|
The practice of medicine is a collaborative effort and optometry is no exception. As we discussed in the first installment of this series, comanagement plays a critical role in healthcare delivery and, as primary eyecare providers, ODs should be at the helm of the referral relationship.
While comanaging cornea cases is not as commonplace as with cataract patients, it remains an important relationship that every optometrist should have in their network. Understanding how to leverage collaborative efforts is beneficial for both patients and practice.
Annual Cornea ReportCheck out these articles: Skip the Scalpel? A Medical Approach to Endo Recovery |
First and foremost is the convenience for patients. In many cases, the best cornea specialist is not always the closest. Comanagement ensures patients receive specialized care while also having the support of their primary optometrist, eliminating the need for unnecessary travel.
“Comanagement allows patients to obtain the most specialized care while maintaining a meaningful relationship with their local optometrist, who has fostered their care for years,” notes Katelyn Lucas, OD, of Price Vision Group, a large cornea specialty practice in Indianapolis. “It also allows the optometrist to see the cornea in the early phase so that they can better determine if issues arise such as rejection, wound dehiscence, increased inflammation or other problems that can occur over time.
 |
|
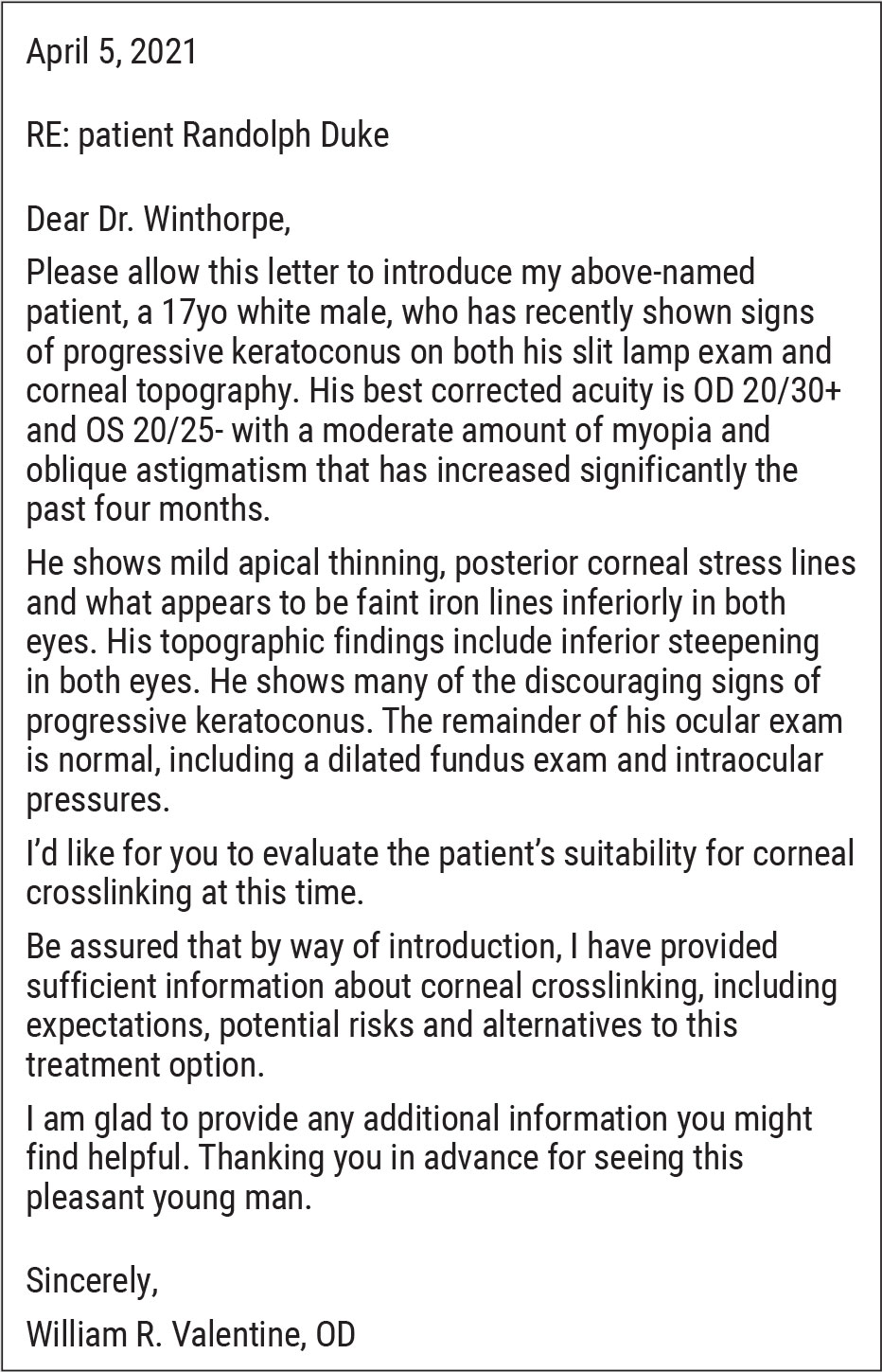
Foreign body cases are one area where it’s crucial for optometrists to take the lead in initiating urgent care to the full extent of their skills and scope of practice. This is a patient’s cornea immediately after removal of a metallic foreign body but prior to rust ring removal. The object was superficial enough that it was removed with a sterile cotton swab after anesthetizing the patient’s eye. Click image to enlarge. |
“With cornea surgeries, especially transplants, lack of follow-up can lead to loss of graft and even permanent vision loss due to steroid induced glaucoma, immunologic rejections or infections,” she continues. “Getting in for a timely exam when problems arise is critical in taking care of corneal transplants, and having a doctor convenient to their location allows for prompt medical attention.”
