 |
A 53-year-old man previously treated for advanced glaucoma presented with slowly progressive painless vision loss in his right eye. He had missed his visits for the past year, though he had been obtaining medication refills through his pharmacy. His vision at this visit was light perception. A year earlier, it was 20/200 and three years earlier it was 20/70 with fixation loss and profound visual field loss from glaucoma.
His recent vision reduction was due to a hypermature cataract that fully developed in the year between visits. Intraocular pressures (IOPs) were 14mm Hg OD and 16mm Hg OS. He had neither pain nor inflammation and gonioscopically his anterior chamber angles were open and normal. However, with mature and hypermature cataracts, one must be concerned about phacomorphic and phacolytic glaucoma.
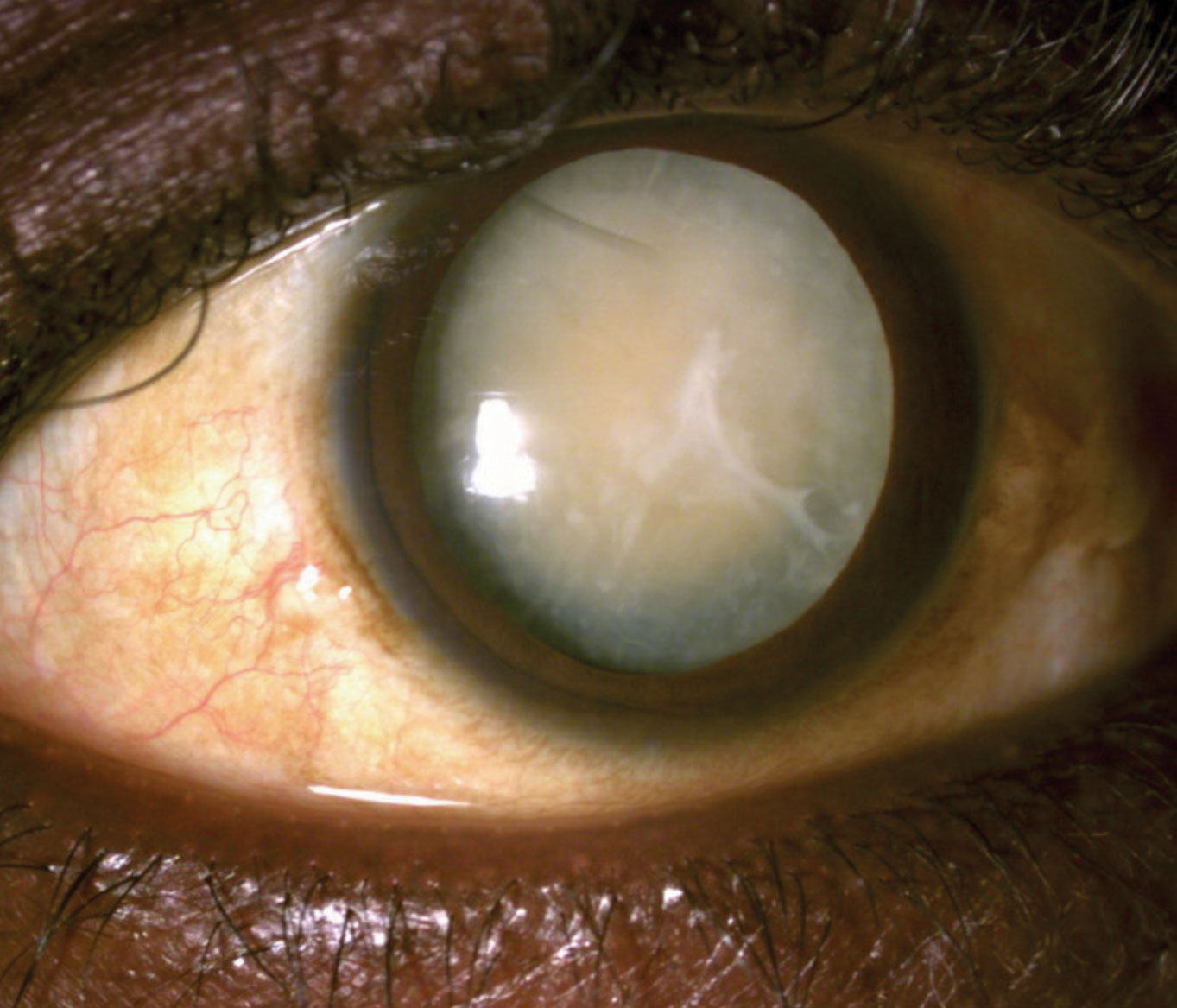 |
| This 53-year-old patient’s left eye’s vision was reduced to light perception as a result of this hypermature cataract. Click image to enlarge. |
Discussion
Upon cataract hypermaturation, the lens cortex undergoes spontaneous lysis and absorption with secondary lens nucleus shrinkage and capsule wrinkling.1-4 This allows internal lens proteins to leak out through an intact though permeable lens capsule.1-4 While the internal lens proteins are the host’s own body tissue, they have never been exposed to the anterior chamber due to their envelopment by the lens capsule. When the body detects these internal lens proteins, it interprets them as foreign and antigenic. Subsequently, a lens-induced inflammatory reaction ensues.3 A pronounced macrophage response occurs in the anterior chamber.6 Numerous macrophages containing phagocytized degenerated lens material (phacolytic cells) can be found in the anterior chamber. The lens-induced inflammation often causes a secondary rise in IOP with secondary glaucoma.
