Practical Matters in Myopia ManagementWith an expanding arsenal of information, myopia can be a puzzling area of care. In this second annual Review of Optometry supplement, experts offer solutions backed by science to help you manage this growing patient population. Click here to download a PDF. Check out the other articles featured in this supplement: |
Optometrists have been masters at measuring and managing refractive error for over a century, primarily by neutralizing it optically with corrective lenses rather than viewing it as a disease amenable to modification. Sentiment began to shift, however, following the 2016 publication of Brien Holden Vision Institute’s prevalence estimates that alerted the world to a possible future in which half the global population would be myopic by 2050.1 Five years after that seminal paper, the World Council of Optometry in 2021 deemed interventional treatment for myopia to be the new standard of care.2 Whether or not you share that view, it’s clear that the profession has embraced myopia management as a viable option for many children.
Newly graduating optometrists are now equipped with the proper tools to manage myopia after completing both didactic and clinical training during their time in optometric programs. A decade ago, only a handful of schools incorporated myopia management as part of the formal optometric curriculum or offered dedicated myopia management clinics to the local communities. This article will outline how myopia management can be incorporated smoothly for practitioners in their practice as well as where to start.
 |
|
Fig. 1. Young patients can be successful in contact lenses with the proper help from parents. Click image to enlarge. |
Step 1: Be the expert
As optometrists, we are the primary gatekeepers for managing myopia. While understanding nearsightedness as a common refractive error that is correctable with optical devices is our bread and butter, it is crucial to recognize myopia as a disease and consider it a treatable condition on par with dry eye, glaucoma and countless other ocular diseases. Our ability to classify it as such signals to young patients and their parents that we are in sync with current treatment paradigms.
To get to this point, you and your staff will need to learn more about different myopia management modalities, how they work and when they are optimal for use. Fortunately, educational resources are abundant. The International Myopia Institute (myopiainstitute.org) disseminates consensus papers from experts and many industry stakeholders provide didactic materials, too. There’s also a continuously updated body of clinical peer-to-peer advice presented at Review of Myopia Management (www.reviewofmm.com), a sister publication to Review of Optometry.
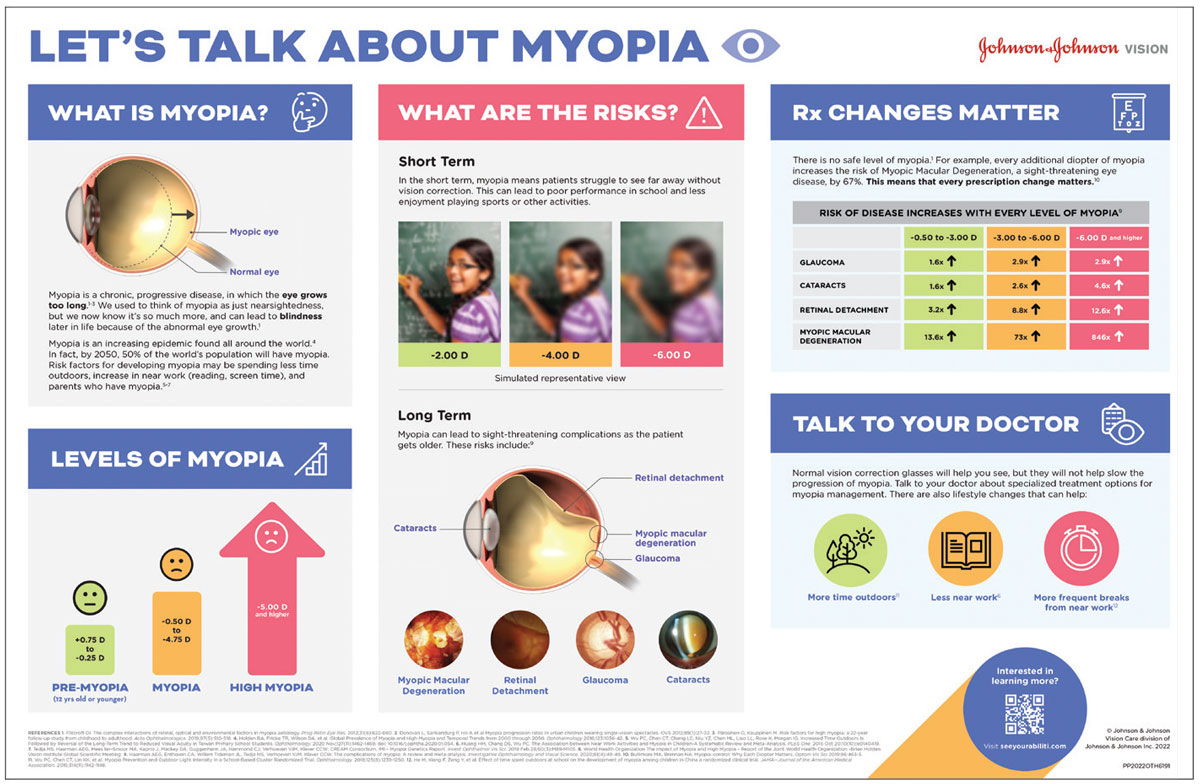
Whether you are a new grad or are an eyecare provider wanting to explore myopia management for the first time, there are plenty of CE courses, both online and live, that offer great overviews of the options currently available. Local industry meetings and downloadable resources can also be helpful to summarize our current understanding of slowing the progression of myopia (Figure 2).