Comanagement ConnectionsCheck out other articles in this series: Be a Retina Referral Rock Star |
This second installment of our comanagement series will delve into cornea management and ways to help ODs enhance their referral relationships. We will take a closer look at the role of optometry in closing the practice gaps that often exist in this category. Comanagement is not only a way to provide comprehensive patient care; when done successfully, it also can elevate individual practices and the profession as a whole.
Optimizing Cornea Management
Cornea care encompasses a host of conditions and therapeutic interventions; therefore, comanagement can vary greatly depending on the patient’s individual needs. However, no matter the procedure, optimal patient outcomes depend on effective collaboration.
 |
|
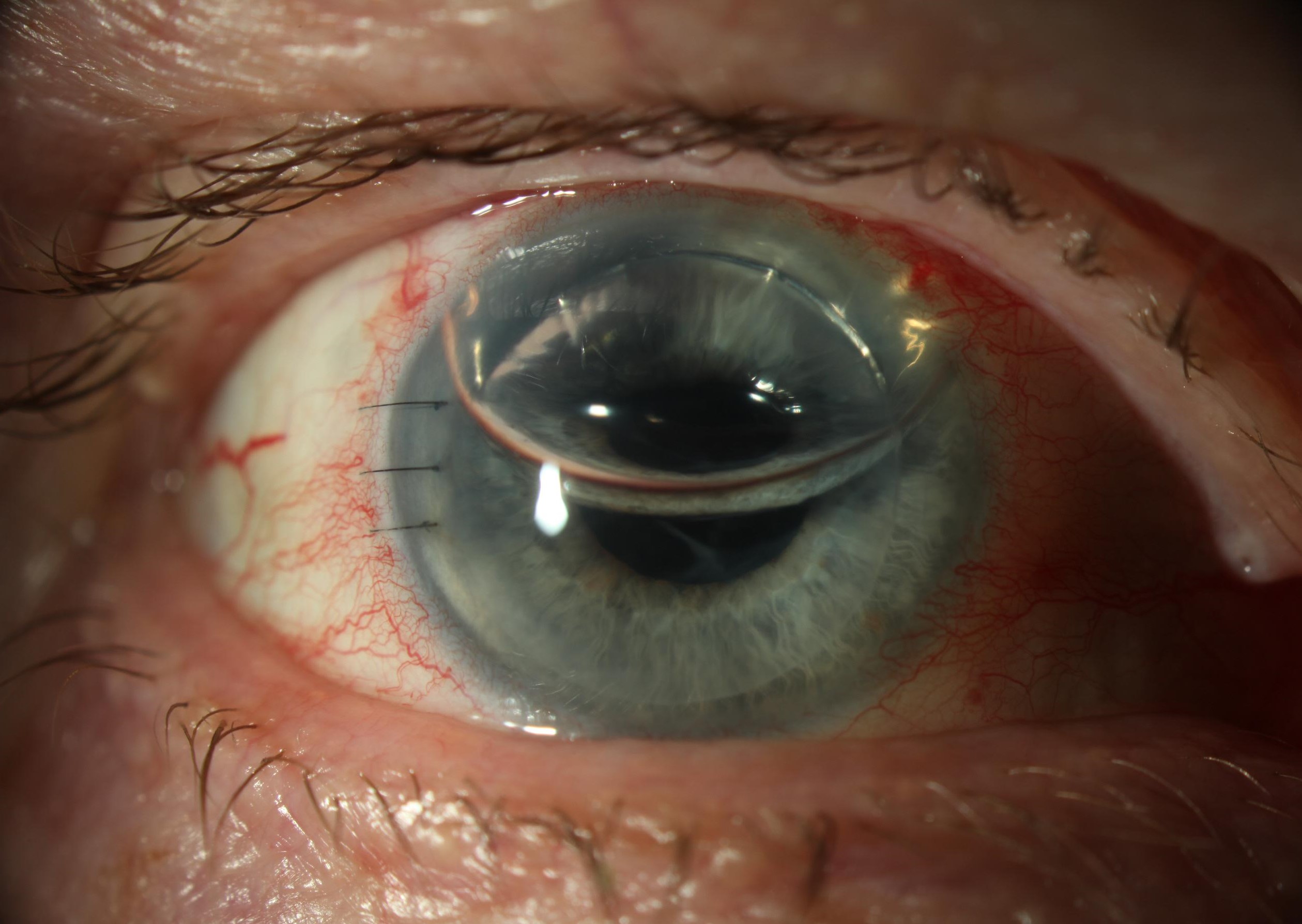
This is a patient one day post-DSAEK. For both DSAEK and DMEK, the transplants are supported by the air bubble in the anterior chamber. Both transplant types require supine positioning that can be difficult for people with spinal problems, and they suffer from periodic early dislocation of the graft, but in this case the eye and transplant are healing well. Click image to enlarge. |
“Surface procedures, such as phototherapeutic keratectomy (PTK), superficial keratectomy and corneal crosslinking (CXL), lend themselves well to comanagement between optometry and ophthalmology,” notes Mitch Ibach, OD, of Vance Thompson Vision, a large anterior segment surgical practice in Sioux Falls, SD. “Patients are still going to need some type of vision rehabilitation afterwards and optometrists are in the position to take the lead following surgery.
Investing in TechnologyComprehensive cornea care and comanagement of these conditions depends on a number of factors, including having the right tools at your disposal. “Corneal topography or tomography should be the next equipment primary optometrists embrace,” notes Dr. Ibach. “Cornea care should be in the hands of optometry and that is much easier to do when you have the right tools.” It is