 |
A 34-year-old male from Venezuela presented to our tertiary care center with a two-day history of redness, photophobia and worsening vision in his left eye. He was asymptomatic in his right eye. His past ocular history was significant for at least one similar episode in the left eye eight years prior.
His visual acuity was 20/20 OD and 20/150 OS with no pinhole improvement. Pupils were equally round and reactive without a relative afferent pupillary defect. His confrontation visual fields were full to careful finger counting, and there were no extraocular motility restrictions. His intraocular pressures were 18mm Hg OD and 13mm Hg OS.
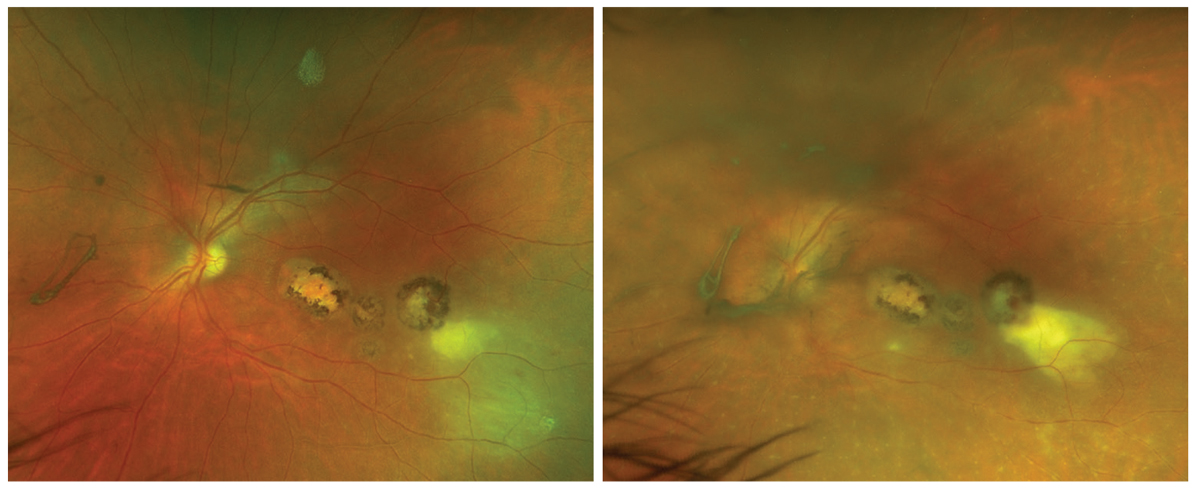
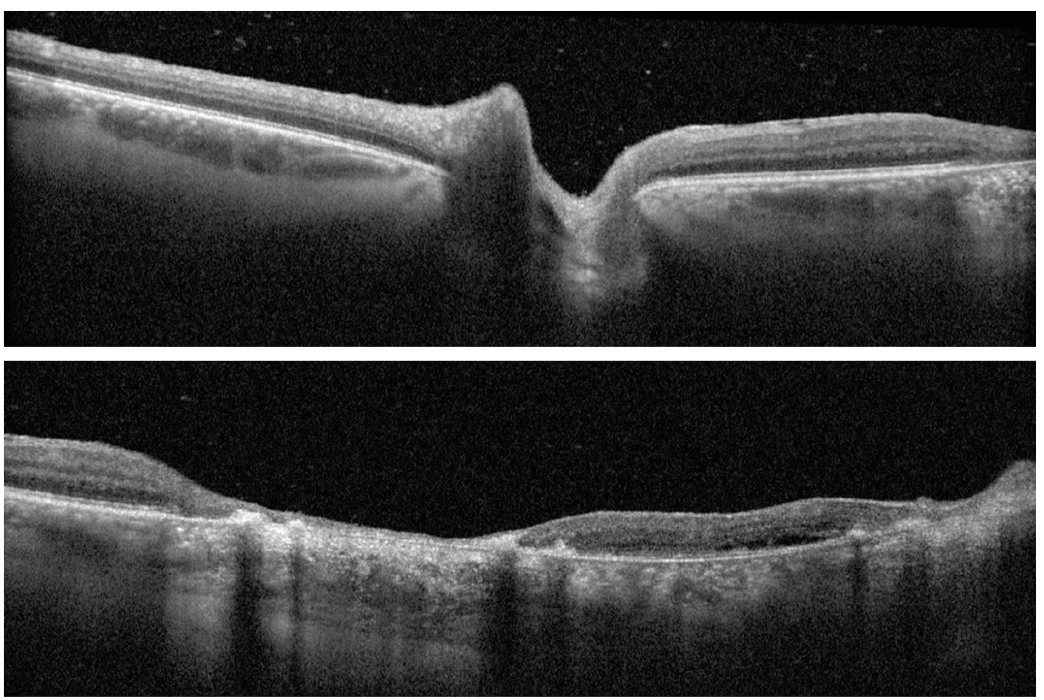
Fundus photos and OCT images are available for review (Figures 1-4). Slit lamp examination was unremarkable OD; OS, there was 2+ diffuse conjunctival hyperemia with limbal flush and 2+ anterior chamber cell. There were also trace posterior vitreous cells with mild posterior vitreous haze (Figure 3).
