 |
A 40-year-old white male presented for a LASIK evaluation with a complaint of blurry distance vision related to myopia in both eyes. His medical and ocular histories were unremarkable and he was not taking any medication. He reported no drug allergies and his past family and social histories were unremarkable.
His best-corrected visual acuity was 20/20 in each eye. Ocular motility was full with no limitation and pupils were equal and reactive to light with no afferent defect. Ocular alignment was normal with an orthophoric position in primary and lateral gazes. Additionally, he noted 10 out of 10 color plates in each eye.
Intraocular pressure measured 13mm Hg OU. The anterior segment exam was unremarkable. Fundus exam showed healthy lenticular, vitreous, vascular and retinal structures. The optic nerves showed a cup-to-disc ratio of 0.20 with mild temporal disc pallor (OD>OS) and strong spontaneous venous pulsations.
Although he was asymptomatic, the disc pallor raised a red flag. So we ordered spectral-domain optical coherence tomography (SD-OCT) and visual field testing. But the SD-OCT showed a normal retinal nerve fiber layer and the visual field was full without defect in either eye.
That, too, raised a red flag.
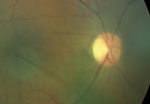 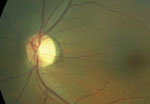 | |
| An asymptomatic patient presented with mild temporal optic disc pallor in both eyes. Normal SD-OCT and visual fields led us to order visual-evoked potential testing. |
The presence of temporal optic nerve pallor, normal retinal examination, normal SD-OCT and a full visual field prompted us to order a visual-evoked potential (VEP) test. The VEP test revealed a mild delay in amplitude and latency of both eyes, which confirmed our clinical suspicion of optic atrophy. In this case, the differential diagnosis included space-occupying lesion, demyelinating disease, nutritional optic neuropathy, autoimmune-related optic neuropathy and dominant optic atrophy. Consequently, we scheduled him for magnetic resonance imaging (MRI) of the brain and orbits with and without contrast and fat suppression.
Imaging studies revealed multiple periventricular white matter (PWM) lesions. Causes of PWM lesions are extensive but most commonly include normal senescent changes, hypertension, focal cerebrovascular accidents, demyelination, migraine, vitamin B6 (pyridoxine) deficiency and infectious or inflammatory-related vasculitis.1
Subsequently, we ordered the following serologies: complete blood count; vitamin B6, B12 and folate; erythrocyte sedimentation rate; comprehensive metabolic panel; angiotensin converting enzyme; lysozyme; Lyme titre; fluorescent treponemal antibody absorption; rapid plasma reagin; human immunodeficiency virus; antinuclear antibody and anti-neutrophil cytoplasmic antibody—all of which were normal.
Accordingly, we referred the patient to neurology for evaluation. The abnormal VEP test and PWM lesions on MRI prompted an additional MRI of the neck and spine, which was unremarkable.
Given the patient’s age, segmental pattern of pallor, abnormal VEP test and the specific location (i.e., periventricular and juxtacortical) of MRI lesions, he was diagnosed with multiple sclerosis and started on Avonex (interferon beta-1a, Biogen).
To date, the patient is doing well.
Discussion
This case illustrates two very important points: (1) pseudopallor of the disc must be differentiated from asymptomatic optic nerve atrophy, and (2) VEP should be measured in suspected cases of optic nerve pallor when SD-OCT and visual field are unremarkable.
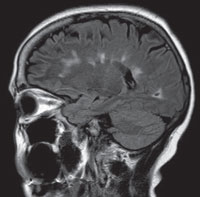 | |
| MRI revealed white matter lesions, which indicated a demyelinating condition. |
The normal color of the disc is a manifestation of the interaction between the superficial nerve fiber layer and the deeper intraretinal vascular plexus. The hue of the disc is fairly subjective, and the temporal portion is often lighter in color than the rest of the disc because there are fewer densely packed capillaries at this location. This is why crowded discs appear hyperemic and large myopic discs often appear pale temporally. However, in pathologic pallor, loss of nerve fiber layer results in light reflecting off glial cells on the surface of the disc.
