 |
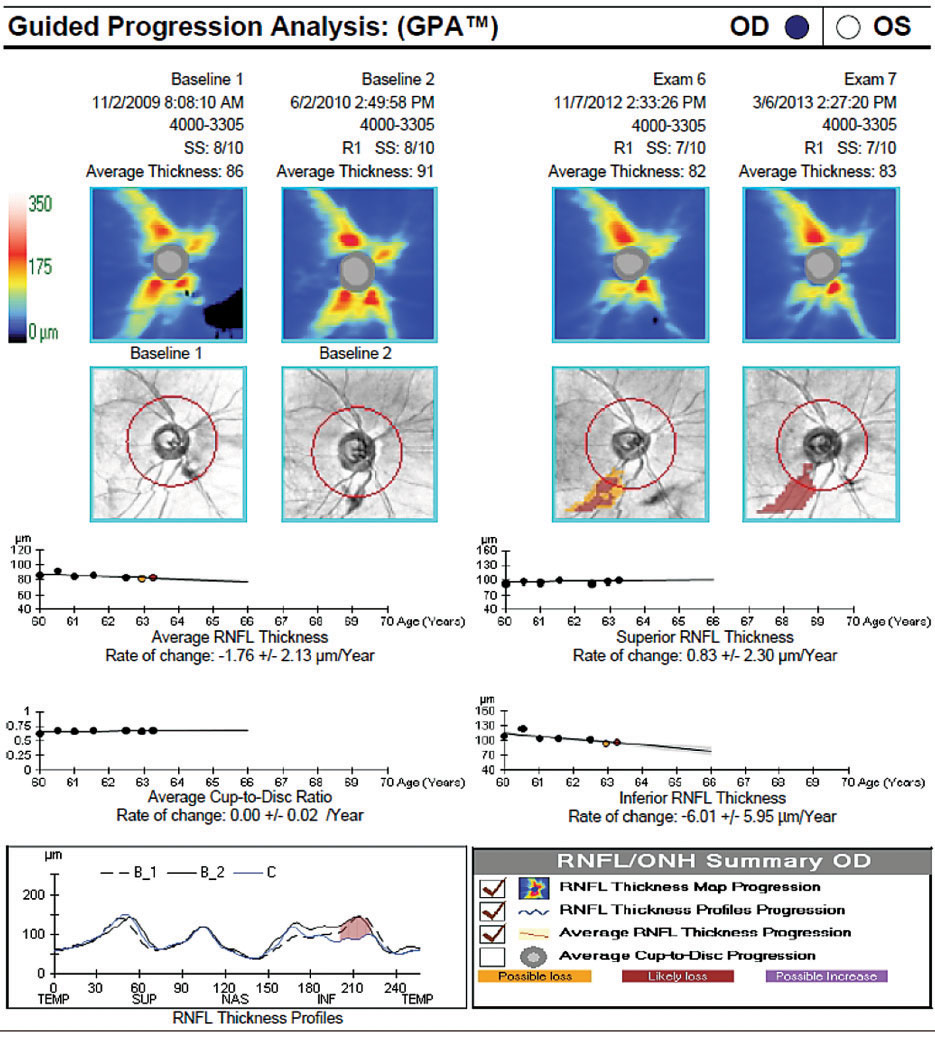
| It’s hypothesized by the authors of the study that neuroaxonal loss is driven by additional seizure-accompanying mechanisms, mainly peri-ictal hypoperfusion and hypoxia, leading to increased blood-brain barrier permeability, glial activation, central inflammation and neuronal loss. In time, RNFL serial analysis akin to the above seen in a glaucoma patient may become a clinical tool of disease monitoring. Photo: Danica J. Marrelli, OD. Click image to enlarge. |
Add another neurological condition to the list of diseases with findings that can manifest in the retina. Clinicians already know the well-established ocular findings in dementia and Parkinson’s patients, and new research has linked retinal nerve fiber layer (RNFL) thinning to epilepsy. Recently, OCT has been proposed to help identify thinning of the peripapillary RNFL (p-RNFL) as a promising marker for cerebral neuronal loss in those with the neurological condition. It’s important to note that clinical implications have not yet been identified but one new study has aimed to systematically characterize the extent of retinal neuroaxonal loss in a wide spectrum of people with epilepsy and to evaluate the main clinical determinants.
The prospective study had researchers use spectral-domain OCT on 98 people with characterized epilepsy and 85 controls, all ranging from ages 18 to 55. Assessed were structures of all inner retinal layers and the total macula volume. The study authors found those with epilepsy (58% female) displayed significant neuroaxonal loss across all retinal layers (global-pRNFL, macular-RNFL, ganglion cell inner plexiform layer and inner nuclear layer) as well as reduced total macula volumes when compared with controls. Occurrence and frequency of tonic-clonic seizures and number of anti-seizure medications were both factors associated with the extent of neuroaxonal loss seen; this was most pronounced in men.
Elaborating on their findings for an article in the journal Epileplsia, the authors pointed to the incidence of tonic-clonic seizures as a relevant determiner of retinal neuroaxonal loss. The retinal measures of those with epilepsy but without tonic-clonic seizures did not differ from the controls, even with comparable disease duration, number of anti-seizure medications taken and were older than those experiencing tonic-clonic seizures. Instead, this group saw retinal measures in-between healthy controls and the group experiencing this seizure type, suggesting more subtle retinal changes. Adjacently, the findings suggest significant retinal neuroaxonal loss primarily happens with high disease activity and severity, as evidenced by the relationship with occurrence and frequency of tonic-clonic seizures.
The authors also believe disease activity and severity to be tied to retinal neuroaxonal loss through the association of greater number of anti-seizure medications mapping onto extent of neuroaxonal loss.
Neuroaxonal loss seen in men was more pronounced than in women, independent of age, disease duration, number of anti-seizure medications and seizure frequency. This finding establishes previous research reporting sex-specific differences in RNFL thickness in those with epilepsy and another structural MRI study that found greater vulnerability of men to experience seizure-related brain atrophy with temporal lobe epilepsy.
The clinical potential of these results is palpable but not yet fully realized, with the authors stating that “the non-invasive and economic measurement via OCT bears the potential to establish as a practical tool to inform patient management.” This would be helpful to “assess the progression rate of the neuroaxonal loss, which could help to monitor the disease activity and treatment response.”
“This could be of great importance in people who are not able to document their seizures to decide on treatment adjustments. The retinal thickness could thereby be an objective and more complex parameter than the so far used seizure frequency,” the authors concluded in their paper.
Delazer L, Bao H, Lauseker M, et al. Association between retinal thickness and disease characteristics in adult epilepsy: a cross-sectional OCT evaluation. Epilepsia Open. November 3, 2023. [Epub ahead of print]. |

