 |
A 40-year-old Caucasian female presented with three days of paracentral visual disturbance in both eyes (OU). She denied flashes, floaters, pain or photophobia. Her medical and ocular histories were unremarkable; she denied any prescription, over-the-counter or illicit drug use. She also denied any similar previous episodes and had no known environmental or drug allergies.
Her entrance visual acuities with pinhole were 20/25 OD and 20/20 OS. Her pupils were equally round and reactive without a relative afferent pupillary defect. Confrontation visual field and extraocular motility testing were both normal, and intraocular pressure was 14mm Hg OD and 12mm Hg OS by applanation. Anterior segment examination revealed 3+ diffuse punctate epithelial erosions (PEE) OD and 2+ PEE OS. Posterior segment findings can be seen below.
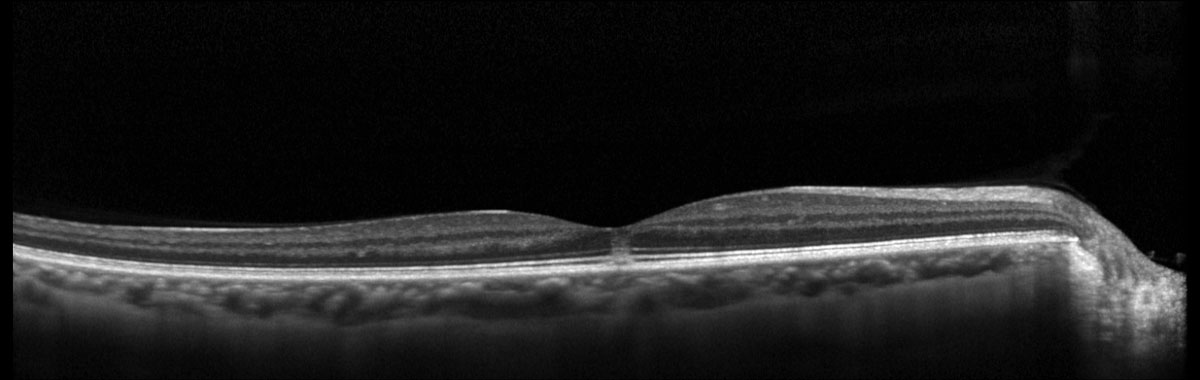 |
Fig. 1. Heidelberg Spectralis macular OCT of the right eye. Click image to enlarge. |
 |
|
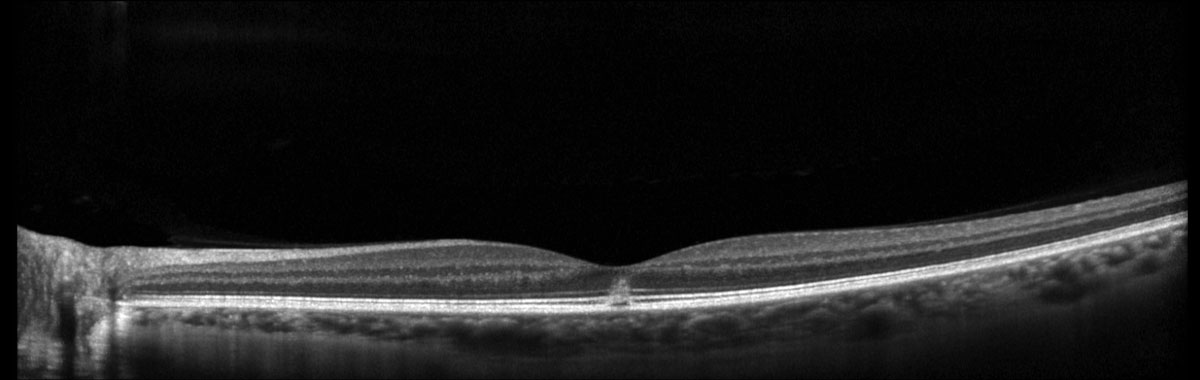
Fig. 2. Heidelberg Spectralis macular OCT of the left eye. Click image to enlarge. |
Take the Retina Quiz
1. Which of the following descriptions of the OCT images (Figures 1 and 2) is true?
a. There is a subretinal hyperreflective lesion.
b. There is hyperreflectivity of the outer retina.
c. There is intraretinal fluid.
d. There is vitreomacular traction.