 |
|
Figs. 1 and 2. Ultra-widefield photo of the left eye on presentation and on follow-up four days later. Click image to enlarge. |
Take the Retina Quiz
Take the Retina Quiz
1. Which of the following is false regarding Figures 3 and 4?
a. There are posterior vitreous cells.
b. There is papillitis.
c. There is multifocal outer-retinal and retinal pigment epithelium (RPE) atrophy of the macula.
d. There are outer-retinal cystic changes of the macula.
2. What is the most likely diagnosis?
a. Syphilis.
b. Toxoplasmosis.
c. Tuberculosis.
d. Viral retinitis.
3. Which treatment option is most appropriate for this patient?
a. Oral sulfamethoxazole/trimetho-prim and clindamycin.
b. Triple therapy (oral pyrimethamine, sulfadiazine, prednisone and folinic acid supplementation).
c. Triple therapy plus oral clindamycin.
d. All of the above are reasonable treatment options.
4. Which of the following is true regarding the diagnosis of this patient?
a. It must be confirmed with serologic studies.
b. It is primarily a non-granulomatous anterior uveitis with posterior spillover.
c. It is the most common cause of posterior uveitis worldwide.
d. The primary site of infection is the choroid.
5. Which of the following is not a typical feature of the patient’s condition?
a. Dense vitritis.
b. Papillitis.
c. Posterior or panuveitis.
d. Preseptal cellulitis.
 |
|
Figs. 3 and 4. Spectralis OCT of the left optic nerve and left macula. Click image to enlarge. |
Diagnosis
Fundus exam OS revealed multifocal pigmented macular scars involving the fovea (Figures 1 and 4). There was a presumably new, hypopigmented lesion in the temporal macula with more prominent overlying vitritis adjacent to the strand of hyperpigmented lesions. There was no retinal vasculitis or papillitis at that time (Figure 1).
His panuveitis was representative of a reactivation of toxoplasmosis. Posterior uveitis serology was obtained, and serum T. gondii IgG titers were elevated with PCR confirmation of T. gondii DNA, which also ruled out viral causes of necrotizing retinitis.
Discussion
Ocular toxoplasmosis is the most common cause of posterior uveitis and is secondary to T. gondii, an obligate intracellular protozoan.1 Patients tend to present with blurred vision, floaters and photophobia.1 Clinical findings of ocular toxoplasmosis may include a posterior or panuveitis with diffuse or focal vitritis, papillitis, macular edema, retinal hemorrhage and retinal vasculitis/segmental retinal arteritis.1,2
Ocular toxoplasmosis is characterized by a unilateral focal area of necrotizing granulomatous retinochoroiditis obscured by overlying vitritis, classically termed as a “headlight in the fog.”1,2 There may be adjacent hyperpigmented chorioretinal scars.1,2
Infection most commonly occurs in the retina and RPE, but tissue cysts (bradyzoites) have also been isolated in other ocular structures, including the choroid, vitreous, iris and optic nerve.1,2
Segmental retinal arteritis is characterized as periarterial exudates and intra-arterial plaques that may resemble retinal emboli.2 It can be present anywhere in the fundus and is otherwise a benign finding. This generally resolves without sequelae but can persist for months even after clinical resolution of intraocular inflammation.3-5
As the retinochoroiditis resolves, the disorganization of the retinal layers and hyperpigmentation produces the appearance of an inactive toxoplasmosis scar.2 The typical presentation of congenital toxoplasmosis is a unilateral macular scar.2 Reactivation can be seen in up to two-thirds of patients and often occurs adjacent to the site of primary infection due to the rupture of intraretinal cysts and local immune reaction.1,2,6 Decreased visual function secondary to toxoplasmosis is typically related to macular or optic nerve involvement.1
Diagnosis is primarily clinical (no serologic confirmation required) but can be supported by lab testing.1,2,7 Elevated serum IgG antibodies confirm past exposure but low titers do not rule it out.1,2 Also, IgM titers may not be elevated at initial presentation.1,2,7
