The wet form of age-related macular degeneration (AMD) affects approximately 250,000 Americans per year.1 Because severe vision loss in wet AMD is commonly associated with choroidal neovascular membranes (CNVM), scientists have gained much knowledge about how intravitreal injection may help treat CNVM and possibly improve vision. Well look at some of this knowledge here.

Diagnosis
CNVMs develop when abnormal blood vessels grow from the choriocapillaris through Bruchs membrane into the space beneath the retinal pigment epithelium.
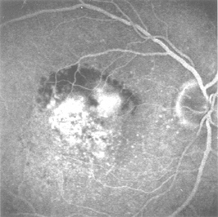
If a patient presents with sudden decreased acuity, metamorphopsia and central or paracentral scotoma, fluorescein angiography (FA) is warranted. This test helps identify the type of lesion and its location, which dictates treatment options.
There are two types of CNVMs: classic and occult. Angiography of classic CNVM exhibits discrete hyperfluorescence and late leakage. Occult CNVM shows a fluorescein pattern that exhibits a fibrovascular pigment, epithelial detachment or late leakage with a poorly defined source. (Indocyanine green angiography may allow for better views of occult CNVMs when FA images are obscured by overlying hem-orhages and exudates.)
On average, clinicians may expect 78% of CNVMs to be subfoveal, 16% juxtafoveal and 5% extrafoveal. Of the subfoveal lesions, 73% will be occult with the remainder being predominately or minimally classic.2 Two types of intravitreal injectiontriamcinolone and anti-vascular endothelial growth factormay prevent or reduce angiogenesis. These injections, described below, may therefore be useful in treating both forms of CNVMs.
Triamcinolone
Triamcinolone is a water-soluble corticosteroid that inhibits leukocytes, which release angiogenic factors. A study done at Ruprecht- Karls-University in Heidelberg, Germany, shows this injection can improve vision.3 The study included 67 patients (71 eyes) who presented with exudative AMD; 68 eyes had predominantly or total occult type, and three had classic type. All participants received an intravitreal injection of 25mg of crystalline triamcinolone acetonide.
The mean follow-up time was seven months. Visual acuity was highest one to three months after the injection, and 66% of the participants had improved vision at three months, while 11 eyes lost acuity. Six patients experienced a decrease in visual acuity after an initial increase, and they received a second injection. Meanwhile, three eyes experienced an increase in acuity.
Another study, done by Indiana School of Medicines department of ophthalmology in Indianapolis, combined the injection with photodynamic therapy (PDT). Researchers found that patients needed fewer repeat treatments of PDT when also treated with intravitreal triamcinolone.4 (For more on intravitreal triamcinolone, see Report from ARVO: Retina,)
Anti-VEGF
Intravitreal injection may help treat CNVMs in wet AMD patients.
Several studies were performed in the 1990s using interferon injections to inhibit vascular endothelial proliferation and migration on subfoveal CNVM in the laboratory. The studies, however, came up short:
A 1992 study included eight participants but helped only one idiopathic subfoveal CNVM patient.5 Patients also reported side effects of lethargy and malaise, which limited compliance among study participants.
A 1993 pilot study included 10 patients. While nine eyes showed clinical and angiographic improvements in one eye, five of the eyes still had active CNVM.6
Another 1993 study included four patients. Visual acuity stabilized in three of the patients. But, researchers pointed to a short follow-up time.7
A 1994 study of 24 patients found that the anatomic and visual status of a majority of the subjects eyes remained the same or worsened after treatment.8
Also, all the participants had adverse reactions involving multiple organ systems. Due to poor outcomes, interferon treatment was largely abandoned.
Enter the intravitreal injection of anti-VEGF. Vascular endothelial growth factor (VEGF) has been linked with the pathogenesis of retinal and subretinal neovascularization in both diabetic retinopathy and CNVM secondary to AMD. Now, anti-VEGF treatments are showing promise where interferon did not.
Phase II clinical trials for classic and occult neovascularization are very promising. One in four patients showed an improvement of three lines of acuity, and almost nine in 10 patients showed stabilization or improvement three months following the injection.9 Like triamcinolone, anti-VEGF has also been tested in combination with photodynamic therapy and has shown a significant reduction in the percentage of patients who require repeat PDT. Only 40% of patients in the combination treatment group required repeat PDT treatment, while 93% in the PDT-only control group needed repeat PDT.10
According to the National Institutes of Health, AMD is the leading cause of blindness in Americans over age 50. As such, we must be vigilant in staying on top of not only the latest pharmacologic interventions mentioned above, but all AMD treatment options.
1. Spaide RF, Sorenson J, Maranan L. Combined photodynamic therapy with verteporfin and intravitreal triamcinolone acetonide for choroidal neovascularization. Ophthalmol 2003;Aug;
110(8):1517-25.
2. Olsen TW, Feng X, Kasper TJ, et al. Fluorescein angiographic lesion type frequency in neovascular age-related macular degeneration. Ophthalmol 2004;Feb;111(2):250-255.
3. Jonas JB, Kreissig I, Hugger P, et al. Intravitreal triamcinolone acetonide for
exudative age related macular degeneration. Br J Ophthalmol 2003 Apr;87(4):462-68.
4. Rechtman E, Danis RP, Pratt LM, Harris A. Intravitreal triamcinolone with photodynamic therapy for subfoveal choroid neovascularisation in age related macular degeneration. Br J Ophthal 2004 Mar;88(3):344-7.
5. Loughnan MS, Heriot WJ, ODay J. Treatment of subfoveal choroidal neovascular membranes with systemic interferon-alpha 2a. Aust N Z J Ophthalmol 1992 Aug;20(3):173-5.
6. Kirkpatrick JN, Dick AD, Forrester JV. Clinical experience with interferon alfa-2a for exudate age-related macular degeneration. Br J Ophthalmol 1993 Dec;77(12): 766-70.
7. Tholen A, Kain H, Messmer E.Treatment of age-associated macular degeneration with interferon-alfa-2a. Ophthalmologe 1993 Jun;90(3):279-82.
8. Chan CK, Kempin SJ, Noble SK, Palmer GA. The treatment of choroidal neovascular membranes by alpha interferon. An efficacy and toxicity study. Ophthalmology 1994 Feb;101
(2):289-300.
9. Eyetech Study Group. Anti-vascular endothelial growth factor therapy for subfoveal choroidal neovascularization secondary to age-related macular degeneration: phase II study results. Ophthalmology 2003 May;110(5):979-86.
10. (TAP) Study Group. Photodynamic therapy of subfoveal choroidal neovascularization in age-related macular degeneration with verteporfin: one-year results of 2 randomized clinical trials TAP Report 1. Treatment of Age-related Macular Degeneration with Photodynamic Therapy. Arch Ophthalmol 1999;Oct.117(10):1329-45.

