A majority of optometrists are content to describe themselves as primary eyecare providers, but over one quarter feel they also possess “subspecialty skills” in one or more specific niches—and they would like such capabilities to be recognized by others, too. Doing so would bolster referrals to ODs and could allow greater integration of optometry into the wider healthcare infrastructure. Enthusiasm for subspecialization is strongest among the younger members of the profession, but even most senior ODs see it as valuable, while still expressing some wariness over an as-yet-undefined credentialing process. Still, ODs seem ready to hash out the details.
Those are some of the key findings from a new survey on optometric sentiment toward optometric subspecialization. Conducted by Jobson Optical Research in August 2023, this survey received input from 506 practicing ODs and 95 optometry students.
The research is being released during this year’s Academy of Optometry annual meeting in hopes of stimulating discussion among various stakeholders. The full report will be available for download from Jobson Optical Research. Below, we share highlights of some of the major trends and discuss how they might inform a profession-wide discussion about efforts to formally credential ODs in various subspecialties.
“It would reassure patients that they are seeing a provider who understands their individual condition thoroughly,” wrote an optometrist from Cincinnati in response to the survey. “It would also serve as a way for eyecare providers to refer patients to each other in a meaningful and more purposeful way if we knew each other’s clinical interests.”
 |
|
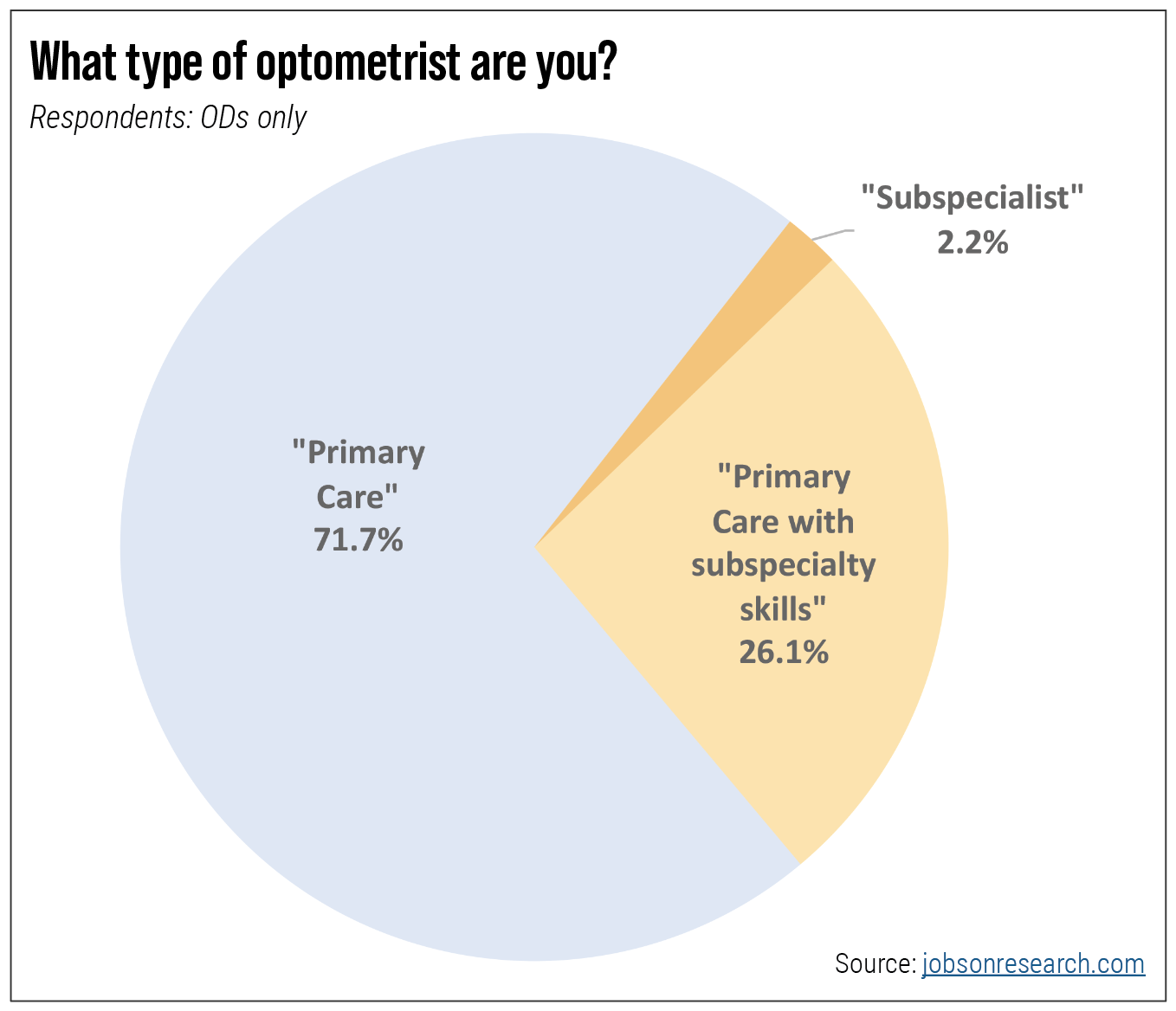
Fig. 1. Primary eyecare remains the chief responsibility of optometrists, but over one-quarter say they possess an additional layer of skills in one or more specific disciplines. Click image to enlarge. |
Subspecialties Taking Shape
Among ODs who responded to the survey (i.e., excluding students), 41.5% have been practicing for over 20 years and 62.7% are in private practice settings. As Figure 1 shows, primary eye care is the domain of virtually all respondents but, importantly, 26.1% say they also have additional expertise above and beyond that level and 2.2% call themselves subspecialists outright.
