 |
Q:
A patient complains of vision loss OS and a headache for the past month. Where do I go from here?
A:
With vision loss of potential neuro origin, it’s important to remember that it’s easy for patients to cheat on confrontation field testing if you aren’t attentive. It’s useful for screening, but dig deeper if the results don’t make sense, advises Paula Johns, OD, of Santa Fe, NM.
Dr. Johns recently treated a 71-year-old Native American female with these symptoms. Medical history was significant for kidney transplant, immunosuppression and deep vein thrombosis. Her ocular history included pseudophakia and low tension glaucoma, which was well controlled with latanoprost Qhs.
During the exam, best-corrected visual acuity was 20/20 OD and OS. Dr. Johns found no relative afferent pupillary defect, and the patient’s anterior and posterior segment findings were normal. Confrontation field testing appeared to be normal.
Based on these initial findings, Dr. Johns considered a possible diagnosis of an old branch retinal artery occlusion, presenting as a whitening of the retina in the acute phase but returning to a normal appearance, as found on dilated fundus exam here.
Dr. Johns had the patient return in two days for further testing, including automated visual fields, where she expected to find an altitudinal visual field defect. Instead, she discovered a complete homonymous hemianopsia. Based on those findings, Dr. Johns predicted a left occipital lobe abnormality and ordered a CT scan immediately.
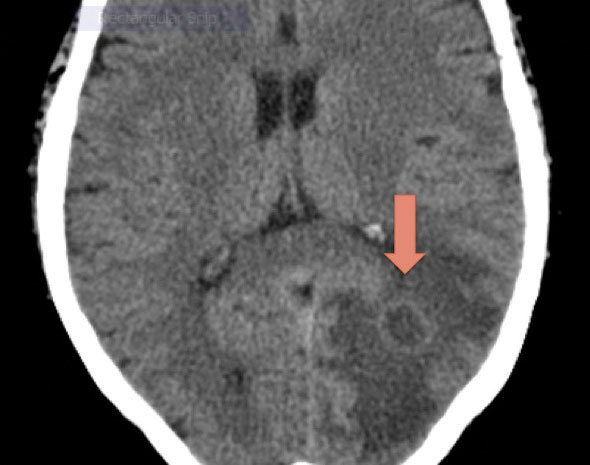 |
| Fig. 1. The patient’s CT revealed a ring-enhancing lesion and vasogenic edema. Photo: Paula Johns, OD |
Differentials
Since homonymous hemianopsia is found in myriad conditions, Dr. Johns considered several diagnoses, including stroke, its most common cause in adults.1 But a tumor cannot be ruled out initially—10% of cases are caused by one.2 If a tumor is suspected, imaging with CT or MRI should be ordered with special attention to the part of the brain expected to have the lesion, she says.
Trauma is another possible etiology, accounting for 10% to 12% of cases.2,3 Such lesions can be occipital. A majority (54%) of homonymous hemianopia patients with traumatic brain injury have multiple brain lesions.2,3
Other differentials to consider are multiple sclerosis (MS) and Alzheimer’s disease. The posterior form of Alzheimer’s can cause homonymous hemianopsia, and patients may not experience other Alzheimer’s symptoms. Brain imaging may be normal or may show cerebellar atrophy.2,4
Cases arising from MS are uncommon; when it presents, optic neuritis is the most common ocular manifestation. Visual field defects in MS usually have good prognosis and resolve over months.2,5
Infection is yet another potential cause, and a brain abscess can lead to a symptomatic mass effect. If infection is present, the CT will show an abscess. Although rare, infection can be more common in immunocompromised patients.1,6
Imaging and Next Steps
This patient’s CT showed a ring-enhancing lesion to the left occipito-parietal lobe with surrounding vasogenic edema (Figure 1). The assessment was left homonymous hemianopsia secondary to suspected brain abscess. The patient was sent to a local emergency room.
At the hospital, the initial suspicion was toxoplasmosis. However, the patient tested negative on cerebrospinal fluid analysis, so the next steps were craniotomy and abscess drainage. The culture showed Nocardia, a gram-positive bacteria found in plants and soil that can quickly spread from its primary infection site to end-organ systems such as the brain. The patient was treated long-term minocycline and imipenem. Within a year, she had full recovery of the visual fields.
In challenging cases like this, the importance of CT or MRI imaging cannot be overstated, Dr. Johns says. A stroke is the most common diagnosis, but other pathologies must be considered. “By catching the brain abscess before it became more symptomatic, this patient survived what could have been a fatal infection,” she says.
1. Goodwin D. Homonymous hemianopia: challenges and solutions. Clinical Ophthalmology. September 2014:1919-27. 2. Zhang X, Kedar S, Lynn MJ, Newman NJ, Biousse V. Homonymous hemianopias: Clinical-anatomic correlations in 904 cases. Neurology. 2006;66(6):906-10. 3. Bruce BB. Traumatic homonymous hemianopia. Journal of Neurology, Neurosurgery & Psychiatry. 2006;77(8):986-88. 4. Lee AG, Martin CO. Neuro-ophthalmic findings in the visual variant of Alzheimer's disease. Ophthalmology. 2004;111(2):376-81. 5. Law SW, Lee AW, Chen CS. Multiple sclerosis presenting with homonymous hemianopia. Australian Family Physician. 2009;38(10):795-96. 6. Lin Y-J, Yang K-Y, Ho J-T, Lee T-C, Wang H-C, Su F-W. Nocardial brain abscess. Journal of Clinical Neuroscience. 2010;17(2):250-53. |

