In Favor
Technology Improves Care, Convenience and Communication
By Ken Jeffers, OD
I use ultra-widefield imaging (UWFI) as an alternative to, and sometimes even a replacement for, dilation in many of my patients.
There, I said it. If you’re a member of an optometric social media site, you’ve probably already formed an opinion of me based on this first sentence, and it may not be a positive one. I’m not asking you to agree with me. Rather, I’m asking you to hear me out with an open mind. This article is not a scholarly treatise comparing UWFI’s clinical accuracy in a retinal exam to that of a dilated fundus exam, because there are plenty of those already written. I’m writing as a typical private practice optometrist who happens to believe in the technology because I’ve been using it nearly every day in practice for the past five years.
Before I state my case as to why I support the use of UWFI, I want to make a few things clear:
- Dilation is still the standard of care to which an optometrist will be held in a court of law.1
- No technology can replace a good case history and clinical examination.
- UWFI is an excellent tool to have at our disposal—as is a bottle of tropicamide.
- I have no financial agreements or endorsements to disclose. I own an Optos Daytona, but there are other UWFI devices to choose from.
- In all patients for whom I use UWFI, I still look at their optic nerve and macula with a fundus lens at the slit lamp for an undilated binocular view.
Now that those are off of my chest, let me tell you how I use the ultra-widefield imaging modality and how it has benefited both my patients and practice.
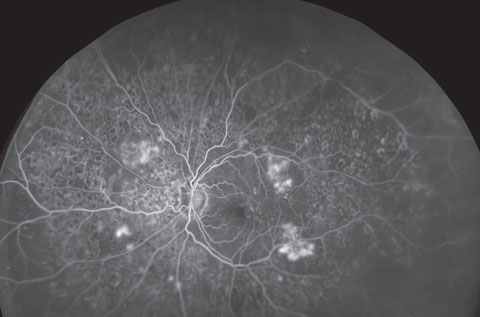 |
| UWFI can provide expansive views of the retina and help document the progression of myriad conditions, such as diabetic retinopathy, seen here in its severe form. Click image to enlarge. Photo: Optos |
Five Pros of UWFI
I have five basic reasons for you to consider UWFI in your office:
1. Patients don’t like being dilated. If you care about what your patients think and what motivates them to seek—or avoid—care, it would be unwise to ignore this fact.
Granted, we’ve all seen patients who exaggerate the side effects of dilation. I’ve heard everything from, “The last time I was dilated, I was blind for three days” to “I haven’t been able to see the same since the last eye doctor dilated me and I’ll never let anyone do that to me again.” Our patients can be, shall we say, dramatic. So, if you had an option to make their eye exams easier, wouldn’t you want to consider it? UWFI certainly has the potential to revolutionize how we practice. It’s an ingenious technology and patients love it. I have had several patients make an appointment in my office because they heard about UWFI and did an Internet search to find an office that provides this diagnostic modality. When these patients present to my office, I’m always careful to tell them that UWFI does not work for everyone, and I may still need to dilate their eyes.
2. Patients are impressed with the technology. When my technicians capture the ultra-widefield image, patients often ask what the device does. They are curious about it. When I show them the image of their own eye and compare it with images from the library of pathology, they are often blown away with what we can see. When I show them pictures of patients with choroidal melanomas, diabetic retinopathy, hypertensive retinopathy, papilledema and other pathology, they often comment, “I didn’t even know you could see those types of problems in an eye exam.” UWFI gives me an opportunity to show them first-hand what these conditions look like and educate them about the importance of regular eye examinations.
I truly believe UWFI has improved my patients’ compliance with their eye exam frequency. Although I often explain what I’m doing and what I can see during a dilated fundus examination, it doesn’t seem to have the same impact on compliance as the patient “examining” their own retina with me.
3. In certain cases, UWFI can be superior to a dilated exam using a conventional fundus lens at the slit lamp or with a binocular indirect ophthalmoscope. Before you hit “send” on the hate email you just composed, I also think a dilated fundus examination is superior to UWFI in certain cases. Ideally, doing both is best. Truthfully, certain pathologies can be better seen with UWFI, while others can be better seen through dilated pupils.