 |
|
Fig. 2. This infographic aimed at parents succinctly conveys the risks of childhood myopia progression and why management should be considered. It’s available for download to use in your practice. Click image to enlarge. |
Step 2: Build a patient base
I opened a cold-start practice in February 2021 with a heavy emphasis on myopia management. The biggest challenge I faced was finding patients, but if you are already in an established practice, look no further than your existing patient base. Most EHR systems have the ability to retroactively apply search criteria. This will allow you to, for example, check for myopes under the age of 10 seen in the last year. Sending these patients’ parents an informative email or scheduling them for their annual visit is an excellent way to start their myopia management journey.
As a proactive approach, I used social media, conducted Zoom calls with concerned moms who questioned myopia management and had my local Business Improvement Area repost and share my social media posts. All it really takes to get started is a handful of patients. Their parents will tell other parents, and in a short period of time you can build a local and perhaps cross-border or even international referral network. I communicated with local health professionals—the dentist next door, local family doctors, pediatricians and even pharmacists—regarding myopia management in my practice.
Step 3: Anticipate motivators and barriers to treatment
It is imperative to set the right expectations when broaching the subject of managing myopia. Parents need to understand that their child’s myopia will likely progress no matter what; however, with treatment, we can significantly slow that progression. Do not promise complete cessation or even reversal of refractive error.
Once you have the parent(s) on board, determining which type of treatment to use is dependent on an interplay of factors. I often ask parents—or even the child—questions like, “Do you brush your teeth every day?” and “Do you make your bed every morning?” Adherence to common daily routines can determine if the child is ready for a contact lens option. Ultimately, it should be a group decision with parents, child and practitioner when deciding which modality to use.
Parents in and around my practice often have their children enrolled in extracurricular sports and see the use of ortho-K or myopia-slowing soft contact lenses as a way to simultaneously treat their child’s myopia and provide a competitive edge over spectacle lens use. Some family doctors or pediatricians may not support myopia management, but that is typically because they are unaware of it. I simply remind parents that, although these are not new treatment options, an explosion of research in recent years supports the validity of the effort and those of us in the eyecare community are best positioned to gauge their child’s viability.
The patient’s ocular surface should be free of dry eye or blepharitis if choosing a contact lens option—typically not a problem with kids—and family and social situations should be considered, too. Does the child spend time at two different homes? If so, will contact lens supplies need to be provided at both? Having this type of information on your radar will ensure that parents are capable of adherence to their child’s treatment protocol.
Step 4: Plant the seed during routine eye exams
I always like to reference the age-expected refractive norms for children when they receive an eye exam. The CLEERE study found that future myopia by age 13 is highly likely in children with refraction below +0.75D by the age of six to seven years.3 These are the children who should be closely watched. Consider shorter intervals between eye examinations as well as behavioral advice on optimizing the child’s visual environment (i.e., the well-known recommendations of more outdoor time and less screen time).
