 |
|
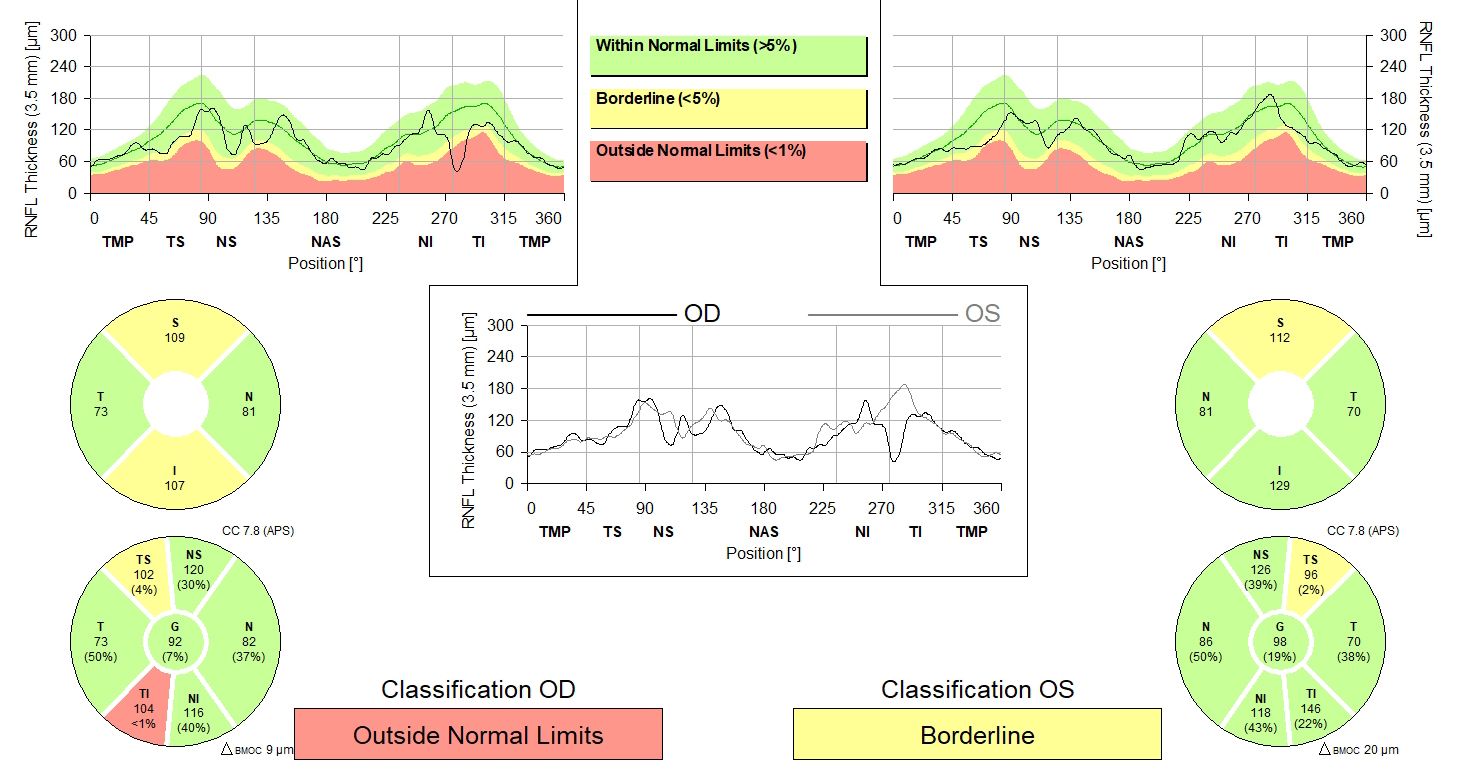
Higher IOP variability was independently associated with RNFL thinning rate in patients with glaucoma. Photo: Heidelberg. Click image to enlarge. |
Elevated intraocular pressure (IOP), as the only clinically modifiable risk factor for the progression of open-angle glaucoma, plays an outsized role in the management of this disease. However, the specific mechanisms of IOP’s influence has yet to be elucidated, as open-angle glaucoma has been found to develop across a wide spectrum of IOP profiles.
A recent study evaluated the association between long-term IOP variability and OCT-based rates of retinal nerve fiber layer (RNFL) thinning, an objective measure that quantifies the retinal structural damage in patients with glaucoma. The team also investigated IOP variability, mean IOP and peak IOP to compare each parameter’s association with the rate of RNFL thinning. They determined that IOP variability was independently associated with structural change in patients with glaucoma, even after adjusting for mean IOP, supporting its potential value in clinical management.1
In this retrospective analysis of a longitudinal cohort, patients were enrolled from the Diagnostic Innovations in Glaucoma study and the African Descent and Glaucoma Evaluation study. Eyes with at least four visits and two years of follow-up OCT and IOP were included. A total of 815 eyes (564 with perimetric glaucoma, 251 preperimetric) from 508 patients with imaging were followed for a mean of 6.3 years. Of the 508 included patients, 55.3% were Caucasian, 38.4% were African American, 4.7% were Asian and 1.6% were another race or ethnicity.1
Higher IOP variability was independently associated with RNFL thinning rate in patients with glaucoma. The mean rate of RNFL change was -0.67μm per year. In multivariable models adjusted for mean IOP and other confounding factors, a faster annual rate of RNFL thinning was associated with a higher standard deviation of IOP (-0.20μm per 1mm Hg) or larger IOP range (-0.05μm per 1mm Hg). When both mean IOP and IOP variability were higher, RNFL thinning was faster.1
The researchers noted that the majority of patients with perimetric glaucoma had mild glaucoma based on visual field mean deviation. As such, their results may not be applicable to patients with more advanced glaucoma, although the study population can reflect the patient population in most glaucoma clinics. They also stated, “The patients who exhibited glaucomatous progression and may have been treated medically to achieve lower IOP were not excluded, which may have affected study results.”1
A commentary to the article published in JAMA Ophthalmology discussed the study’s assessment of the somewhat greater influence of variability in IOP rather than mean IOP in the rate of RNFL loss and its suggestion that clinicians should pay attention to IOP variability when making clinical decisions.2
“Patient data were not censored for pressure values obtained after glaucomatous progression, when likely the medical treatment was increased to achieve a lower pressure with a consequently misleading appearance of greater overall variability,” the commenter wrote. “Risk factors should only be analyzed up to the point of an outcome.”
The writer of the commentary also suggested that “perhaps the correlations with IOP factors would be more robust if the inclusion criteria were further limited to those on only medical treatment and excluding those with a history of filtering surgery, laser trabeculoplasty and interim cataract surgery, all of which were associated with a slower RNFL thinning over time in the study.”
“Patients with primary open-angle glaucoma with early damage whose pressures are consistently reduced by 30% and in the normal IOP range usually do quite well, and those with advanced disease in whom the pressures are consistently below 15mm Hg also usually do well,” the author wrote. “It is in those in whom those targets are not easily met that it would be good to have more clues about who has higher risk and in whom more frequent monitoring or further treatment should be considered.”2
1. Nishida T, Moghimi S, Chang AC, et al. Association of intraocular pressure with retinal nerve fiber layer thinning in patients with glaucoma. JAMA Ophthalmol. October 27, 2022. [Epub ahead of print]. 2. Palmberg PF. What is it about intraocular pressure that matters in glaucoma progression? JAMA Ophthalmol. October 27, 2022. [Epub ahead of print]. |