Any pathology requiring a three-dimensional view of the fundus (e.g., papilledema, macular edema or any retinal lesion with risk factors for malignancy, including elevation) requires a good dilated exam—plus UWFI.2-4 Because UWFI provides up to a 200-degree temporal and nasal imaging field and can image up to 82% of the retina, it is often better—30% better, in one study—at locating peripheral retinal lesions such as tears, holes, nevi and hemes than a dilated exam.5,6
Research also suggests UWFI can be advantageous when examining patients with diabetes. One study found UWFI, compared with standard techniques, identified retinal nonperfusion and neovascularization in an additional 10% of eyes, while other researchers found diabetic retinopathy was identified 17% more frequently in non-mydriatric UWFI compared with the ETDRS standard.7-9
Seeing the entire retina at once provides a distinct advantage within the context of diagnosing peripheral lesions.5 It’s not easy to miss retinal pathology with UWFI, as long as you obtain good quality images.
4. UWFI provides a permanent, digital image in the patient’s chart for future reference. How many times have you found something on a dilated fundus examination and wondered how long it had been there? No one enjoys that anxious moment when we think to ourselves, “Is this new or did I miss it last year?” UWFI nearly eliminates this doubt. And I don’t know about you, but my ultra-widefield images are a little better than my retinal drawings.
5. UWFI can be profitable. The device is costly to purchase, but I’ve found that it pays for itself if you believe in the technology like I do. The capture rate in my office is between 70% and 80%, and I charge a nominal fee for this service. This income is not susceptible to the chargebacks, discounts or contractual fees we have become all too accustomed to in optometry today. There is nothing wrong with making money on a service that benefits the patient and that they want.
The benefit is not just financial, either: It also saves time. We all know dilating is probably the biggest bottleneck in our office flow. I save, on average, 20 minutes on each eye exam when I use the ultra-widefield imaging modality instead of dilation.
The Power of Belief
But remember, the decision to bring any new technology into your office should never be financially motivated. Before I adopt new equipment in my office, I make sure it meets two criteria: It must benefit my patients in some way, and it must be able to pay for itself and, at some point in time, become profitable.
If you add this technology to your office, it is critical that you believe in it. Some optometrists are not on board with UWFI, and I respect that. You have to decide if it fits your practice culture and your own clinical philosophy. For UWFI to be successful in your practice, you have to make sure your staff understands it and they all have the same “script” when explaining it to patients. Do not delegate the education of UWFI to your staff entirely, though, as the recommendation ultimately needs to come from you, the doctor, to use the modality. Talk to patients about it yourself. They deserve more than a photocopied handout mixed in with the bundle of admissions papers they get in the waiting room.
As ultra-widefield imaging is optional, this is the exact script I use with my patients:
“The next portion of the exam is the internal eye health exam. This is the part of the exam where we look for eye health problems as well as general health problems that can be detected through your eye exam. The traditional way to perform this exam is with dilation (I then explain what dilation is and does), which is a service covered by your insurance but is less convenient for you. We now have an alternative to dilation called ultra-widefield imaging, which costs extra but is faster and more convenient. In most cases, UWFI is sufficient, but it depends on the quality of the images we are able to capture. If the images are not usable in my opinion, I will have to dilate you and you will not be charged for UWFI in this case. Which do you prefer today?”
Misleading a patient to think that UWFI is a replacement for dilation is unethical and ultimately reflects poorly on our profession. I only use UWFI for routine care or for capturing pathology. I never use UWFI alone when a patient presents with symptomatology clearly requiring a dilated exam to properly evaluate.
I am not oblivious to the critics’ claims about UWFI, and I agree with many of them. While I support the use of UWFI, it still comes with limitations and disadvantages.5,10 For example, good quality images rely on patient cooperation; some training is needed to capture good quality images; eyelid and eyelash artifacts can obstruct the view, especially of the superior and inferior retina; images can be blurry due to media opacities; the camera can create artifacts; and so on. Other than the last reason, these limitations could arguably present during a dilated fundus examination as well.