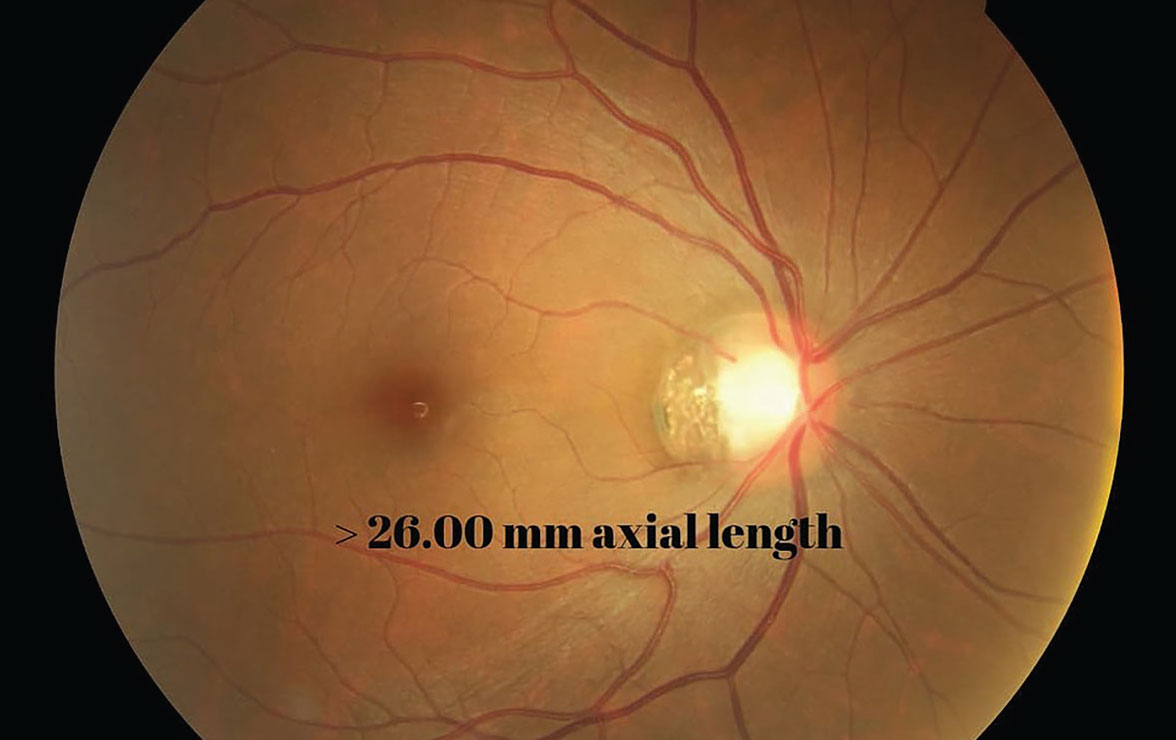
For most new myopes, and definitely those with an esophoric posture, I will dilate them to confirm their prescription under cycloplegic conditions. Suppose the child is premyopic, meaning they are quickly on their way to losing their protective plus power. In that case, I will combine this factor with parental myopia and myopiagenic environmental factors to determine my treatment plan. Use an eye model or draw a sketch to show how cataracts and compromised retinal health can become greater risks with high myopia. Some parents will have no idea what you are talking about, while others will be on the ball and ask you if their child has progressed.
Step 5: Dedicate time to communicate
For parents who have not heard of myopia management—and barely understand myopia itself—it is vital to take your time to relay the critical information. There will be skeptics, but the more data you can provide, the higher the likelihood they will at least consider the value of starting myopia treatment. Educational tools such as normative growth curves and refractive error prediction algorithms can be useful, especially if incorporated into instrumentation that can track patient data over time. The Myopia Calculator from the Brien Holden Vision Institute allows you to enter a patient’s age, ethnicity, refractive error and prospective myopia management treatment. The calculator will estimate the level of expected myopia with or without treatment.3
In my patient scheduling, I use a dedicated myopia management consultation time-slot of 15 to 30 minutes to confirm the prescription, take axial length measurements and discuss risks, which is also where the calculator might come in handy to present both treated and untreated courses of action. With the focused consultation, there is time for all questions to be answered, and I also will follow up with an email to summarize the visit. This can be directly from you or a staff member who is dedicated to dealing with myopia management questions in your office. If the patient is referred in, completing reports back to the referring doctor reinforces referral loop closures and possibly secures future referrals.
