 |
Referrals are a critical aspect of optometric practice, even among ODs who practice to the full extent of their license. Therefore, they must be prepared to collaborate with specialists while maintaining their position as the primary eye care provider. This involves offering detailed recommendations to any specialist to whom they are entrusting their patient’s care.
“The role of the OD as the manager of their patients’ vision and medical eye wellness is a critical component of optometry that has been taken on by our profession very appropriately over the last decade or so,” notes James Thimons, OD, of Ophthalmic Consultants of Connecticut.
Comanagement ConnectionsCheck out other articles in this series: Be a Retina Referral Rock Star The Many Layers of Cornea Comanagement |
“Your patients have chosen you as their primary eye care provider, the individual who will serve their best interests and needs,” he emphasizes. “One way we do this is by knowing when to refer to a specialist. The concept of shared patient care has become the standard that we live by.”
Why is a collaborative approach important? First and foremost, the quality of care provided to the patient is—in most cases—markedly better, according to Dr. Thimons. It offers patients convenience as well as the ongoing support of the primary eye care provider they know and trust.
For optometrists, it keeps them connected to the patient’s medical care while providing the additional benefit of an extra set of eyes. It also offers an avenue for professional development. ODs can use this relationship to grow their skills as well as their practice.
“Glaucoma is a disease that involves a lifetime of continued management,” says Dr. Thimons. “And so, the comanagement of these patients is very different than the episodic relationship we see with other diseases. It is much more intimate and evolved. It is also the one—in my opinion—with the highest level of responsibility but also holds the greatest rewards.”
 |
|
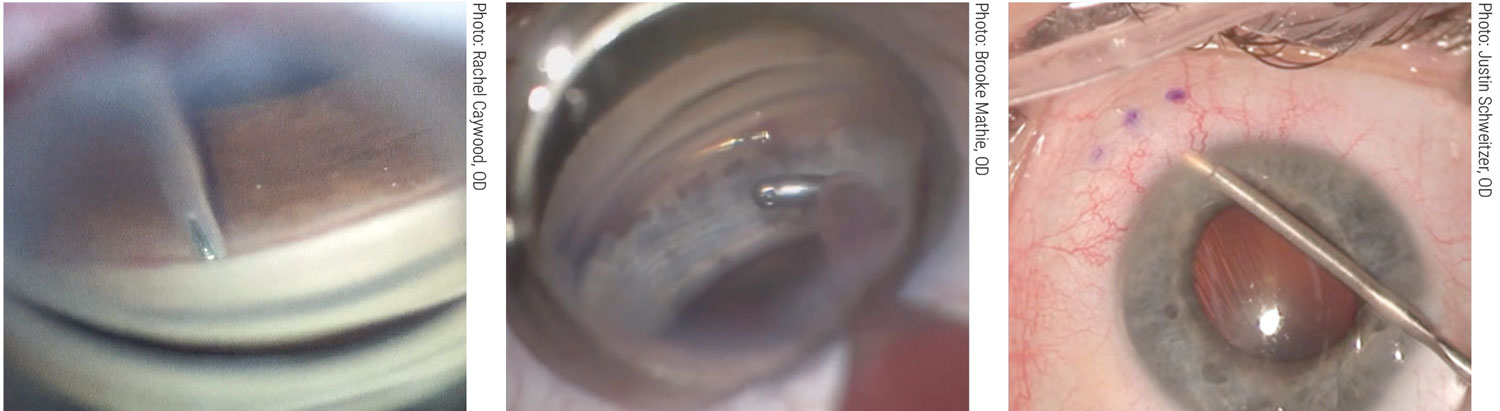
A stent for all occasions. Left to right: iStent Inject (Glaukos), Hydrus Microstent (Ivantis), Xen gel stent (Allergan). ODs should be well-versed in the uses of these and other options to play a part—perhaps a decisive one—in the timing and selection of a MIGS procedure. Click images to enlarge. |
Establishing Relationships and Effective Communication
Successful collaboration depends on the skills of both the optometrist and specialist as well as a strong relationship founded in mutual trust and respect. This is especially true when it comes to glaucoma—a chronic condition that requires ongoing care and close comanagement.
Collaborative care begins by fostering connections in your community. “Connecting or meeting with surgeons in the area is a great first start to build a relationship,” suggests Abagail Kirk, OD, of Memphis. “It’s important for an optometrist to introduce him or herself to the new ophthalmic community they are joining,” and that includes both other optometrists and ophthalmologists, she notes.