Subsequently, there are certain conditions that can create the illusion of pallor. Mimickers of optic atrophy include physiologic myopic temporal pallor, aphakia, pseudophakia, tilted discs, optic nerve hypoplasia and myelinated nerve fibers.2
Optic atrophy can clinically present as diffuse or segmental, the latter of which may be altitudinal, temporal or bowtie (band) in configuration. Although diffuse optic atrophy is non-specific, segmental pallor often yields a specific disease entity based on a pattern:
• Altitudinal pallor is often observed in vascular disease such as anterior ischemic optic neuropathy.
• Temporal pallor, as seen in our patient, is typical of optic neuritis, toxic/nutritional, and hereditary optic neuropathies.3
• Band atrophy is observed in chiasmal syndromes and optic tract lesions.4
Additional clinical findings that may help support true optic nerve atrophy include identifying the presence of a segmental pattern and the presence of collateral venous vessels, macular exudates, attenuated arterioles and high water mark sign.2 Formal VF testing, OCT and electrophysiological tests (i.e., VEP) are also helpful. In our patient, the VF and SD-OCT were unremarkable, but the VEP showed a decrease in amplitude and latency, which confirmed our suspicion of mild optic nerve atrophy.
VEPs are electrical signals that are a measure of the electrophysiological activity at the visual cortex and are part of the total electrical brain activity, as measured by electroencephalogram. VEPs are a representation of the visual pathway function from the anterior segment to the visual cortex.
The VEP will elicit waveform, amplitude and latency responses based on a delivered stimulus to the visual system. Amplitude indicates how much information is reaching the visual cortex whereas latency (peak time) indicates the time the electrical signal takes to travel from the retina to the visual cortex. Latency measurements can reveal issues affecting vision if it takes more time than usual for the electrical signals to reach the visual cortex.5 A large number of clinical studies have shown that VEP tests can reveal demyelinating lesions in the optic nerve and are more sensitive in confirming both clinical and subclinical optic neuropathy when compared to optical coherence tomography.6
In this particular case, temporal pallor of the disc was the only questionable clinical finding. Since the patient’s visual acuity was normal and ancillary findings were unremarkable, we believed this was representative of a chronic intracranial process. After MRI revealed PWM lesions and serology discounted additional pathology, we were highly suspicious of a chronic demyelinating condition. Because the patient had no prior occurrence of acute or sub-acute vision loss, the most likely cause was a slow, chronic conduction deficit from demyelination of the optic nerve. This explains why the OCT and VF were unremarkable and the VEP test was abnormal. If demyelination were to continue to affect the nerve, we would expect to find papillomacular bundle field defects and associated nerve fiber layer loss.
Ultimately, we advocate for testing VEP to differentiate pseudopallor from asymptomatic optic atrophy if the visual field and SD-OCT are normal.
1. Barkhof F, Scheltens P. Imaging of white matter lesions. Cerebrovasc Dis. 2002;13 Suppl 2:21-30.2. Digre KB, Corbett JJ. Practical Viewing of the Optic Disc. Massachusetts: Butterworth-Heinemann, 2002.
3. Rath EZ, Rehany U, Linn S, Rumelt S. Correlation between optic disc atrophy and aetiology: anterior ischaemic optic neuropathy vs optic neuritis. Eye (Lond). 2003 Nov;17(9):1019-24.
4. Miller NR, Newman NJ, Biousse V, Kerrison JB. Walsh & Hoyt’s Clinical Neuro-Ophthalmology: The Essentials. 2nd ed. Philadelphia: Lippincott; 2007.
5. Odom JV, Bach M, Brigell M, et al. ISCEV standard for clinical visual evoked potentials (2009 update). Doc Ophthalmol. 2010 Feb;120(1):111-9.
6. Naismith RT, Tutlam NT, Xu J, et al. Optical coherence tomography is less sensitive than visual evoked potentials in optic neuritis. Neurology. 2009 Jul;73(1):46-52.