2. What is the most likely diagnosis?
a. Berlin’s edema.
b. Lamellar macular hole.
c. Solar retinopathy.
d. Vitelliform macular dystrophy.
3. What is the proposed mechanism for this patient’s condition?
a. Inherited retinal dystrophy.
b. Mechanical trauma.
c. Photochemical toxicity.
d. Photothermal toxicity.
4. What is the most appropriate next step in the management of this patient?
a. Intravitreal anti-VEGF.
b. Intravitreal triamcinolone.
c. Observation and counseling.
d. Topical prednisolone acetate 1% four times daily for one week.
5. Which of the following is true?
a. The disease is inflammatory in nature and requires the use of an anti-inflammatory medication.
b. The disease is often progressive and there is no treatment; genetic testing is indicated.
c. The disease is often self-limiting but may result in permanent vision loss.
d. The disease is secondary to mechanical closed-globe blunt trauma.
Diagnosis
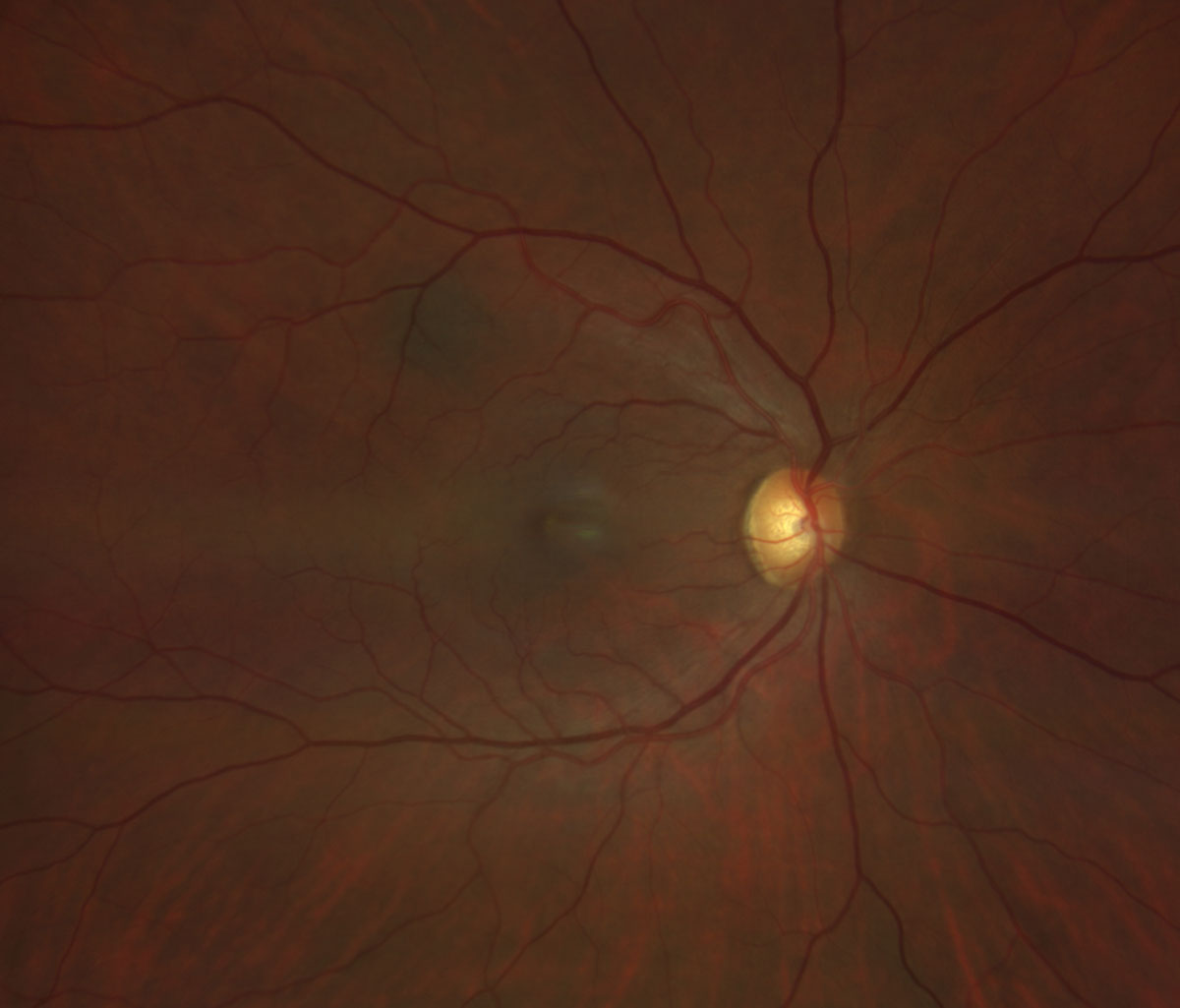
Fundus examination revealed bilateral white punctate foveal lesions in both eyes (Figures 3 and 4). Additionally, there was a small hyperpigmented flat choroidal lesion along the superotemporal vascular arcade without overlying deposits or fluid, consistent with a choroidal nevus (Figure 3). The optic nerve, retinal vasculature and retinal periphery were all otherwise normal (Figures 3 and 4).
Ancillary testing with retinal OCT revealed bilateral, hyperreflective subfoveal outer retinal disruption involving the photoreceptor inner segment and outer segment (IS-OS) layers OU (Figures 1 and 2).
Upon further questioning, the patient admitted to a recent compulsion to sungazing for minutes at a time over the last few months while photographing nature. Most recently, she endorsed a history of sungazing for three consecutive minutes the day before she noticed her symptoms starting. She adamantly denied any hallucinogenic or mind-altering drugs.