imperative that ODs have a way to measure the curvature of the cornea, according to Dr. Ibach, who suggests some type of auto or manual keratometry if they do not have a topographer. Other tools that could be helpful, but don’t necessarily need to be available at your practice, include a specular microscope and, on rare occasions, confocal microscopy, according to Dr. Shovlin. “These are not essential to your practice, but they can be very helpful and may be something you want available to you through your referral source.” |
Intraocular corneal surgeries (or, more broadly, transplantations) do not follow the path of traditional comanagement, he explains. “The majority of early post-op management—the first three months or more—occurs at the surgical center due to the delicate nature of the follow-up care. The primary referring OD often takes over post-op care in most cases later than in other, less invasive procedures.”
When a corneal transplant patient returns to their optometrist can vary and usually depends on how the surgical center handles postoperative care. However, the optometrist’s work begins well before surgery. Preparing the ocular surface for corneal surgery is an important preoperative step in maximizing healing, notes Dr. Ibach.
“Careful documentation of preoperative acuities is essential as well as a detailed assessment of the corneal condition,” says Joseph Shovlin, OD, also at a large multispecialty practice with emphasis on anterior segment care. “Optometrists should report any other comorbidities or potential problems.
“A lot of these patients will have secondary issues, such as glaucoma,” he explains. “Some patients have lid disease that may be the driver for the corneal problem; therefore, careful documentation of the cornea and adnexa is key.”
One of the most important responsibilities of the OD is managing patient expectations. “You don’t want someone going to a cornea specialist expecting a 20/20 outcome when that might not be possible,” notes Dr. Shovlin. “Given their longstanding relationship, patients trust their optometrists to prepare them for any procedure, but this is especially important for an intimidating surgery like corneal transplant.”