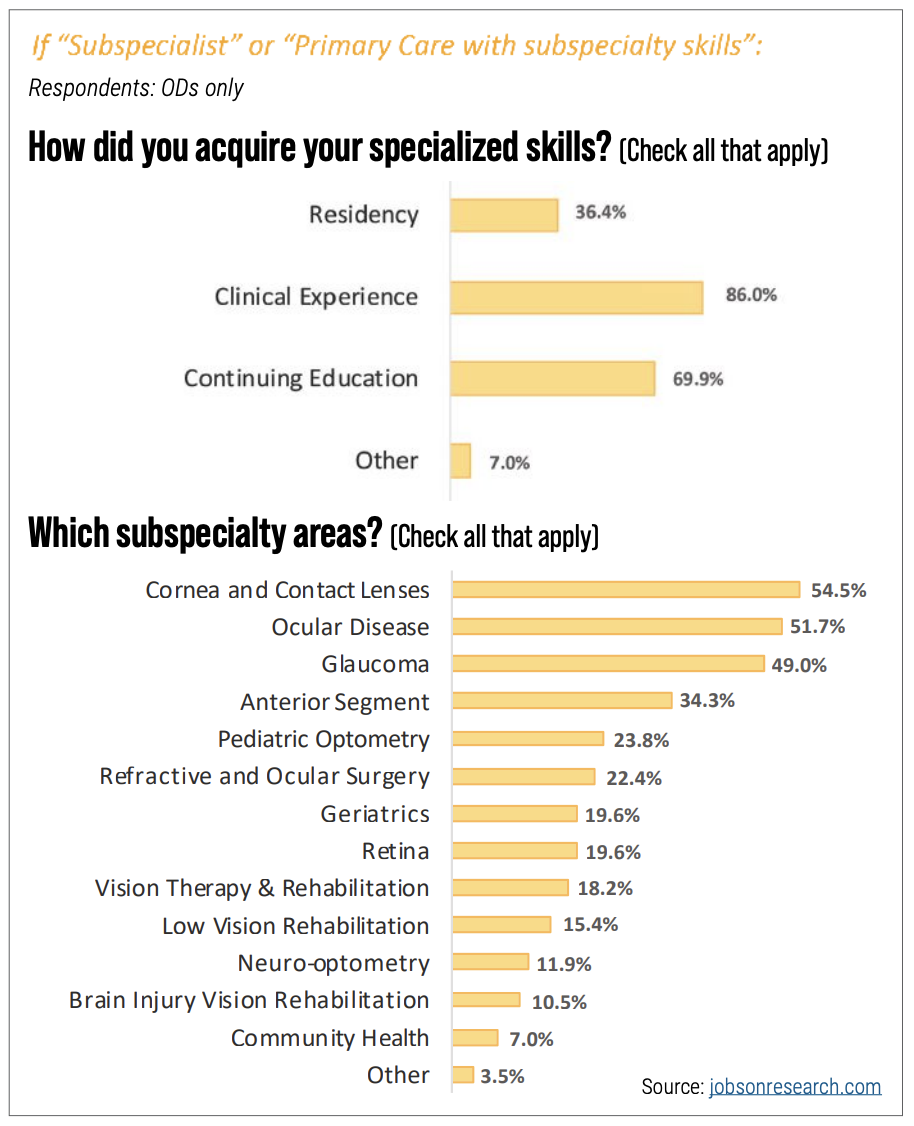
In the survey, 86% of those who lay claim to subspecialty skills point toward the clinical experience they developed over the span of their careers (Figure 2). Peer-to-peer training via continuing education was called out by 69.9% and optometric residency training came in at a healthy 36.4% of respondents.
 |
|
Fig. 2. Through a combination of residency training, CE and ample clinical experience, optometrists feel they have developed specialized skills, chiefly in optometric strongholds. Click image to enlarge. |
Still, formalized processes to define, train and credential subspecialists are needed for any such effort to take off.