Never has a medical device in optometry inspired such riveting debate! I personally believe this topic is so emotional to many of us because some of our colleagues are misleading our patients into thinking that it is a replacement for dilation.
Few would argue that UWFI is not a useful technology, and when presented to our patients properly and ethically, it can be used as an alternative to dilation in many of our patients.
Dr. Jeffers is an attending optometrist at Professional Eyecare Associates in Casa Grande, Ariz.
In Opposition
All That Glitters is Not GoldBy Paul C. Ajamian, OD
Would you allow a surgeon to operate on you with one eye occluded? I wouldn’t. Stereopsis gives a medical specialist a better appreciation of the depth and contour of clinical entities. It’s simply too valuable to the outcome to be cast aside under the guise of convenience—or worse, profit.
None of our 35-year-old Omni Atlanta comanagement centers own a UWFI device, because the model doesn’t really work for a practice like ours and I am not happy about what it teaches our patients. We dilate every patient who needs it, and they expect it, so there is usually no argument between patient and clinician.
Understandably, there are increasing numbers of patients who will chose a primary care practice that does have UWFI and does not dilate. This puts the practice that does not have the instrument at a disadvantage, so some practices have relented and brought the instrument in as a screening device to attract patients.11 This gives the doctor the chance to at least explain to the patient face-to-face the necessity of dilation in their particular case.
It’s safe to say there’s nothing wrong with a device to screen the fundus. However, when the screener picks up something suspicious or questionable in appearance, dilation is well still the standard of care to further delineate the problem.11
The care model I take exception to can be exemplified by the following scenario: The patient presents to the front desk to sign in for their annual exam and the receptionist says: “Would you like to be mapped today? The test costs $45 and will allow us to forego dilation, a procedure that causes pain and light sensitivity and blurred vision for a number of hours after the exam.” What would you say if it were presented that way? Not only does it put the patient in a position to choose their own medical testing protocols, it also implicitly puts forth the notion that dilation is bad. If they choose UWFI and later you determine that they still need to be dilated, you’re now in the awkward position of having to convince them to do something that you told them their $45 would prevent. I know this may seem like an exaggeration, but patients hear what they want to hear, and this approach of offering a “dilation-free” exam may cause you to have to swim upstream at some point in the future.
In our comanagement practice, patients sometimes will present from other optometrists and will request UWFI. For instance, one who recently presented for a cataract evaluation physically blocked me as I was about to dilate her and said, “Dr. X never dilates me! Aren’t you going to map me like he does?” She truly believed that our exam was inferior to his because we were doing a dilated exam instead of UWFI, and nothing could be said that would change her mind.12
It’s critical to advise patients that UWFI is not a substitute for a dilated exam. Unless we sufficiently drive this point home, we are going to teach an entire generation of patients they don’t need to be dilated and, worse, that dilation has terrible side effects and is no longer the standard of care. If we take care to treat UWFI as a screening modality, no problem. But when we put too much stock in it, problems are going to arise.
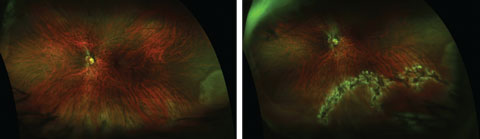 |
| This retinal break with retinal detachment, seen post-treatment (right), was diagnosed using dilated funduscopy, but was not apparent pre-treatment (left) using UWFI. Click image to enlarge. Photos: Jessica Steen, OD |
As a clinician, one qualm I have is that using UWFI can cause false positives—something we have seen in our referral setting more than once. I have had a number of patients sent to us for retinal detachment (RD), macular holes, schisis and branch artery occlusions who, in fact, had artifacts on UWFI—clinically speaking, nothing—but were told they had a potential major eye condition requiring surgery. And it’s not just false positives that pose risks for our patients and practices; clearly, false negatives would be even worse.