Phacolysis can be considered an innate evolutionary response to cataractogenesis. Prior to the advent of surgical lens removal, many individuals would become blind from cataracts. The subsequent lytic process and inflammatory degradation would effectively remove the visual obstruction. Unfortunately, the eye would be left aphakic and often irreparably damaged from inflammatory glaucoma. Spontaneous absorption of cataracts through the phacolytic process has been reported, which supports this evolutionary role of phacolysis.5,6 While the cataract maturation process is generally slow, once a lens has become hypermature, the phacolytic process can develop rapidly.7
Phacomorphic glaucoma typically afflicts older females, often of small stature with moderate hyperopia and a nanophthalmic eye.8 Frequently, an advanced, intumescent cataract will be present in the affected eye with commensurate reduced vision. There will be a shallow anterior chamber and possibly iris bombé. In eyes with markedly asymmetric cataract formation, the depth of the anterior chambers may be accordingly disparate. Patients may present with an acute onset of ocular redness and pain with an edematous cornea and elevated IOP, as typically seen in an angle closure attack. During an acute attack, few to no anterior chamber angle structures will be visible on gonioscopy.8-10 The resultant secondary angle closure may be either acute, subacute or chronic and can occur in eyes with previously open angles, as well as those with previously narrow, occludable angles.11-13 In chronic angle closure cases that occur from phacomorphism, no symptoms will be seen.
Treatment
When managing the inflammatory component in phacolysis, topical corticosteroids are indicated, just as they would be for any anterior uveitis.14 Cycloplegics are also indicated.14 The choice should be dictated by the severity of the uveitic response and the patient’s degree of discomfort. Typically, homatropine is an adequate choice.14
Patients with phacolysis may experience loss of zonular support to the lens, which manifests as phacodonesis.14 In cases of poor zonular support, cycloplegia with attendant pupil dilation may result in anterior dislocation of the lens, possibly into the anterior chamber. If poor zonular support to the lens is suspected, cycloplegia should be avoided.
The secondary glaucoma accompanying phacolysis is often improved by the reduction in inflammation with topical steroid therapy. However, if additional pressure reduction is necessary, clinicians may turn to aqueous suppressants, barring any systemic contraindications. Avoid miotics and prostaglandin analogs due to their propensity to aggravate the disease.14
As with acute primary angle closure glaucoma, medical therapy is initially used to acutely lower the IOP in eyes with phacomorphic glaucoma. Beta-blockers, alpha-2 adrenergic agonists, topical corticosteroids, topical or oral carbonic anhydrase inhibitors and oral hyperosmotics may be all systematically employed. An exceptional effect of prostaglandin analogs in managing the IOP of patients with chronic angle closure glaucoma both before and following LPI has been reported.15-17 In cases where pupil block precipitates the angle closure, LPI is indicated following medical treatment to attempt to relieve the resultant aqueous congestion and IOP rise. This is especially true where a relative pupil block, secondary to the unusual lens anatomy is the main pathogenesis.18
In most cases, it is necessary to remove the antigenic lens to fully manage phacolytic and phacomorphic glaucoma. Manual small-incision cataract surgery with trypan blue staining of the anterior lens capsule is a safe and effective method of cataract extraction for patients with phacolytic glaucoma, as is phacoemulsification.19 Phaco combined with anterior vitrectomy is also an option in these cases.20,21 Anecdotally, femtosecond laser-assisted cataract surgery may be a viable option.22
These hypermature lens conditions develop typically when a patient is deemed a poor candidate for surgery or otherwise cannot obtain or undergo cataract extraction. In the patient presented here, he already had longstanding severe vision loss from advanced glaucoma; thus his developing cataract was never addressed. With no future visual potential in this eye from pre-existing glaucoma, he will be monitored for the possible development of phacomorphism and phacolysis and then addressed accordingly should these complications develop.