“At my practice, we have a dedicated community outreach team that meets and introduces new optometrists in the area to our practice and mission,” she continues. “This way, the optometrist feels welcomed and already has the names and numbers of specialists that can participate in patient care.”
When choosing the right glaucoma surgeon—or any comanagement partner—there are a number of factors to take into consideration, including training and expertise. Another critical component is making sure you are working with someone who aligns with your practice.
“Connecting with someone who shares your philosophies when it comes to glaucoma management is key,” notes Dr. Thimons. “What you don’t want is to join forces with someone whose approach conflicts with your own; this can only be derived through discussion.”
Dr. Thimons also recommends that you spend time with them, particularly in the OR, if possible. “That’s the best place to observe their skills while also getting a sense of how they interface with patients. Do they match or complement your style? Will your patients feel comfortable with this person?”
Once you have connected with a glaucoma surgeon, building a strong relationship that includes effective communication is critical. You have to feel comfortable with how you work together and exchange information. “Comanagement is successful when it involves partners who value one another,” Dr. Thimons emphasizes. “Open lines of communication ensure you are both on the same page and that the patient receives seamless, high-quality care.”
 |
|
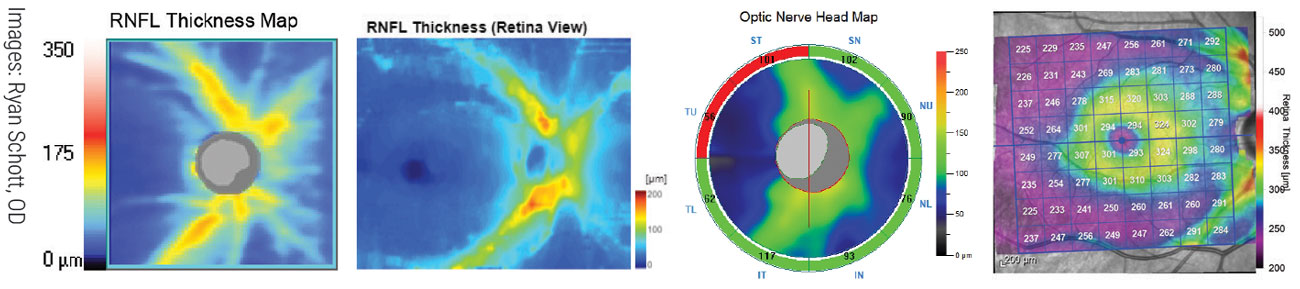
Understanding the fundamentals of OCT use in glaucoma is now an essential part of care and greatly extends the OD’s ability to manage cases themselves prior to referral. Shown here are four RNFL thickness maps of the same patient on different platforms, from an analysis Review of Optometry published in February 2020; it can be found on the website. From left to right: Zeiss Cirrus 6000, Topcon Maestro2, Optovue Avanti, Heidelberg Spectralis. Click images to enlarge. |
Optimizing Your Approach to Glaucoma
Unlike some other ocular conditions for which there’s a clear need to comanage—such as cataracts—glaucoma is a lifelong disease that will most likely require ongoing collaboration. Therefore, ODs must have the knowledge and skills necessary to optimize not only the care they provide as an individual, but also their work as a comanagement team.
While the breadth of an optometrist’s glaucoma management depends on the state in which they practice, all ODs have the authority and expertise to medically manage these patients.
How a glaucoma case is handled really depends on the stage of the disease at diagnosis. If the patient has mild glaucoma and is older at the time of diagnosis, they may never need surgery, notes Houston glaucoma expert Danica Marrelli, OD. In those cases, she may not need to comanage with a glaucoma surgeon at all.
“If I have a patient who can be managed medically, there’s no reason to involve an ophthalmologist,” she emphasizes. “On the other hand, if I have a younger patient or the diagnosis is more severe, I will begin my comanagement relationship earlier. I’ll discuss the need for potential laser or surgical interventions with my patient and I may get a consultation with the surgeon sooner.”
Managing medications includes understanding when adjustments need to be made to a patient’s treatment regimen and which medications work well together. “There’s a tendency for optometrists to prescribe one medication and then, if the patient’s not well-controlled, to send them to an ophthalmologist,” notes Dr. Marrelli, while suggesting that this may be premature. “If needed, I am more than capable of prescribing multiple medications to a patient and monitoring them appropriately.”