Step 6: Present all options
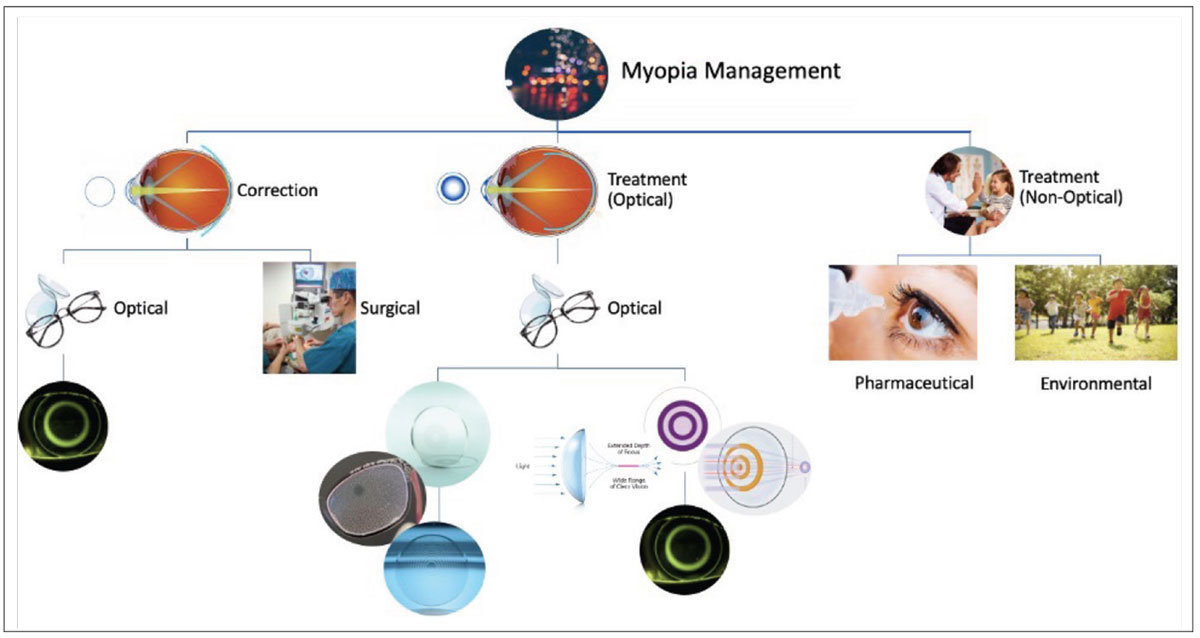
Managing myopia is great in its versatility; many options are possible. It is important to communicate all options, whether they be optical, pharmaceutical, environmental or behavioral lifestyle modifications. I love displaying the flowchart in Figure 3 on a screen and reviewing it with parents.
Regarding corrective lens modalities, contact lenses and spectacles lenses (available in Canada but not yet approved in the US) are the main first-line treatment options. Either off-label multifocal, approved dual-focus or orthokeratology (ortho-K) lenses can work effectively, as countless studies demonstrate. Optometrists in the US can use CooperVision’s MiSight contact lenses on-label or VTI’s NaturalVue lenses off-label. In Canada, we also have access to a dual-focus lens from Johnson & Johnson Vision called Acuvue Abiliti 1-Day, which uses a unique, ring-focused optical design. Also marketed in Canada but not yet the US are three spectacle lens options: Hoya’s MiyoSmart, Essilor’s Stellest and, most recently, Zeiss’s MyoCare.
Forthcoming in the pipeline is CooperVision’s SightGlass Vision MiSight spectacles. These lenses will use a different optical principle than traditional contact or spectacle lenses for myopia, which induce peripheral blur to blunt the signal that stimulates axial elongation.4 Instead, SightGlass MiSight spectacle lenses will use a concept the manufacturer calls “diffusion optics technology” (DOT). The DOT concept differs by decreasing contrast sensitivity instead of inducing peripheral blur.5 Since high contrast has been shown to cause myopia progression, this decrease may potentially slow down its course.6
Although dual-focus contacts and spectacles are different physical forms of vision correction, the two modalities offer comparable efficacy, hovering around 50% slowing of myopia.7,8 The three spectacle options available in Canada also achieve nearly the same efficacy. Rather than competing, both contact lens and spectacle lens interventions offer a greater level of customized care that can be tailored to each patient’s needs. Despite the deep penetration of myopia management seen with contact lenses because of their established availability in recent years, spectacle use so far has taken over a significant portion of pediatric contact lens wearers in my practice, achieving about a 50/50 split between modalities in use by my patients.
Potentially contributing to this trend, parents of my youngest patients seem most amenable to spectacle lens use; they are also easy for clinicians to prescribe. However, with these benefits also come drawbacks. Eyeglasses for myopia control are expensive; the single-vision lenses that parents may have bought before for $200 or less can reach prices of $800+ (CAD), which can be hard for parents to accept.
