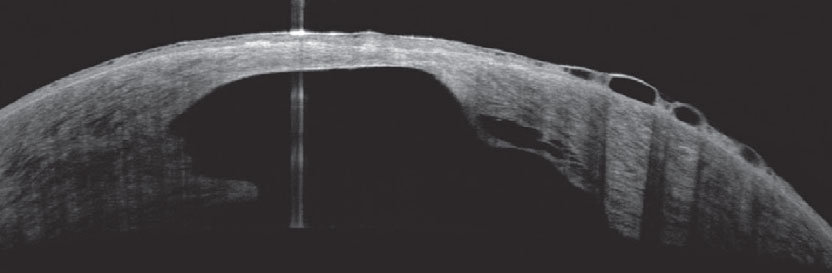
Decreased corneal thickness is the strongest predictor risk for developing hydrops. Photo: Joseph Shovlin, OD. Click image to enlarge. |
For keratoconic patients diagnosed at an young age, their condition tends to be more aggressive and can exhibit an increased likelihood of developing hydrops.3-5 In a study that evaluated the ethnic associations of developing acute corneal hydrops, it was reported that Pacific ancestry raised a patient’s risk and New Zealand European ethnicity decreased it.7 Ultimately, the literature suggests that the presence of advanced keratoconus is at the very least associated with the development of corneal hydrops, Dr. Song elucidates.
Treatment
Once hydrops has developed, the results after healing also vary patient to patient. Some patients can potentially gain improved visual acuity due to the flattening effect on the cornea, while in others acuity can decrease if central corneal scarring is severe. Hydrops heals at different rates for all patients (weeks to months), depending on the severity and patient’s comorbidities. Some will develop hydrops in one eye, with a subset of these developing hydrops in the fellow eye later on.
Due to the unpredictable nature of corneal hydrops and the lack of concrete evidence as to what definite risk factors exist, the best we can do as eyecare practitioners is to treat corneal hydrops when it does occur and advise patients to undergo corneal crosslinking or other preventative treatment early after their initial keratoconus diagnosis, advises Dr. Song. For patients who have not yet had corneal crosslinking, a conversation about its necessity should occur soon after the detection of keratoconus. Pertaining to individuals who possess any form of ocular allergies and who are also prone to rubbing their eyes, adequate patient education and treatment for the allergies must happen at the onset of their diagnosis and not once the patient has already progressed to the stage of advanced keratoconus.
“In general, it is on eyecare practitioners to work toward detecting keratoconus in a timely fashion and to recommend appropriate preventative treatment(s) before patients develop severe corneal thinning. This will result in preventing corneal hydrops as well as loss of visual acuity,” posits Dr. Song.
Dr. Shovlin, a senior optometrist at Northeastern Eye Institute in Scranton, PA, is a fellow and past president of the American Academy of Optometry and a clinical editor of Review of Optometry and Review of Cornea & Contact Lenses. He consults for Kala, Aerie, AbbVie, Novartis, Hubble and Bausch + Lomb and is on the medical advisory panel for Lentechs.
1. Maharana PK, Sharma N, Vajpayee RB. Acute corneal hydrops in keratoconus. Indian J Ophthalmol. 2013;61(8):461-4. 2. Barsam A, Brennan N, Petrushkin H, et al. Case-control study of risk factors for acute corneal hydrops in keratoconus. Br J Ophthalmol. 2017;101(4):499-502. 3. Grewal S, Laibson PR, Cohen EJ, Rapuano CJ. Acute hydrops in the corneal ectasias: associated factors and outcomes. Trans Am Ophthalmol Soc. 1999;97:187-203. 4. Tuft SJ, Gregory WM, Buckley RJ. Acute corneal hydrops in keratoconus. Ophthalmology. 1994;101(10):1738-44. 5. Basu S, Vaddavalli PK, Ramappa M, et al. Intracameral perfluoropropane gas in the treatment of acute corneal hydrops. Ophthalmology. 2011;118(5):934-9. 6. Fan Gaskin JC, Patel DV, McGhee CNJ. Acute corneal hydrops in keratoconus—new perspectives. Am J Ophthalmol. 2014;157(5):921-8. 7. Edwards M, Clover GM, Brookes N, et al. Indications for corneal transplantation in New Zealand: 1991-1999. Cornea. 2002;21(2):152-5. |