However, that does not mean you withhold interventions that could benefit your patients, she remarks. Medication does not work for every patient and there are a variety of reasons they may not adhere to medical therapy. In those cases, Dr Marrelli stresses the need for additional interventions. “You don’t want to hold on to your patient just to hold on to them,” she notes. “But I also don’t think there is a significant reason to involve ophthalmology if a patient can be successfully managed with medicine.”
Another important aspect of glaucoma management is minimally invasive glaucoma surgery (MIGS), which has dramatically lowered the threshold for surgical consideration. The comanagement for these procedures is typically very straightforward, notes Michael Chaglasian, OD, of Illinois College of Optometry. The challenge can be building your knowledge and understanding of the wide variety of MIGS procedures available.
“This can be confusing and sometimes overwhelming,” Dr. Chaglasian acknowledges. “Educating yourself takes time and experience, but it is an important aspect of care that ODs need to feel comfortable discussing with their patients and managing with specialists.”
It is also important to recognize that not every glaucoma and cataract surgeon performs every MIGS procedure. Therefore, ODs must communicate with the specialists in their area and determine if that individual is trained to perform the procedure that is the best fit for your patient, notes Dr. Chaglasian.
The increasing reliance on selective laser trabeculoplasty (SLT) earlier in the course of glaucoma adds another opportunity for OD-MD comanagement before the disease advances. Increasingly, it’s the primary care optometrist who initiates discussions about SLT as an alternative to medications at the outset of care, and weighs in on the decision in conjunction with the patient and surgeon.
As with any referral, making sure all members of the care team are on the same page is vital to success. Just as the OD must share detailed information and recommendations, they must also be aware of the glaucoma surgeon’s process. Optometrists should ask for the surgeon’s pre-op protocols for all of the many different procedures they perform so they know which medications the patient will be on before or after surgery, suggests Dr. Kirk.
“For example, we start patients on acetazolamide (if there are no contraindications) and prednisolone acetate 1% prior to having Xen Gel Stent surgery, to reduce IOP spikes during or after the procedure and to cut down on post-op inflammation leading to potential scarring of the bleb later,” she explains. “If cleared by cardiology, we may stop blood thinners to lower the chance of developing a hyphema. At day one post-op intraocular pressure, we adjust the medications accordingly to avoid hypotony.”
Postoperatively, ODs can and should manage their patients. “Optometrists are more than capable of treating and managing glaucoma post-surgical interference; the data we collect and assess is the same,” notes Dr. Kirk. “If the intraocular pressure is not reaching the expected outcome following glaucoma surgery, then communicate that to the surgeon.”
Effective comanagement following surgery starts on day one post-op. “Assess the incisions, levels of inflammation and edema, the appearance of the bleb (if applicable) and the intraocular pressure,” she outlines. “Becoming familiar with what is normal makes it much easier to catch those rare occasions that are abnormal.”
Seeing the patient post-op in the morning is also important, Dr. Kirk advises. Some patients may be in pain while others may not have picked up their post-op drops like they were supposed to and will need to go to the pharmacy. “Sending an emergency back to the surgeon is much easier to do if you catch it in the morning vs. late afternoon,” she notes.
“Having a basic understanding of the procedures available via research, attending a CE or asking the surgeon is not just important but imperative to your confidence and ability to accurately continue certain treatments,” Dr. Kirk emphasizes.
Effective patient communication is also vital to glaucoma comanagement. This begins by helping patients understand the process. Setting expectations when it comes to potential interventions prior to sending them to an ophthalmologist is extremely helpful, according to Dr. Kirk. “A patient that already comes in with an understanding of what to expect shows the surgeon they can trust your assessment of your patients, which streamlines the consultative process and sets the patient up for success.”
Addressing Gaps and Challenges
A critical aspect of glaucoma management is knowing when to escalate from medical to surgical intervention. Navigating this requires that ODs have confidence in their skills and expertise as well as a strong relationship with the glaucoma surgeon.
To avoid under- or over-referral, the optometrist must identify the appropriate target pressure for their patient from the onset of diagnosis, suggests Dr. Chaglasian. “Keeping track of that target pressure and whether or not you have achieved it is key,” he says.
