 |
|
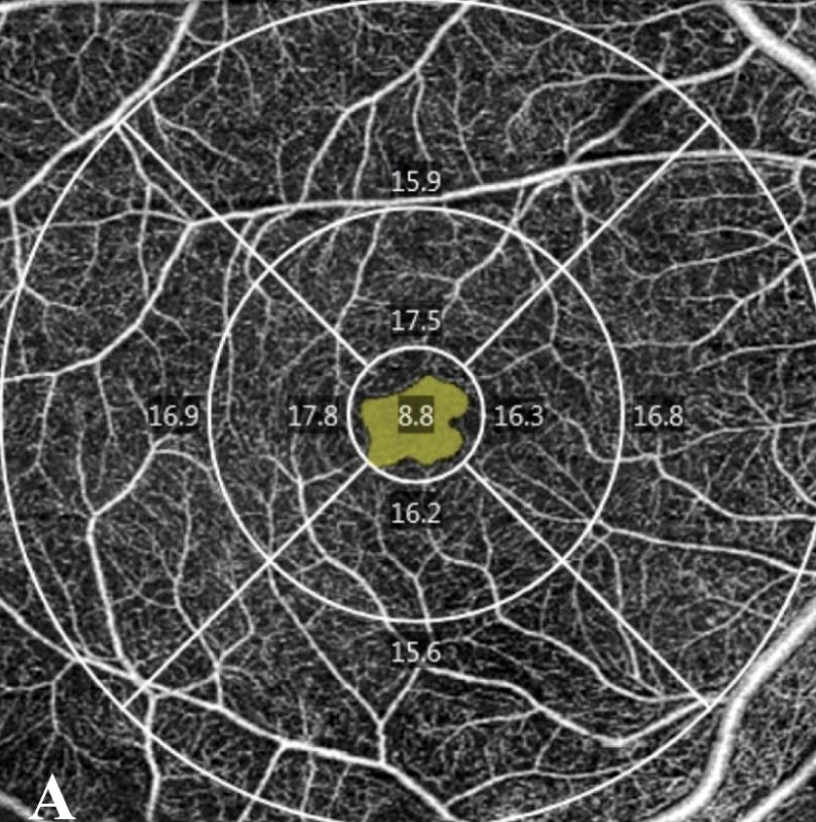
Macular perfusion density (PD), vessel density (VD), and fractal dimension (FD) on OCT-A have been found to be correlated with NP on UWF-FA, suggesting that OCT-A may be a useful tool for estimating peripheral retinal NP in patients with DR. Photo: Salongcay RP/Ophthalmic Research, https://karger.com. Click image to enlarge. |
New research has investigated a possible association between retinal and macular nonperfusion in those with different diabetic retinopathy (DR) stages. To do so, retinal nonperfusion was evaluated using ultra-widefield fluorescein angiography (UWF-FA) and macular nonperfusion with quantitative macular OCT angiography (OCT-A) to assess any correlation between peripheral nonperfusion index (NPI).
The study researchers included 48 eyes, all which had UWF color fundus photos, UWF-FA and OCT-A performed. OCT-A was used to determined foveal avascular zone (FAZ) parameters and vessel density, perfusion density and fractal dimension on superficial capillary plexus. Extent and distribution of NPI was determined on UWF-FA within the fovea-centered concentric rings corresponding to the posterior pole (<10mm), mid-periphery (10mm to 15mm) and far periphery (>15mm) and within the total retinal area, the central macular field, ETDRS fields and within each extended ETRDS field (P3-P7).
The researchers found that macular perfusion density correlated to NPI in total retinal area, posterior pole, mid-periphery, far-periphery, P3-P7, central macula and total ETDRS area. Macular vessel density and fractal dimension correlated to NPI in total retinal area, mid-periphery, far-periphery and in P3-P7. FAZ perimeter was correlated to NPI at the posterior pole, central macular area and FAZ area to NPI in central macular area.
These observations prompt the authors to suggest that OCT-A may serve as a useful and non-invasive tool to estimate peripheral retinal nonperfusion. As they explain, “the results of our study suggest that OCT-A metrics could be used as biomarkers of peripheral ischemia, particularly in patients with relative/absolute contraindications to undergoing FA.”
They add upon further discussion that the possibility OCT-A serving as an alternative biomarker of peripheral ischemia would be clinically helpful. This would greatly help manage DR patients, since use of FA to establish peripheral nonperfusion is already limited in practices for its invasive nature as well as potential life-threatening side effects. OCT-A is an ideal imaging method to quantify nonperfusion, regardless of DR severity, due to its ability to detect blood flow noninvasively with high contrast and depth resolution.
The authors elaborate on just how implementation of this approach might take place in the future: “The tedious grading process of total nonperfusion area and total area on UWF-FA, as performed in the present study, makes it unsuitable for routine clinical practice. The process could become more straightforward through software improvements and automation, allowing these measurements to be readily available for integration into the surveillance of diabetic eye disease.”
Vujosevic S, Fantaguzzi F, Silva PS, et al. Macula vs. periphery in diabetic retinopathy: OCT-angiography and ultrawide field fluorescein angiography imaging of retinal non perfusion. Eye (Lond). February 24, 2024. [Epub ahead of print]. |