While the surgical center will be more involved in postoperative care for corneal transplants and other invasive procedures, optometrists have an important role to play and should be included in all aspects of care.
“All corneal transplants need to be followed on a regular basis to monitor for rejection and steroid response which can be done with the comanaging optometrist,” says Dr. Lucas. “This helps ensure the success of optometry practices and improves the doctor-patient bond.
“Early post-op visits done with an optometrist also allows for a ‘second objective opinion,’” she notes. “A good comanaging surgeon values this as they can be unconsciously biased from seeing a complication in their work.”
Infection is always a concern postoperatively, notes Dr. Shovlin. “Depending on when you see the patient, you always have to make sure that the cornea is compact, and be sure to look for signs of early infection and rejection,” he says. “As time goes on, graft failure is a concern and it’s very important to monitor intraocular pressures as well as monitor for lens changes with needed prolonged steroid use.”
Dr. Lucas recommends reviewing the ophthalmology practice’s comanagement packet, which typically contains instructions for post-op visit frequency, necessary testing and medication changes. Familiarizing yourself with medication schedules and tapers from the surgical center helps improve consistency and outcomes, emphasizes Dr. Ibach.
No matter the type of procedure, communication between providers is essential. “Effective comanagement requires regular communication between the referring OD and the surgeon, especially if there are any questions,” Dr. Lucas reiterates. “There’s no such thing as a stupid question. Optometrists need to feel comfortable enough to be able to ask questions about the care of their shared patients or how to handle a particular group of patients.”
Open lines of communication also help ensure the necessary follow-up occurs. “Failure to return for follow up visits is a risk; however, regular communication between physicians as well as improved understanding of one another’s scheduling preferences can help combat this issue,” Dr. Lucas suggests.
Taking the Lead
As the ranks of optometrists grow, ODs are in the position to take even more of a leadership role across the continuum of eye care. Beyond surgical procedures, there are other areas of cornea care that can often be handled solely by the optometrist.
There are a variety of ways ODs can take the lead, but two in particular are dry eye and corneal erosions, suggests Dr. Ibach. “Dry eye is definitely a space where optometrists want to do absolutely as much medical treatment as they can for those patients,” he says. “More specific to cornea, recurrent erosions are another.”
If a patient has a corneal erosion, it could be trauma- or dry eye–induced and a one-time event, he explains. “An optometrist can treat that patient in the office with topical antibiotics, lubrication and anti-inflammatories; often, a bandage contact lens or amniotic membrane will help for healing, too.” If it begins to become recurrent, then a referral may be necessary, but “if it’s just the first corneal abrasion or erosion, you don’t always have to send that off for a superficial keratectomy or PTK, especially if the optometrist is comfortable with these conditions.”
A number of clinical entities, such as microbial keratitis, require medical intervention rather than surgery and are well within an optometrist’s scope of practice. Why might an OD opt to send these cases to a specialist? For many, it comes down to what they are comfortable with and their experience with these cases.
How to Write a Referral LetterProviding detailed patient information lays the foundation for effective comanagement. Here is an example of a referral letter that will set you, your patient and the ophthalmologist up for success.
|
“Comanagement looks different depending on your practice. Some generalists are comfortable managing an array of issues—ranging from corneal debridement for patients who have recurring erosion to treating corneal infections—and will only refer when they need a corneal transplant or lamellar surgery,” says Dr. Shovlin. “On the other end of the spectrum are optometrists who prefer to refer any cornea-related issues for confirmation of a diagnosis and appropriate treatment.
“Confidence comes with experience,” he notes. “It’s a matter of seeing enough patients with a particular condition to feel comfortable managing their care. Spend time observing and learning so you can take on cases that are within your scope of practice. I would welcome anyone to come to our practice and spend a day or two with me and our corneal specialists.” Dr. Shovlin practices in Scranton, PA.
Continuing Education
Whether you’re an OD who wants to start expanding your cornea care or a seasoned clinician looking to take your expertise to the next level, there are number of ways to enhance your practice and become more comfortable caring for these patients.
“Optometrists should actively seek continuing education on current corneal practices, specifically with corneal specialists within their geographic area,” suggests Dr. Lucas. “These events are a good way to hear about new developments in their practice regarding patient care or new technology being used.”
In the time of COVID-19, there is no shortage of online offerings, notes Dr. Ibach. “I always recommend our national meetings, such as the American Academy of Optometry or American Optometric Association. There are also myriad regional meetings and focused optometric groups,” he says. “Many groups have a virtual library of accredited courses that can help you improve your practice.”