“Simultaneously, you should be tracking your patient for progressive changes to the visual field and OCT,” he continues. “Any evidence of progression is an indicator that you are not at target pressure and further treatment is necessary, which could entail a number of different approaches such as SLT or MIGS.”
Successfully determining the timing of a referral comes down to tracking a patient appropriately during the medical treatment phase, emphasizes Dr. Chaglasian. While identifying progression in glaucoma is more challenging than other conditions due to the diagnostics required, it is well within the skills of an OD, he notes.
“Many glaucoma specialists are not interested in managing straightforward medical glaucoma, Dr. Chaglasian explains. “They want to work with optometrists who are willing to take on this aspect of care; when done well, this represents a true comanagement partnership.”
In Dr. Kirk’s practice, few of the glaucoma evaluations she sees are unwarranted. “Unfortunately, my experience is usually the opposite,” she says. “I see a handful of patients present with severe or end-stage glaucoma only using latanoprost 0.005% when they can remember to take it.
“These cases are the toughest,” she adds. “Seeing an established patient referred in for glaucoma surgery when drops had been failing for decades and now the only option is a tube is disheartening.”
It is important that ODs think long-term when strategizing for these patients, Dr. Kirk notes. The question to ask themselves is, “How can I keep this patient seeing as much field as possible for the rest of his or her life?”
There are many new devices and surgical procedures that are low-risk, low-anxiety experiences for the patient, and ODs need to be well-versed in their indications and outcomes, she explains. “SLT is a safe and easy treatment, implantation of iStent inject or Hydrus Microstent during cataract surgery are very easily implantable and can lower intraocular pressures up to 30% which adds little to no extra time in the operating room.”
Another area that requires attention is gonioscopy, which, according to Dr. Thimons, is not used as frequently as it should be among both optometrists and ophthalmologists. “Gonioscopy should be used regularly for patients with open-angle glaucoma.” Over time, the angle may begin to narrow and that can go unrecognized without the proper assessment, he says.
“Long-term progression analysis is at the heart of glaucoma therapy,” Dr. Thimons says. “And it’s quite critical that people incorporate technologies at the highest level possible, which is not always the case. It is also important that we don’t default to newer technologies in replacement of previous ones—like gonioscopy—that remain essential to glaucoma care.”
REFERRAL LETTER TIPS FOR THE OD
• Share pertinent patient information (i.e., history of non-adherence; well-controlled on meds; narrow angle). • Make recommendations based on your knowledge of the patient. • Outline the comanagement relationship you expect to have with the specialist. |
Challenges and Gaps
Recognizing when and when not to refer to a retina specialist is an important, yet challenging, aspect of optometric practice.
One example is diabetic retinopathy. In these cases, the OD should first determine the severity. And then, no matter the stage, the optometrist must identify if diabetic macular edema (DME) is present, notes Paul Chous, OD, an expert in diabetes and diabetic eye disease from Tacoma, WA. “Retina specialists don’t need to see patients with mild, nonproliferative diabetic retinopathy without any diabetic macular edema,” he explains, noting that in those cases ODs should monitor patients for progression and counsel on the importance of individually optimized metabolic control, which is far more important in early rather than later-stage diabetic retinal disease.
As the disease progresses and moves beyond moderate severity in nonproliferative cases, the likelihood of patients developing a vision-threatening complication like proliferative diabetic retinopathy or center-involved DME increases dramatically, according to Dr. Chous. Therefore, it is critical that ODs are well-versed in the staging criteria and have the knowledge to monitor and refer these patients appropriately.
For DME, it is recommended that ODs send the patient to a retina specialist; however, Dr. Chous notes, there is a role for the optometrist, especially among patients who require observation and not immediate treatment, such as non–center involved DME or center involved DME with normal visual acuity. To make this determination and diagnose accurately, Dr. Chous says an OD must have access to an OCT.
“I would encourage every optometrist seeing patients with diabetes to have an OCT, but if they don’t, working with a nearby optometric colleague who does can be very helpful and spare patients an unnecessary visit to a retina specialist’s office,” he explains, noting this is also an opportunity to get another opinion on whether or not that patient should be referred to a specialist.
One condition that is often referred unnecessarily to ophthalmology is retinal artery occlusions. These patients, in particular those with branch retinal artery occlusions, do not need retinal surgery, Dr. Fanelli says, noting that they will need an internal medicine or vascular work-up.