Treatment
Tissue cysts are impenetrable by current anti-toxoplasmic drugs and can remain viable indefinitely.1 Still, toxoplasmosis is a self-limiting condition with treatment aimed at minimizing structural damage by modulating the inflammatory response.1,2,6 Treatment is recommended for all immunocompromised patients as well as immunocompetent patients with lesions in the posterior pole, adjacent to the optic disc or larger than two-disc diameters.6,8
“Triple therapy” for the treatment of toxoplasmosis includes the use of pyrimethamine, sulfadiazine and oral prednisone. Pyrimethamine requires folinic acid supplementation to prevent aplastic anemia 1,2,6,9 Bactrim DS (sulfamethoxazole 800mg and trimethoprim 160mg, Roche Pharmaceuticals) has a safer side effect profile compared with triple therapy, but its efficacy has been questioned. Long-term systemic prophylaxis with Bactrim DS can be considered in high-risk patients.10 Clindamycin injections may be useful in recalcitrant cases.1,6
Patient Care
There was macular involvement in our patient, and he was started on oral Bactrim DS two times daily, oral clindamycin 300mg three times daily, topical prednisolone acetate 1% every two hours OS and atropine sulfate 1% two times daily in the left eye.
He returned four days later for follow-up and demonstrated worsening of intraocular inflammation. There was increased vitritis, enlargement of the retinal lesion and new retinal vasculitis/segmental retinal arteritis (Figure 2). This prompted anterior chamber paracentesis to send an aqueous humor sample for polymerase chain reaction as well as administration of an intravitreal injection of clindamycin.
The patient responded well to the adjuvant treatment and was later started on oral prednisone. He achieved quiescence but was continued on prophylactic Bactrim DS given his history of recurrence with macular involvement.
Retina Quiz Answers
1: b, 2: b, 3: d, 4: c, 5: d
Special thanks to Alberta Pengo, who helped contribute to this case. Alberta is a fourth-year optometry extern from New England College of Optometry.
Dr. Aboumourad currently practices at Bascom Palmer Eye Institute in Miami. He has no financial disclosures.
Dr. Dunbar is the director of optometric services and optometry residency supervisor at the Bascom Palmer Eye Institute at the University of Miami. He is a founding member of the Optometric Glaucoma Society and the Optometric Retina Society. Dr. Dunbar is a consultant for Carl Zeiss Meditec, Allergan, Regeneron and Genentech.
1. Schachat AP, Wilkinson CP, Hinton DR, et al. Ryan’s Retina, 6th Edition. Elsevier. 2018. 2. Gass JDM. Stereoscopic atlas of macular disease : a fundoscopic and angiographic presentation. Saint Louis: Mosby, 1970. 3. Chazalon E, Conrath J, Ridings B, Matonti F. Kyrieleis arteritis: report of two cases and literature review. J Fr Ophtalmol. 2013;36(3):191-6. 4. Meier PG, Herbort CP, Jr., Wolfensberger TJ. Spectral domain optical coherence tomography for the characterization of kyrieleis exudates involving both the fovea and retinal vessels. Klin Monbl Augenheilkd. 2016;233(4):545-6. 5. Pichi F, Veronese C, Lembo A, et al. New appraisals of Kyrieleis plaques: a multimodal imaging study. Br J Ophthalmol 2017;101(3):316-21. 6. Yanoff M, Duker J. Ophthalmology, 5th Edition. Elsevier. 2019. 7. Fekkar A, Bodaghi B, Touafek F, et al. Comparison of immunoblotting, calculation of the Goldmann-Witmer coefficient and real-time PCR using aqueous humor samples for diagnosis of ocular toxoplasmosis. J Clin Microbiol. 2008;46(6):1965-7. 8. Holland GN, Lewis KG. An update on current practices in the management of ocular toxoplasmosis. Am J Ophthalmol. 2002;134(1):102-14. 9. Eyles DE, Coleman N. Antibiotics in the treatment of toxoplasmosis. Am J Trop Med Hyg. 1953;2(1):64-9. 10. Fernandes Felix JP, Cavalcanti Lira RP, Grupenmacher AT, et al. Long-term results of trimethoprim-sulfamethoxazole vs. placebo to reduce the risk of recurrent toxoplasma gondii retinochoroiditis. Am J Ophthalmol. 2020;213:195-202. |