The patient was diagnosed with solar retinopathy and photokeratitis.
Discussion
Solar retinopathy describes a type of photic retinopathy resulting in retinal injury secondary to a photochemical reaction.1,2 It has also been termed solar retinitis, photoretinitis, foveomacular retinitis or eclipse burn/retinopathy.1-4 In contrast with photothermal or photocoagulative retinal injury, which occurs at a thermal threshold of greater than 10°F above the body’s temperature, photochemical toxicity occurs with less than 10°F change in body temperature.1,2,4
Solar viewing through a 3mm pupil produces a 7.2°F rise in retinal temperature (less than a threshold for photothermal damage), but sustained viewing for greater than 90 seconds exceeds the threshold for photochemical damage. Of note, solar viewing through a dilated 7mm pupil produces a 39.6°F increase in retinal temperature, far exceeding the threshold for photothermal damage.1,2,4 That being said, momentary solar observation or looking up at the sky on a bright sunny day is typically safe.2
Solar retinopathy is primarily associated with solar eclipse viewing and sungazing in the setting of religious events, rituals, psychiatric illness, consumption of hallucinogenic drugs (e.g., LSD) and hypoglycemia, but can also be caused from exposure to laser pointers.1,3,4 The severity of injury is dependent on age, duration of exposure, intensity of light source, spectral content and even refractive error.1,3,4 Higher energy, shorter wavelength light (i.e., UV radiation) carries greater potential for phototoxicity than visible light.1,2,4 Younger age or clearer crystalline lens status may allow for greater transmission of hazardous UV radiation. Furthermore, emmetropia and low hypermetropia also result in increased relative light focus onto the retina.1,4 Other predisposing factors may include chorioretinal hyperpigmentation, higher body temperature and systemic photosensitizing agents such as tetracycline antibiotics or psoralen.1,2,4