“Subspecialization permeates the entire healthcare system,” says David Heath, OD, president of SUNY College of Optometry and a longtime proponent of subspecialization within optometry. “Pretty much every doctoral-level health profession has subspecialties and there are guidelines, rules and paradigms that are applied. As subspecialties emerge in the optometric profession, we should be in compliance with reasonable and standard structures within the healthcare delivery system.”
Lack of consistent nomenclature is one problem. “What defines a pediatric optometrist, for instance?” asks Dr. Heath. “Is that centered on developmental issues or more medical ones?”
| Interested in obtaining the full report? Check jobsonresearch.com for details. |
Survey respondents cited a wide range of areas they see as their strengths (Figure 2). Some map onto ophthalmology subspecialization categories like glaucoma and retina, others comprise uniquely optometric services (e.g., contact lenses, vision therapy, low vision) and at least one—“ocular disease”—seems an artifact of a previous generation’s effort to evolve optometric care. Educational curricula and advanced training or experience in a focused medical environment that emphasized ocular disease broadened optometry’s mandate beyond refraction and corrective lenses years ago. That may be a point of pride for many ODs—51.7% point to their skills in ocular disease management, second only to contact lenses—but its clinical footprint is too broad to claim as a subspecialty.
“Having a common understanding of what a subspecialty is—which we don’t currently have—can only make referrals and collaboration among optometrists all that much stronger and better,” says Dr. Heath, “and it’s something that ODs themselves are saying they would embrace.”
 |
|
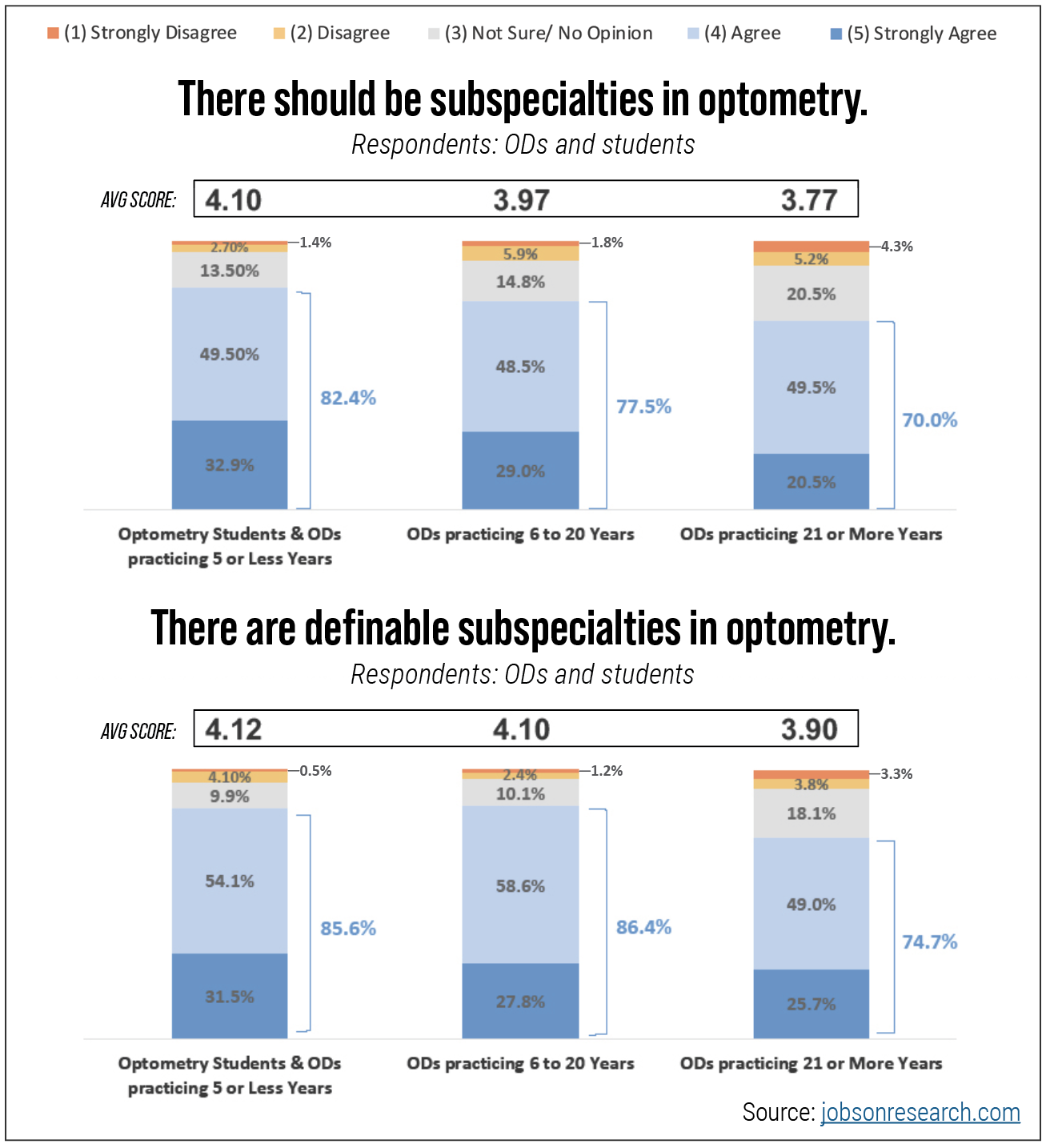
Fig. 3. Respondents endorsed the idea of optometric subspecialties with healthy majorities. Click image to enlarge. |
That’s borne out by the survey data. Even though only 28.3% of survey respondents consider their own skills to include elements of specialized care, a healthy majority do believe there should be subspecialties within optometry and that, moreover, there already are. Figure 3 shows the sentiment on these questions by age bracket. Current students and those ODs who have practiced five years or less are most bullish on both matters: 82.4% say there should be optometric subspecialties while 85.6% say these already exist.