1. Podhorecki J, Munir A. Result of operations for hyper-mature cataract complicated with phacolytic glaucoma. Klin Oczna. 2002;104(5-6):350-3. 2. Rijal AP, Karki DB. Visual outcome and IOP control after cataract surgery in lens induced glaucomas. Kathmandu Univ Med J (KUMJ). 2006;4(1):30-3. 3. Oprescu M. The etiopathology of phacoantigenic uveitis and phacolytic glaucoma. Oftalmologia 1992; 36(3):207-13. 4. Rosenbaum JT, Samples JR, Seymour B, et al. Chemotactic activity of lens proteins and the pathogenesis of phacolytic glaucoma. Arch Ophthalmol 1987;105(11):1582-4. 5. Blaise P, Duchesne B, Guillaume S, et al. Spontaneous recovery in phacolytic glaucoma. J Cataract Refract Surg. 2005;31(9):1829-30. 6. Mohan M, Bartholomew RS. Spontaneous absorption of a cataractous lens. Acta Ophthalmol Scand. 1999;77(4):476-7. 7. Sowka J, Vollmer L, Falco L. Rapid onset phacolysis. Optometry. 2004;75(9):571-6. 8. Abramson DH, Franzen LA, Coleman DJ. Pilocarpine in the presbyope: Demonstration of an effect on the anterior chamber and lens thickness. Arch Ophthalmol 1973; 89(2):100-2. 9. Gorin G. Angle closure glaucoma induced by miotics. Am J Ophthalmol 1966; 62(6):1063-6. 10. Gayton JL, Ledford JK. Angle closure glaucoma following a combined blepharoplasty and ectropion repair. Ophthal Plast Reconstr Surg. 1992;8(3):176-7. 11. Pradhan D, Hennig A, Kumar J, et al. A prospective study of 413 cases of lens-induced glaucoma in Nepal. Indian J Ophthalmol. 2001;49(2):103-7. 12. Prajna NV, Ramakrishnan R, Krishnadas R, et al. Lens induced glaucomas--visual results and risk factors for final visual acuity. Indian J Ophthalmol. 1996;44(3):149-55. 13. Angra SK, Pradhan R, Garg SP. Cataract induced glaucoma--an insight into management. Indian J Ophthalmol. 1991;39(3):97-101. 14. Sung VC, Barton K. Management of inflammatory glaucomas. Curr Opin Ophthalmol. 2004;15(2):136-40. 15. How AC, Kumar RS, Chen YM, et al. A randomised crossover study comparing bimatoprost and latanoprost in subjects with primary angle closure glaucoma. Br J Ophthalmol. 2009;93(6):782-6. 16. Chen MJ, Chen YC, Chou CK, et al. Comparison of the effects of latanoprost and bimatoprost on intraocular pressure in chronic angle-closure glaucoma. J Ocul Pharmacol Ther. 2007;23(6):559-66. 17. Chen MJ, Chen YC, Chou CK, et al. Comparison of the effects of latanoprost and travoprost on intraocular pressure in chronic angle-closure glaucoma. J Ocul Pharmacol Ther. 2006;22(6):449-54. 18. Tomey KF, al-Rajhi AA. Neodymium:YAG laser iridotomy in the initial management of phacomorphic glaucoma. Ophthalmology. 1992;99(5):660-5. 19. Venkatesh R, Tan CS, Kumar TT, et al. Safety and efficacy of manual small incision cataract surgery for phacolytic glaucoma. Br J Ophthalmol. 2007;91(3):279-81. 20. Dada T, Kumar S, Gadia R, et al. Sutureless single-port transconjunctival pars plana limited vitrectomy combined with phacoemulsification for management of phacomorphic glaucoma. J Cataract Refract Surg. 2007;33(6):951-4. 21. Miura S, Ieki Y, Ogino K, et al. Primary phacoemulsification and aspiration combined with 25-gauge single-port vitrectomy for management of acute angle closure. Eur J Ophthalmol. 2008;18(3):450-2. 22. Kránitz K, Takács AI, Gyenes A, et al. Femtosecond laser-assisted cataract surgery in management of phacomorphic glaucoma. J Refract Surg. 2013;29(9):645-8. |