Moreover, while prescribing spectacles is straightforward, follow-through and management of the disease process of myopia can prove more challenging with glasses than contacts. When prescribing spectacles lenses, you want to determine the patient’s baseline axial length and will want to keep continuous measurements on a three- or six-month basis to confirm if it is changing. If axial elongation is occurring along with refractive error changes, additional questions must be brought to the forefront: Is the patient being managed properly? Does adjunctive therapy need to be added? What would adjunctive therapy be? What would follow-up look like when initiating this? In this respect, contact lenses may be the easier modality to recommend if you anticipate the patient’s prescription to change frequently.
 |
|
Fig. 3. This flowchart of possibilities for myopia management can help parents appreciate what options are available for each route. Click image to enlarge. |
The spectacle lens company policy usually has a 12-month warranty window for families who accept the spectacle lens option. For example, if the patient’s Rx changes by a half-diopter or more within 12 months, one company will remake the lenses at no extra cost. After 12 months, lens use can be continued if there is no change in prescription, but if so, parents would again have to pay for another set of lenses (with the 12-month warranty window starting over for that set).
When considering contact lens options, I am more inclined to recommend hybrid multifocal and monthly toric multifocal lenses in patients with astigmatism, but it depends on their Rx. If it lies outside a specific range, I would lean toward a daily option over ortho-K or do partial ortho-K treatment. I also do not recommend single-use lenses for patients with considerable astigmatism unless going for a daily option with single vision glasses over top—that way, astigmatism is corrected.
Atropine can be first-line therapy for young children when contacts or glasses aren’t options, say if the child is four to five years old or if parents are hesitant to try another modality. As the patient ages and their parents become more comfortable with you as their provider, adding spectacles or contact lenses may become more feasible. I will use 0.05% atropine as an adjunct to boost the efficacy of spectacle or contact lens corrective options if there has been additional progression or if there is high risk of increasing myopia. While I almost never use atropine at first, in rare cases I will administer it at three-month follow-ups with fast progressors. Most of the time, I add it in at six months if the patient’s prescription has changed beyond what I expected, or if they jump a quarter or half step in a six-month period. More importantly, I will add atropine if axial length is also increasing with no explanation for a jump in length, which can happen normally with growth spurts.
I like to follow a stepwise approach to aid in my decision of which modality to start. It is by no means a hard and fast rule, but breaking down the various factors to consider when choosing can be quite helpful. These include the age of the child, their prescription, any history of myopia progression and whether axial length has already passed a certain point. There are additional social factors that are just as important, like the child’s comfort level at putting lenses in their eyes, how confident the parents are with the child taking on this responsibility and the parent(s) ability to coax or help the child with lens insertion, removal and care, especially while taking care of other kids. If the child participates in extracurriculars, will one lens modality give them a competitive edge or help them perform better in sports? Questions such as these should also be given weight.
Step 7: Outline a follow-up schedule
I have listed this as a separate step to emphasize—to readers, and ultimately to parents—the value of the service you’re providing. Without describing specific fees, I’ll note that it is vital to remember the added chair time myopia management entails so that you are compensated accordingly. Discussing costs with parents upfront is vital, too, so they can anticipate and plan for what is coming next. I like the global fee model, which is similar to the orthodontic world that some parents may have familiarity with. Once a decision has been made to proceed with treatment, I use the consultation fee and apply it to whatever the balance would be for treatment.
I outline for patients the sequence of follow-ups over the next year once a myopia management plan has been adopted. Presenting an annual package to the patient and their parents, with a schedule of visits, helps convey the value of your services and avoids any surprises for parents. Also be sure to provide take-home and follow-up material; if parents know what’s coming next, they will be more motivated and prepared for compliant behavior and care. A comprehensive package also adds reassurance; parents leave knowing that time was taken to outline important material for them. They may even show your program to friends when talking with other parents, spreading the word about your available services.
Exact follow-up schedules will depend on the modality used. For spectacles lenses, follow-up should occur every three months. Ortho-K involves a bit more of an intense schedule, including follow-ups at one day after dispensing, one week, one month, three months, six months and 12 months. Daily disposable contact lens use will need a one-to-two-week follow-up, as well as three-month, six-month and 12-month visits. These are all designated visits included in my package with fees outlined. Still, if a patient is having trouble outside of a scheduled visit, an additional fee for chair time may be necessary.
 |
|
Fig. 4. Axial length of 26.00mm or greater in children greatly increases their risk of eye disease in adulthood. Click image to enlarge. |
Depending on the modality, I will offer contracts that provide a one-month warranty; if the patient wants to change modality within the first month, the parents will get back a percentage of the fitting fee. What the practice retains from that can be used to apply to the change. This gives parents and patients the time to decide what they do or don’t want.