“I believe a formal credential would allow you to state your specialty with defined support from somewhere,” wrote a student at Pacific University College of Optometry. “It’s not just saying, ‘I’m really good at this’—it proves that you have met a level of standard. It would feel better and easier to promote yourself and your specialty.”
Optometrists practicing 21 or more years were a bit more measured in their support but still endorsed both ideas, with 70.0% and 74.7% expressing agreement, respectively. “It would increase patient access for those who are having long waits for ophthalmology specialists,” an OD from Chicago suggested. “At the same time, optometrists would have closer partnerships with PCPs.”
 |
|
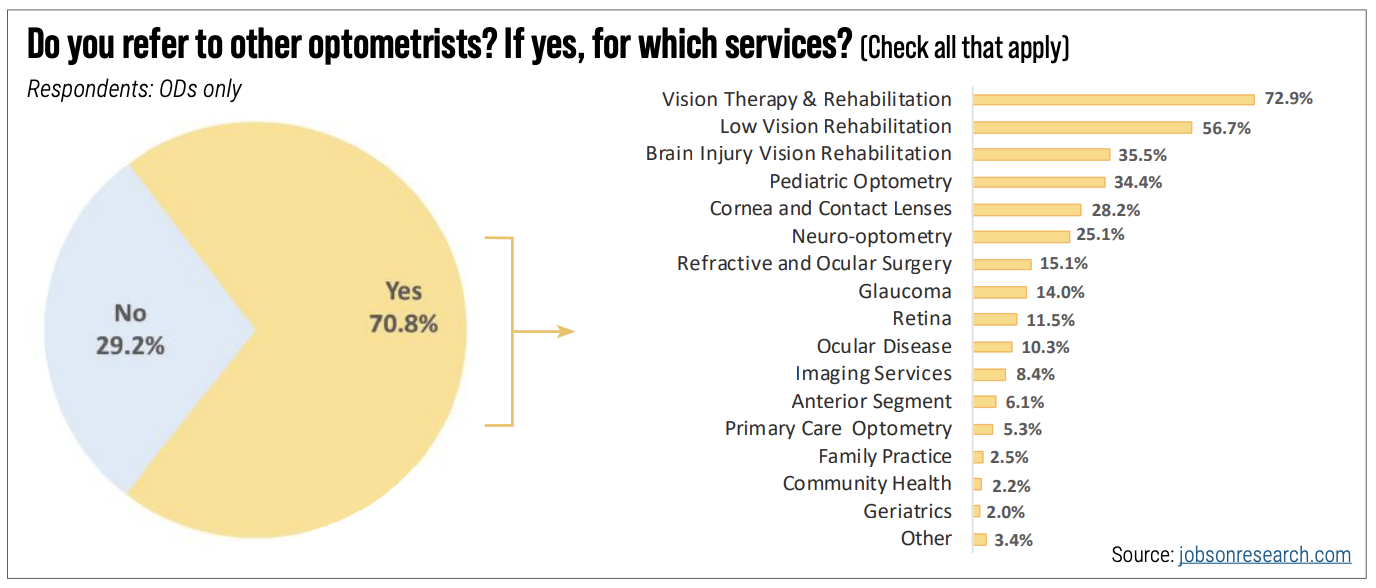
Fig. 4. OD-to-OD referral is surprisingly robust among survey respondents and heavily concentrated on traditional areas of optometric expertise. Click image to enlarge. |
OD-to-OD Networks
The topic of intraprofessional referrals is another area where formal subspecialization would be advantageous. Although the survey found that 70.8% of optometrists already refer to other ODs in some fashion (Figure 4), many cited a desire for greater clarity about who’s on the other end of that relationship.