The missed glaucoma patient. Failure to dilate puts patient and clinician at significant risk for missing glaucoma.2 Recently, a 72-year-old patient was referred for a cataract evaluation, with no mention of any other problems. She had been seen yearly with examinations conducted using an Optomap (Optos), but no dilated funduscopy. Our evaluation revealed that the patient had 0.9 cups and 15-degree field remaining due to end-stage chronic open-angle glaucoma. In the context of my clinical practice, the biggest reasons to dilate are to look at the optic nerve and rule out glaucoma, regardless of the IOP or family history. The only way to evaluate the nerve is through a dilated pupil with a handheld lens. Mapping with UWFI falls far short if you are relying on it to rule out this potentially devastating disease.
RD false positives. At least two patients have presented recently to our clinic with a diagnosis of retinal detachment subsequent to imaging with UWFI. These patients were, to be quite honest, scared to death—and rightly so, as they were sent to us for surgery. When we dilated them, their retinas were flat and showed no signs of RD.
So, what gives? The most obvious outstanding issue that these cases illustrate is that UWFI was not used as an adjunctive modality or a screening tool that can garner initial red flags, which would then be investigated further using the standard of care, dilation. As with all technology, incorrect findings are possible, and to send patients to another professional without dilating should be avoided at all costs.
Research shows UWFI has poor imaging for the detection of retinal holes, tears and postoperative scarring, especially in the inferior and superior periphery.10 The cost of failing to dilate with suspicious findings, particularly if you suspect pathologies such as these, can be measured in terms of harm to the patient. We have the responsibility to practice in a manner that yields the best possible ocular and systemic outcomes for our patients. Practitioners are expected to allay patient’s fears—not create them. When we do, without any defensible reason, it is simply bad practice.
The profession needs to emphasize that dilation is not bad and something to be avoided. There is nothing wrong with using “convenient” modalities to bring patients into the office for a dilated exam. But, practitioners need to realize that UWFI, when it serves that purpose, is simply not a replacement to dilated funduscopy.
Professional Backsliding
After many years of working tirelessly to expand our scope of practice to include dilating drops, our profession in some ways seems to be going backwards by teaching patients, one-by-one, that this procedure is unnecessary and avoidable. We are undermining years of work in the legislature and classroom by doing what we think is more convenient and expedient for our patients.
In some cases, it is. Would I dilate a 1D myope contact lens wearer every single year? No, probably not, and UWFI might be good to do in those alternating non-dilation years. But, to sell it as a substitute is harmful and irresponsible.13 The big question that exists is whether you, a specialist in the discipline of eye care, believe dilation is perceived by the patient as negative—in essence, a problem UWFI solves. If you do, patients will pick up on it and adopt those same beliefs.
While wider images have their value, they also mean less magnification, and many doctors can’t make heads or tails of what they are seeing due to minimization. But, ODs will tell me that they find things on UWFI that they wouldn’t have seen otherwise. Yes, of course this is the case. But, I would say they may not have looked carefully enough, because they knew that UWFI would catch their misses. This I find analogous to the trend among young ODs and MDs in how they approach the macula: take a five-second look at the anatomy and say, “Let’s order an OCT.” We need to look carefully with our eyes, and if an epiretinal membrane is detected, then the OCT is appropriate to document and measure the finding. Otherwise, we are headed down a path of “automated” exams where the instruments have taken over the process.
With online sites such as Opternative promoting “eye exams” without going to the doctor, UWFI could become yet another form of ancillary testing spun as a telemedicine tool that teaches patients that a face-to-face exam is not necessary.13 Our vital, irreplaceable role is to absorb all the diagnostic data we can and offer an assessment—that’s the “art” of medicine, and no machine can replace it. Then, we may order tests to document, measure and establish baselines for those conditions first observed with the clinician’s eye.14,15
Stay True to Your Principles
For sure, UWFI is a great modality for documentation and can be a useful adjunct to established protocols of care. But too often the clinical case for it gets conflated with financial rationalizations. We sometimes see the gee-whiz appeal of a shiny new piece of technology—patients will love it, we’ll look so high tech—and get led astray contemplating the revenue stream it might bring in. But it’s wise to remember your Shakespeare: all that glitters is not gold.