A strong relationship with the surgical practice you refer to can also be beneficial to your professional growth. “Oftentimes, just jumping on the phone or even going in and spending a couple hours with the surgeon can be an excellent way to learn,” Dr. Ibach explains.
“Given the broad range of potential cornea conditions and procedures, everyone is not going to be comfortable comanaging every single one,” Dr. Shovlin states. “It is important to know your comfort level and not overextend yourself because that’s not good for you or the patient.”
 |
|
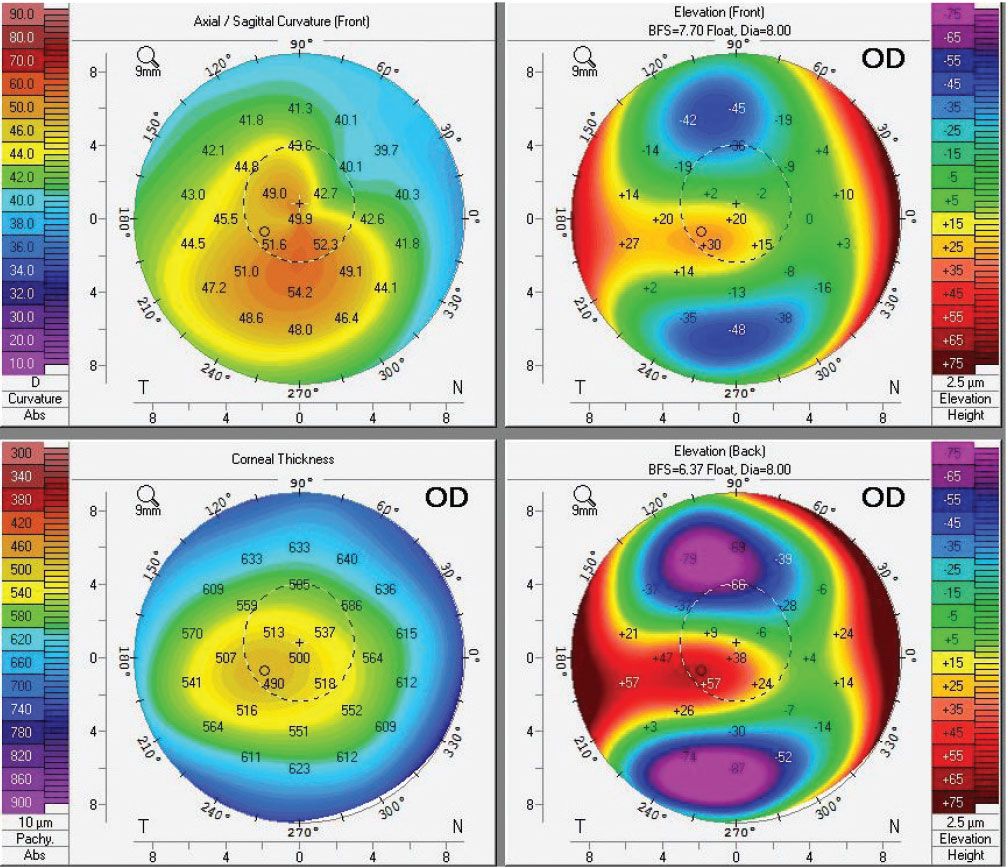
Despite moderate keratoconus, this eye sees relatively well with glasses at 20/25-. Fortunately for the patient, the primary OD was suspicious for keratoconus due to high astigmatism and a reduction in best-corrected acuity and sent them for evaluation The Pentacam shows deviations with topography, pachymetry, and anterior and posterior elevations that makes the diagnosis clear cut. The patient was able to be crosslinked and maintains good acuity because their primary OD managed the eye perfectly. Click image to enlarge. |
That being said, “don’t be afraid to expand your knowledge and skills,” he continues. “Find a colleague—this can be a specialist or a local optometrist who has a special interest in the cornea—who can help guide you clinically so next time you see that particular condition you are more comfortable managing the patient.”
Addressing Gaps in Care
While advances in cornea management continue, challenges remain, and optometrists are uniquely positioned to tackle these difficulties and fill any gaps in care.
One area where optometrists can have significant impact is keratoconus. With the advent of corneal crosslinking, these patients now have an available intervention that could change the course of their disease. However, many patients are not receiving this treatment as soon as they could.