Visual symptoms typically develop within hours of solar exposure and include central or paracentral scotoma, chromatopsia, metamorphopsia, photophobia, as well as headache or periorbital ache.1,2,4
Solar retinopathy generally presents with bilateral, foveolar lesions that may be asymmetric with greater severity in the more dominantly fixating eye.3,4
Diagnosis is essentially based on clinical exam with supportive history. Visual acuity is typically reduced to 20/40 to 20/70 at presentation.4 Acute solar maculopathy will show a white, yellow, red or gray foveolar lesion OU.3-5 The exam often evolves over the first two weeks with fading of the original lesion and development of retinal pigment epithelial (RPE) mottling and/or atrophy adjacent to or in place of the original lesion.1-5
Ancillary testing may be acquired, and OCT is thought to be the most helpful imaging modality.5 Acutely, OCT will show hyperreflectivity of the IS-OS and RPE layers extending from the outer retina toward the inner retina, while focal IS-OS and RPE loss can be seen in the chronic phase (i.e., focal hypertransmission on OCT).2-6 Fluorescein angiography may be normal during the acute phase but can evolve within weeks to hyperfluorescence in the form of a window defect, corresponding with the area of hypertransmission seen on OCT.2-5 Fundus autofluorescence is a less useful diagnostic tool as it often only shows isoautofluorescence, but acute central hypoautofluorescence with a surrounding hyperautofluorescent ring at the site of the lesion has been reported.7
 |
|
Fig. 3. Zeiss Clarus fundus photo of the right eye. Click image to enlarge. |
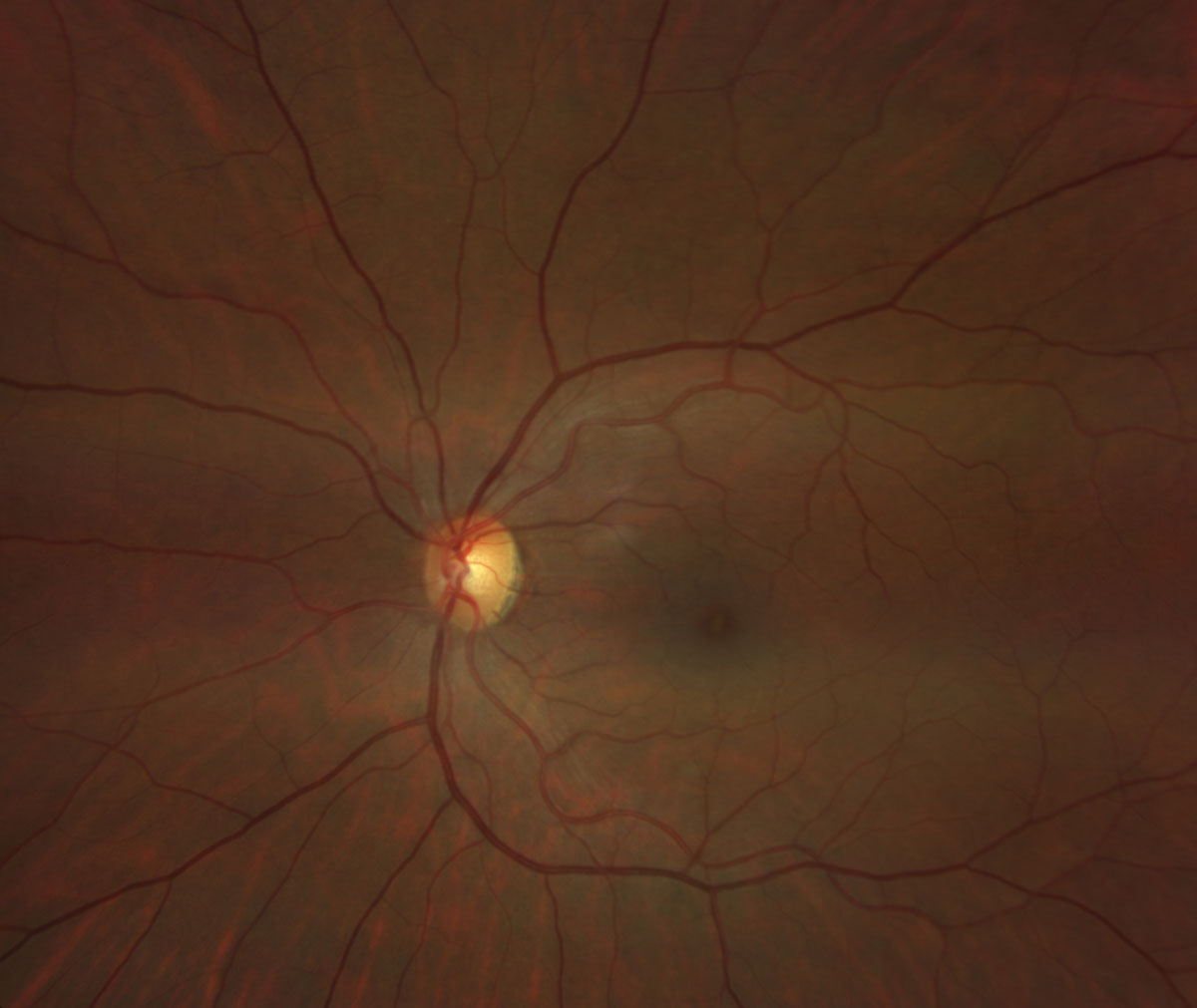 |
Fig. 4. Zeiss Clarus fundus photo of the left eye. Click image to enlarge. |
Treatment