“I think formal credentialing coupled with a directory of said specialty would make it much easier to refer to colleagues for these specialties,” another survey respondent pointed out. “As it stands, everything seems to be by word of mouth.”
Indeed, 82.4% of respondents said they would be more inclined to refer to another optometrist if that individual had formal training validated by a community of their peers (Figure 5).
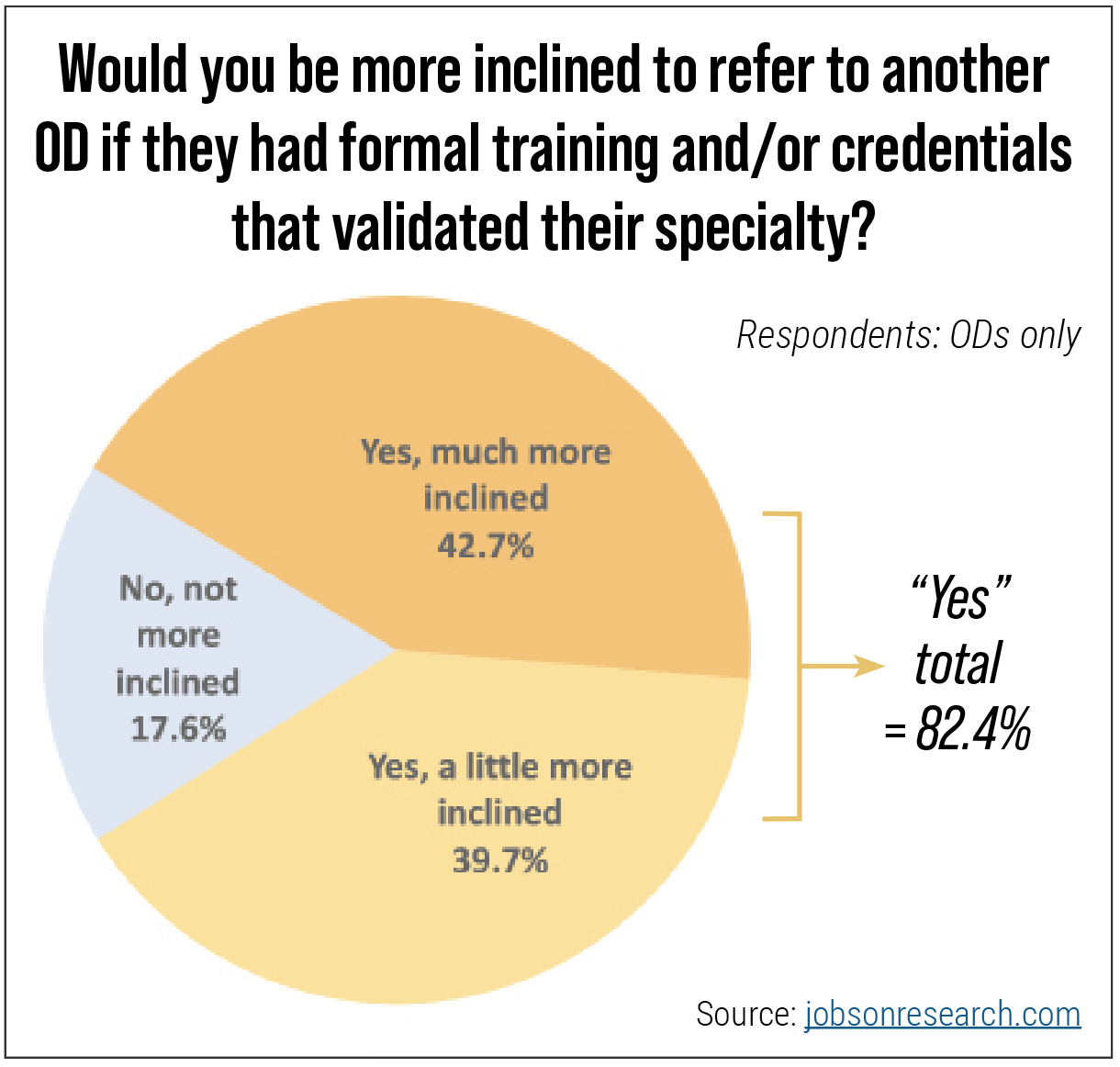 |
| Fig. 5. “There should be less stigma about OD-to-OD referrals,” wrote an OD from Minnesota. “Subspecialization would allow a practitioner to become phenomenal in one area and provide the absolute best care possible to each patient.” Click image to enlarge. |
Some areas are quite far along in the process. “Low vision has already defined itself,” explains Dr. Heath. “That community has a set of approximately 20 advanced competency statements that really identify the knowledge and skills required. Other areas we may consider discrete disciplines within optometry still need to undergo a process of establishing broad-based community agreement on what comprises their core competencies,” Dr. Heath notes.