“With corneal crosslinking being an emerging area in the field, focusing our attention on diagnosing keratoconus as early as possible and providing treatment will ensure the best possible outcomes for patients,” says Aaron Bronner, OD, of Pacific Cataract and Laser Institute, a large OD-MD multidisciplinary practice in the Northwest. “This requires a shift in professional screening for this disease. We have usually just let them develop organically because there hasn’t been a way to stop progression.
“When keratoconus gets bad enough it becomes apparent and the diagnosis is easy, but what we want to do at this point is identify the condition before it becomes really apparent,” he continues, noting that this requires the appropriate screening tools. “The Pentacam (Oculus) is a very good device that can diagnose keratoconus at stages way before the patient has symptoms.”
If an optometrist has a patient with findings consistent with the condition, such as dramatically increasing astigmatism or not correcting to 20/20 with glasses, they can use this device to confirm their suspicions, suggests Dr. Bronner, who acknowledges this technology may not be available in every optometry practice due to cost constraints.
“If you don’t have the device at your clinic, you can send them to the surgery center that comanages with you for testing only,” he notes. “It doesn’t have to be a full referral and is a cost-effective approach to diagnosing a problem.”
Key TakeawaysWhile cornea comanagement can vary greatly depending on the condition and procedure, it is an essential aspect of care. Here are a few takeaways to help you partner with surgeons more effectively:
|
Another potentially challenging but important aspect of care is knowing when to make a referral, particularly when it comes to a procedure like corneal transplant. “Although there have been improvements thanks to DSEK/DMEK, corneal transplants are still challenging procedures with a greater risk of complication than routine procedures like cataract surgery,” says Dr. Bronner. “Therefore, you wouldn’t recommend this surgery at the first signs of endothelial disease. Instead, waiting for the condition to progress somewhat is important.”
“Keep in mind, the risk of DSAEK and DMEK are lower than traditional PK, but higher than say cataract surgery. Because of that, you’ll want to see a bit more VA reduction prior to a surgical referral than you would for a routine cataract operation,” he explains. “Of course, any corneal comanagement center will be happy to see your patient as early in the disease process as you like, but one of the most critical aspects of comanagement is the patient hearing a consistent message from both the referring doctor and the surgery center. Therefore, early referrals should be accompanied by more guarded recommendations for surgery.”
Depending on how you handle comanagement, it can have a positive or negative impact on your patient relationships. “An important part of the patient relationship is the long-term trust that’s been built over time,” notes Dr. Ibach. “That can be put in jeopardy if you don’t thoroughly educate a patient on your findings prior to referring to a specialist.”
Clinical Pearls• For corneal crosslinking, PTK and superficial keratectomy patients, the first decision is when the epithelial defect has resolved and timing of the bandage contact lens removal. • Among CXL patients, it is very common to see a thinning/condensing of the pachymetry after treatment with an initial steepening of corneal topography in the first one to six months. This is expected due to epithelial remodeling and shouldn’t cause concern, according to Dr. Ibach. • Contact lenses play an important role in vision recovery after penetrating and deep anterior lamellar keratoplasties, Dr. Lucas notes. “Fitting specialty contact lenses can be lucrative for optometry practices and help increase contact lens referrals from cornea specialists.” |
For instance, if a patient is “diagnosed” with basement membrane dystrophy or keratoconus at the surgical center, but they were referred for a different condition, it can cause them to doubt their primary eye care provider and be hesitant to return to their practice for postoperative care, according to Dr. Ibach. “Oftentimes, the OD did see and diagnose this problem, but didn’t discuss it with the patient prior to referral,” he explains. “As a result, there is potential for trust to breakdown between the patient and maybe even the comanaging ophthalmologist.”
An ongoing commitment to growing as a healthcare provider, both individually and in collaboration with ophthalmologists, is invaluable to not only for patients, but the profession at large.
“Our ophthalmology colleagues are staying pretty even in number while the patients who need care only continues to grow,” notes Dr. Ibach. “The more that we as optometrists can help facilitate pre- and postoperative management, the more opportunity we’re going to have for our surgical partners to take care of patients from a surgical standpoint.
“Comanagement is also a practice builder. Providing exceptional care can lead to referrals not just from patients, but also the ophthalmologists you work with,” he concludes. “Collaboration, when done well, elevates both patients and their providers.”