Solar retinopathy is a self-limiting disease, and there are no proven therapeutic interventions available.1,2,4,5 Often, vision can improve to 20/20 to 20/40 or near baseline levels over a period of weeks to three to six months.1,2,4 Counseling is necessary to discourage further sungazing or eclipse viewing without proper eye protection.2,4 If psychiatric illness is suspected, a psychiatric referral may be indicated.
This patient was counseled on the potential for permanent vision loss and discouraged from continuing such behavior. She was offered a psychiatric referral but declined. Copious lubrication with preservative-free artificial tears hourly for five days was recommended to address the photokeratitis.
Retina Quiz Answers
1: b, 2: c, 3: c, 4: c, 5: c
Dr. Aboumourad currently practices at Bascom Palmer Eye Institute in Miami. He has no financial disclosures.
Dr. Dunbar is the director of optometric services and optometry residency supervisor at the Bascom Palmer Eye Institute at the University of Miami. He is a founding member of the Optometric Glaucoma Society and the Optometric Retina Society. Dr. Dunbar is a consultant for Carl Zeiss Meditec, Allergan, Regeneron and Genentech.
1. Yanoff M, Duker JS, Ausburger JJ, et al. Ophthalmology, Fifth ed. Philadelphia: Elsevier Saunders, 2019. 2. Ryan SJ, Davis JL, Flynn HW, et al. Retina, Fifth ed. London; New York. Saunders/Elsevier, 2013. 3. Freund KB, Sarraf D, Mieler WF, et al. The retinal atlas, Second ed: Elsevier, 2017. 4. Agarwal A, Gass JDM. Gass’ Atlas of macular diseases, Fifth ed. London: Elsevier, 2011. 5. Duker JS. Handbook of retinal OCT, Second ed. Philadelphia, Pennsylvania: Elsevier, 2021. 6. Bechmann M, Ehrt O, Thiel MJ, et al. Optical coherence tomography findings in early solar retinopathy. Brit J Ophthalmol 2000;84(5):547-8. 7. Bruè C, Mariotti C, De Franco E, et al. Solar retinopathy: a multimodal analysis. Case Rep Ophthalmol Med. 2013;2013:906920. |