A Group Effort
Dr. Heath believes the momentum, and most of the heavy lifting, will happen at the level of the societies. “In every health profession, the formalization of subspecialties occurred through grassroots activities,” explains Dr. Heath. “You really need the community that views themselves as either subspecialists or primary care docs with subspecialty skills to be developing the advanced competencies that define the area. They can’t be developed from above. It has to come from the bottom up.”
Professional organizations ranging from ASCO and the Academy down to the many area-specific societies that help foster subspecialty expertise can play a role in moving the conversation forward, he suggests. Some may be looking at ways to credential their members, he says, while many others may simply want to get together to talk about their shared interests and expertise. “But any credentialing process has to be built atop the cumulative knowledge of those practitioners operating at the ground level,” Dr. Heath emphasizes.
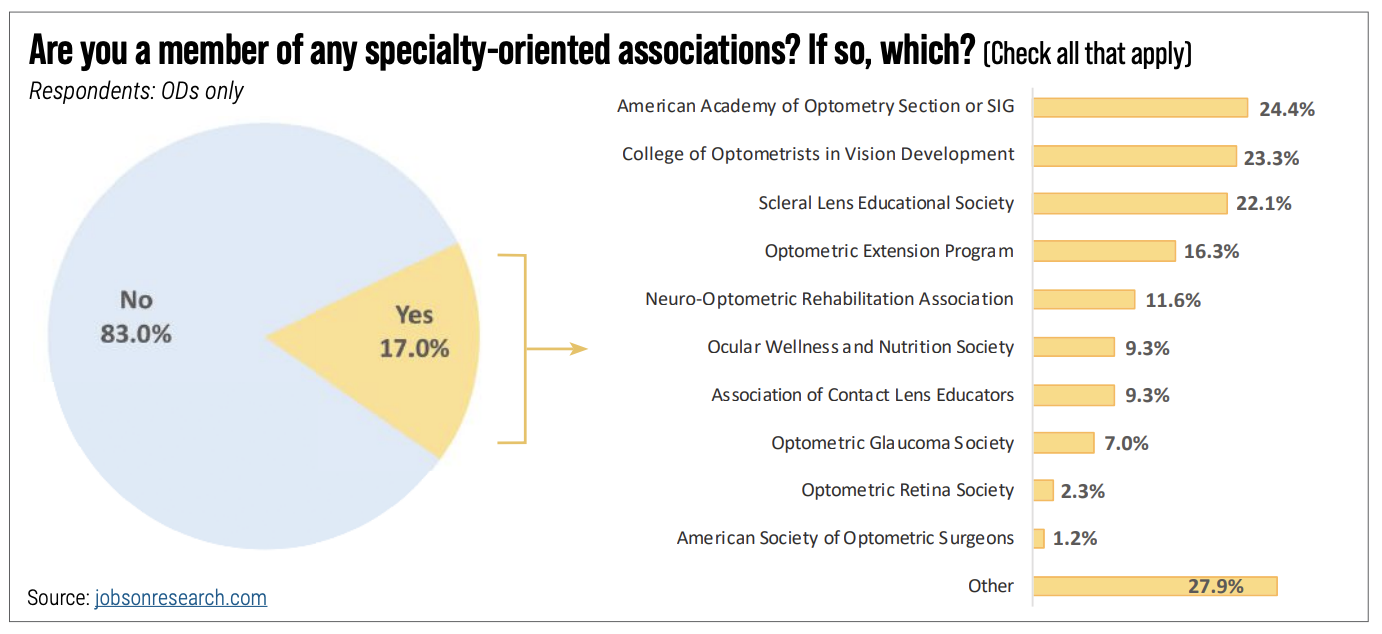 |
| Fig. 6. A relatively easy way to begin developing specialized expertise is through the mentorship to be found in professional societies. Only about one-sixth of survey respondents reported having taken such a step, however. Click image to enlarge. |
Membership in professional societies that prioritize advanced training provides a chance for mentoring and greater access to expertise. Nearly one quarter of respondents (24.4%) with such an affiliation say they belong to a Special Interest Group or Section of the Academy of Optometry (Figure 6). Among single-discipline organizations, the most populous in the survey seem to be the College of Optometrists in Vision Development (COVD) at 23.3% and the Scleral Lens Education Society, which garnered a 22.1% response. However, it’s worth noting that specialty organization membership as a whole only represented 17% of the entire sample studied.
Devil’s in the Details
If there’s one area where optometrists—established ones in particular—may express some trepidation, it’s in the prospects for credentialing.