In these cases, the OD can and should begin the initial workup by assessing the stroke risk of the patient (medical history, medications, carotid auscultation) and make the determination of whether the patient needs immediate referral to a stroke center or the emergency department for carotid and cerebral imaging, explains Dr. Fanelli. If the artery occlusion appears more to be related to fibrin deposits, then cardiology involvement is necessary.
This is also true for retinal vein occlusion without macular edema. Patients with retinal vein occlusions need evaluation of those etiologies that precipitate occlusion, such as poorly controlled hypertension, atherosclerosis and diabetes, or in patients without retinal vascular evidence of the above, perhaps evaluation of coagulability, notes Dr. Fanelli.
“If we’re going to market ourselves as frontline eye care providers, we can’t just cherry-pick the easy cases and manage those,” Dr. Fanelli urges. “We must create a culture of, ‘It’s OK to treat corneal ulcers on the visual axis, it’s OK to manage vein occlusion and so on, because I know what I’m doing and I’m comfortable with that.’”
Optometrists must also step up and be more forthcoming about discussing prevention. “We are the primary eye care providers and it behooves all of us in optometry to talk to our patients about preventing retinal disease,” says Dr. Chous. “We have the chance to educate our patients on the benefits of healthy lifestyle choices and encourage them to make a change.”
“From a comanaging perspective, I inform the retina specialist that I have advised the patient on lifestyle management of the retinal disease, including better diet, exercise, smoking cessation, compliance with sleep therapy and other prudent lifestyle changes,” he explains.
Here again the strength of your relationship with longstanding patients may make you uniquely well-positioned to discuss such things. An ophthalmologist with no prior relationship and level of trust with a new patient may have a harder time of it.
 |
Skill-building is critical, especially in glaucoma. The Optometric Glaucoma Society’s website offers many educational resources teaching basic and advanced techniques, plus information about upcoming meetings and networking opportunities. Click image to enlarge. |
Continued Growth and Development
Optimizing your glaucoma management depends on your ongoing growth as a provider of optometric care. There are a number of ways to do this, and comanagement in and of itself is a means for professional development. It is an opportunity for ODs to enhance their glaucoma management skills and take a more active role in the management of these patients.
“Managing cases with the help of a specialist allows optometrists to expand their knowledge and skill,” explains Dr. Thimons. “Next time, instead of referring that type of case, you may now have the confidence to manage it on your own. True comanagement is a teaching opportunity between professionals, which is what medicine should be when it’s at its best.”
When looking to improve and grow your glaucoma management skills, it is important to familiarize yourself with current procedures and devices, notes Dr. Kirk. “For instance, there is a wealth of free knowledge on the very hot topic of MIGS right now,” she says. “Watch videos of the techniques and see how they are performed. It would behoove your clinical decision making and your patients’ well-being to stay up to date.”
Professional organizations are another excellent resource for education and support. “Whether through mentorship or continuing education, there are a number of ways for optometrists to enhance their skills,” notes Dr. Marrelli. “For instance, the Optometric Glaucoma Society offers a non-CE credit series where small groups of glaucoma experts and doctors meet to discuss cases.”
Key Takeaways
• Actively share your recommendations with the glaucoma surgeon when referring patients. • Open lines of communication between practices is essential when comanaging patients. • Educate your patients and set expectations prior to sending them to a specialist. • Comanagement is an opportunity to learn. Take advantage of this to enhance your skills and build your confidence. |
Glaucoma management is a crucial component of optometric practice, and it is well within the ODs scope of practice to medically manage these cases. To do so successfully, optometrists must dedicate their time to not only enhancing their skills, but also building a strong comanagement relationship where they take the lead as the primary eye care provider.
Building the foundation for effective glaucoma management—and comanagement—takes an ongoing effort. This includes embracing additional responsibilities within your scope of practice; however, this can and should be done at your own pace.
“I am so excited for Massachusetts and the recent Texas glaucoma law,” notes Dr. Marrelli. “But the truth is, just because a law goes into effect doesn’t mean that the optometrist is ready to start this process. However, they also shouldn’t be intimidated either. Comfort and confidence come with time.
“I would encourage ODs to reach out to fellow optometrists who are actively managing glaucoma,” she notes. “They are very willing to walk alongside those who may want to start, but just don’t quite know how. Taking that first step can be overwhelming, but there are a variety of resources available, and optometrists are well-equipped to take charge when it comes to caring for these patients.”