The purpose of adjunctive modalities is not to steer patients to a test with the primary purpose of making money. A screening test is fine as long as it leads to a detailed fundus exam, instead of acting as a replacement for one. Make sure you are thinking solely about the clinical value that any device brings to your practice and your patients.13,14
My practice has been dilating patients for 38 years. When patients are educated on the necessity of a procedure, it is not perceived as inconvenient. If we teach our patients that dilation is a bad thing so that we can upsell them an a la carte test, it’s a disservice to our patients and our profession—and, in my opinion, unethical.13
If the test ultimately increases compliance with regular dilated eye exams, so be it. But don’t lose sight of the main objective: compliance with the standard of care.
Dr. Ajamian is the center director of Omni Eye Services of Atlanta.
| 1. AOA Evidence-based optometry guideline development group. Evidence-Based Clinical Practice Guideline. Comprehensive Adult Eye and Vision Examination. American Optometric Association. St. Louis, MO; 2015. Available at www.aoa.org. 2. American Academy of Ophthalmology preferred practice patterns committee. Preferred Practice Pattern Guidelines. Primary Open Angle Glaucoma. San Francisco, CA; American Academy of Ophthalmology; 2015. Available at www.aao.org/ppp. 3. Taylor HR, Vu HT, McCarty CA, Keeffe JE. The need for routine eye examinations. Invest Ophthalmol Vis Sci. 2004;45(8):2539-42. 4. Siegel BS, Thompson AK, Yolton DP, et al. A comparison of diagnostic outcomes with and without pupillary dilation. J Am Optom Assoc. 1990;61(1):25-34. 5. Shoughy S, Arevalo JF, Kozak I. Update on wide- and ultra-widefield retinal imaging. Indian J Ophthalmol. 2015;63(7):575-81. 6. Brown K, Sewell JM, Trempe C, et al. Comparison of image-assisted versus traditional fundus examination. Eye and Brain. 2013; 2013(5):1–8. 7. Wessel MM, Assker GD, Parlitsis G, et al. Ultra-wide-field angiography improves the detection and classification of diabetic retinopathy. Retina. 2012;32:785-91. 8. Silva PS, Cavallerano JD, Sun JK, et al. Nonmydriatic ultrawide field imaging compared with dilated standard 7-field 35mm photography and retinal specialist examination of diabetic retinopathy. Am J Ophthalmol. 2012;154:549-559. 9. Silva PS, Cavallerano JD, Tolls S, et al. Potential efficiency benefits of nonmydriatic ultrawide field retinal imaging in an ocular telehealth diabetic retinopathy program. Diabetes Care. 2014;37:50-5. 10. Kornberg DL, Klufas MA, Yannuzzi NA, et al. Clinical utility of ultra-widefield imaging with the Optos Optomap compared with indirect ophthalmoscopy in the setting of non-traumatic rhegmatogenous retinal detachment. Semin Opthalmol. 2015; 21:1-8. 11. An Optometrist’s Guide to Clinical Ethics. Bailey RN, Heitman E, eds. St. Louis, MO: American Optometric Association, 2000. 12. Deyo RA. Cascade effects of medical technology. Annu Rev Public Health. 2002;23:23-44. 13. Advisory Opinion of the Code of Ethics. Appropriate examination and treatment procedures. San Francisco, CA: Am Acad Ophthal; 2007. Available at www.aao.org/ethics-detail/advisory-opinion--appropriate-examination-treatment. 14. Augsburger JJ. Unnecessary clinical tests in ophthalmology. Trans Am Ophthalmol Soc. 2005;103:143-7. 15. Mold JW, Stein HF. The cascade effect in the clinical care of patients. N Engl J Med. 1986;314(8):512-4. |