Figure 7 shows that a slim majority of 51.9% of ODs with 21 years or more under their belts agree there should be a definable process for recognizing optometric subspecialists. Younger optometrists and students were a bit more open to the idea, however (61.7% agreed).
“When we ask whether there should there be a formal process of credentialing,” says Dr. Heath, “there’s a tendency to quickly jump to concerns about undergoing more exams and possibly more exclusionary behaviors that could ensue.” Older ODs who remember the acrimony over board certification are in no mood for a repeat performance.
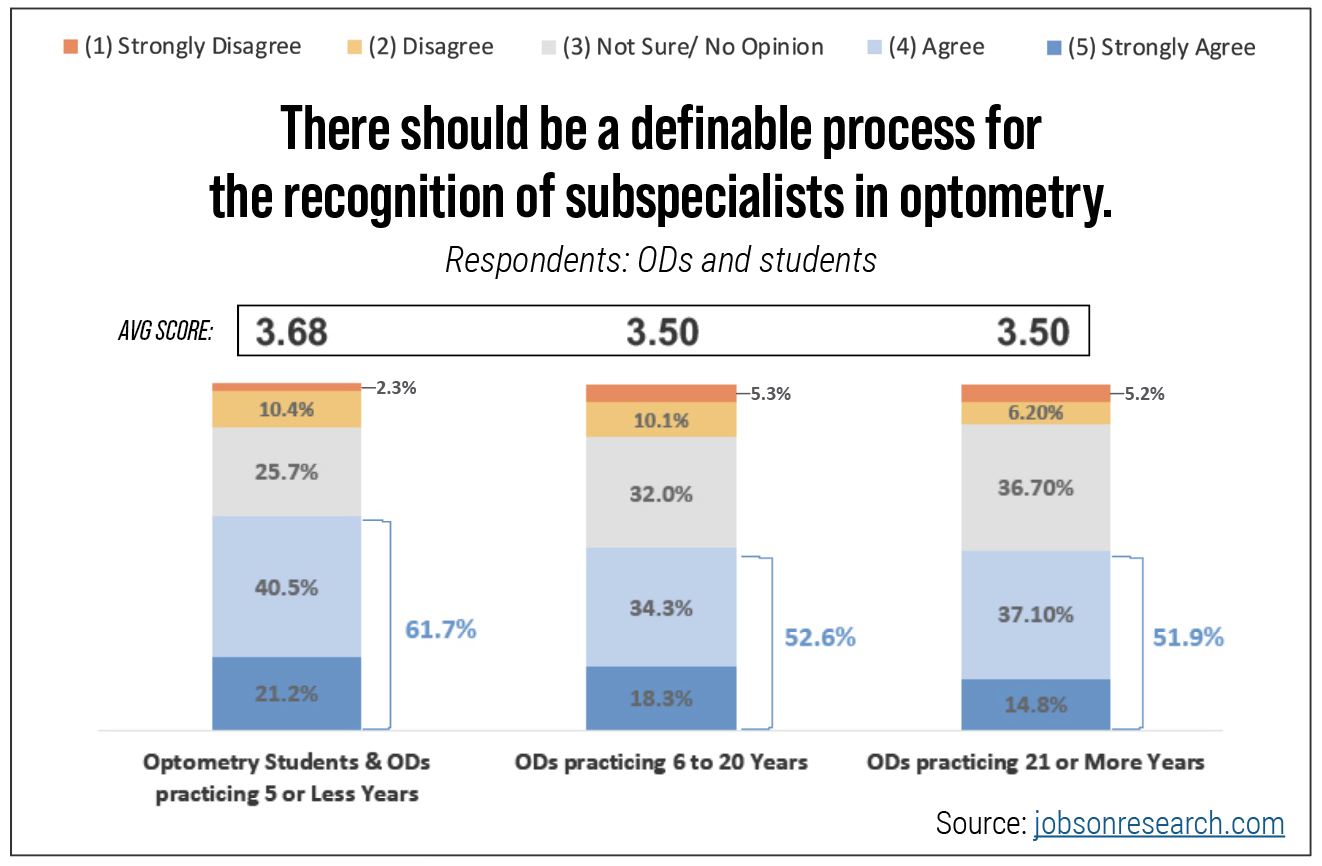 |
| Fig. 7. Optometrists with an established patient base, reputation and referral network may worry about as-yet-unknown mechanisms to codify optometric subspecialties. Click image to enlarge. |
“I’m an evolutionist—let’s take small steps,” offers Dr. Heath. “There’s no reason to jump to a model another profession may have developed over a span of decades. Allowing the organic development of subspecialties is really critical.”