How much can be saved with an annual supply of daily disposables or what is the cost of a backup pair of ortho-K lenses? If you are specific in your treatment plan, it distinguishes the specialized care you are providing from routine care. Also make sure to have a plan for what year two fees will be. If ortho-K treatment is going well and only a replacement pair is needed, a refitting fee is unnecessary.
Step 8: Exude patience with your patients
Regardless of how buttoned-up you are with knowledge of myopia management and how transparent your fee package is, some parents will not be ready to proceed. This is where I am receptive to cues in the office. I will proactively suggest we recheck their child’s prescription in three to six months or will follow-up with email content for them to review once they have gone home. No one should feel forced or guilted into pursuing myopia management, but be clear with parents that there is a finite window of viability for treatment that will eventually close.
Step 9: Keep parents in the know
Whether parents seem receptive to moving forward with treatment or not, I will send an email after the initial consultation visit to reiterate what was discussed: the child’s prescription, what might happen if their myopia is left uncorrected and the steps we discussed. It is both a financial and time investment that needs to be articulated from the beginning for parents to understand the commitment involved.
 |
|
Fig. 5. Here is a door decal that was up at my office to raise awareness about childhood myopia and its risks. Click image to enlarge. |
After they are enrolled, I will send parents periodic newsletter emails from my office about news regarding different myopia management modalities and what new research is saying. It not only shows that you are on top of your game, but differentiates your practice from others that may just give the child the treatment with no up-to-date information on current research. Also, make sure that at least one staff member is designed as a parental liaison who is available to field calls and provide educational materials. Parents appreciate having a “go-to” person’s name and emergency number and/or email address.
Step 10: Don’t try to be a hero right from the start
I find that practitioners who are newcomers to myopia management struggle most with the perceived need to become an overnight expert before even entertaining the idea of offering the service. While additional expertise is obviously beneficial to the practice’s ability to provide this type of service, it is possible to begin slowly.
If encountering a -3.00D child at age seven, it is acceptable to tell the parents that the standard of care is no longer just to prescribe a single-vision pair of glasses. Starting a patient’s myopia management journey can be as simple as starting daily disposables. Single-vision soft contact lenses are an easy first step to start in kids with no or low amounts of astigmatism. Once there’s comfort among patient and parent(s) alike, suggest switching to dual-focus contact lenses designed to mitigate myopia and see where it takes you.
Think about your patients in the last two weeks and consider: Would any benefit from being in a non–single-vision pair of spectacles or contacts? I suspect plenty would.
Dr. Ramdass is in clinical practice in Toronto and Mississauga, Ontario, Canada. She graduated from the Inter American University of Puerto Rico School of Optometry and completed a cornea and contact lens residency at the Michigan College of Optometry. She’s a member of the Ontario Association of Optometrists and fellow of the American Academy of Optometry and the Scleral Lens Society. Dr. Ramdass is a committee member and contributing author for the International Myopia Institute. Her practice, eyecademy.ca, is a Canadian pilot site for SightGlass Vision’s Diffusion Optics Technology lenses.
1. Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036-42. 2. The standard of care for myopia management by optometrists. World Council of Optometry. myopia.worldcouncilofoptometry.info/standard-of-care. Accessed August 10, 2023. 3. Mutti DO, Jordan LA, Zadnik K. Predicting the onset of myopia in children: results from the CLEERE study. BMC Ophthalmol. 2021;21:279. 4. Myopia calculator. Brien Holden Vision Institute. bhvi.org/myopia-calculator-resources. Accessed August 10, 2023. 5. Smith EL 3rd. Optical treatment strategies to slow myopia progression: effects of the visual extent of the optical treatment zone. Exp Eye Res. 2013;114:77-88. 6. SightGlass Vision spectacle lenses. CooperVision SEC. coopervisionsec.eu/sightglass-vision-spectacle-lenses. Accessed August 10, 2023. 7. Rappon J, Chung C, Young G, et al. Control of myopia using diffusion optics spectacle lenses: 12-month results of a randomized controlled, efficacy and safety study (CYPRESS). Br J Ophthalmol. September 1, 2022. [Epub ahead of print]. 8 Walline JJ. Myopia control: a review. Eye Contact Lens. 2016;42(1):3-8. 9. All about eye glasses for myopia control. My Kids Vision. mykidsvision.org/knowledge-centre/all-about-eye-glasses-for-myopia-control. Accessed August 10, 2023. |