Again, it’s already well underway, notes Dr. Heath. “COVD has a board certification credential for their fellows, and the diplomate processes of the Academy are relatively sophisticated and involve multiple kinds of assessment. Optometry residency education, much like in all other health professions, requires a demonstration of advanced competencies.” As well, VA optometrists use the Advanced Competence in Medical Optometry exam as a way to achieve formal recognition, and the American Board of Optometry is piloting a Certificate of Added Qualification over and above one’s status as board certified.
“What we can do as a profession is highlight the principles and guidelines that underpin subspecialties and ensure that development is in concert with health care as a whole,” says Dr. Heath.
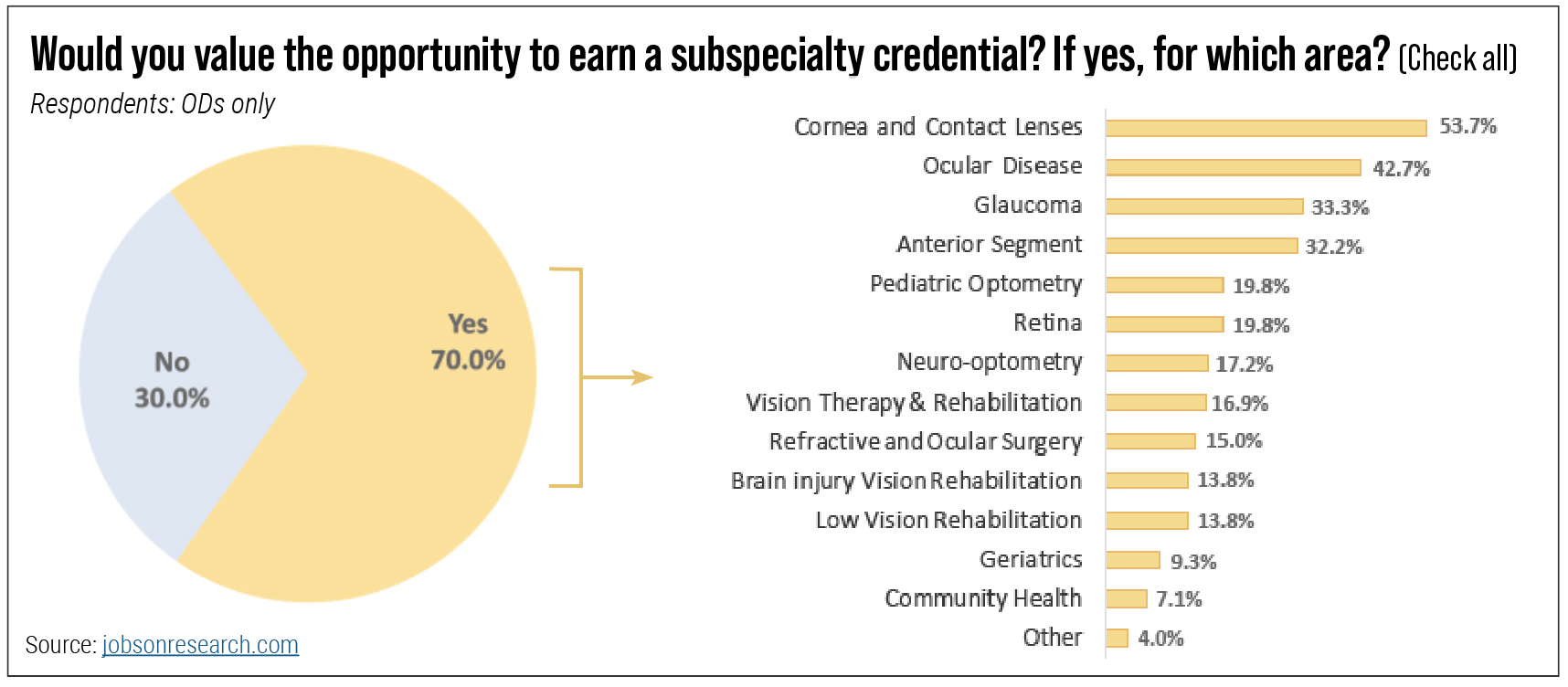 |
| Fig. 8. A robust 70% of ODs say they appreciate the opportunity to pursue a credential of some sort, especially in specialty contact lenses. Click image to enlarge. |
Value Added
Encouragingly, 70% of ODs and 92% of students said they would welcome the chance to earn a subspecialty credential (Figure 8). This is a surprisingly can-do attitude when you recall that just 28.3% said they consider themselves to be currently skilled in something that might be called a subspecialty.
As always, students will be the agents of change. “It would add value to one’s expertise on the topic as well as inspire patient confidence in your skills and education,” summed up a current Nova Southeastern student. At the same time, noted a Canadian optometrist in the survey, “optometry is a profession of generality, and that really should not be lost.

