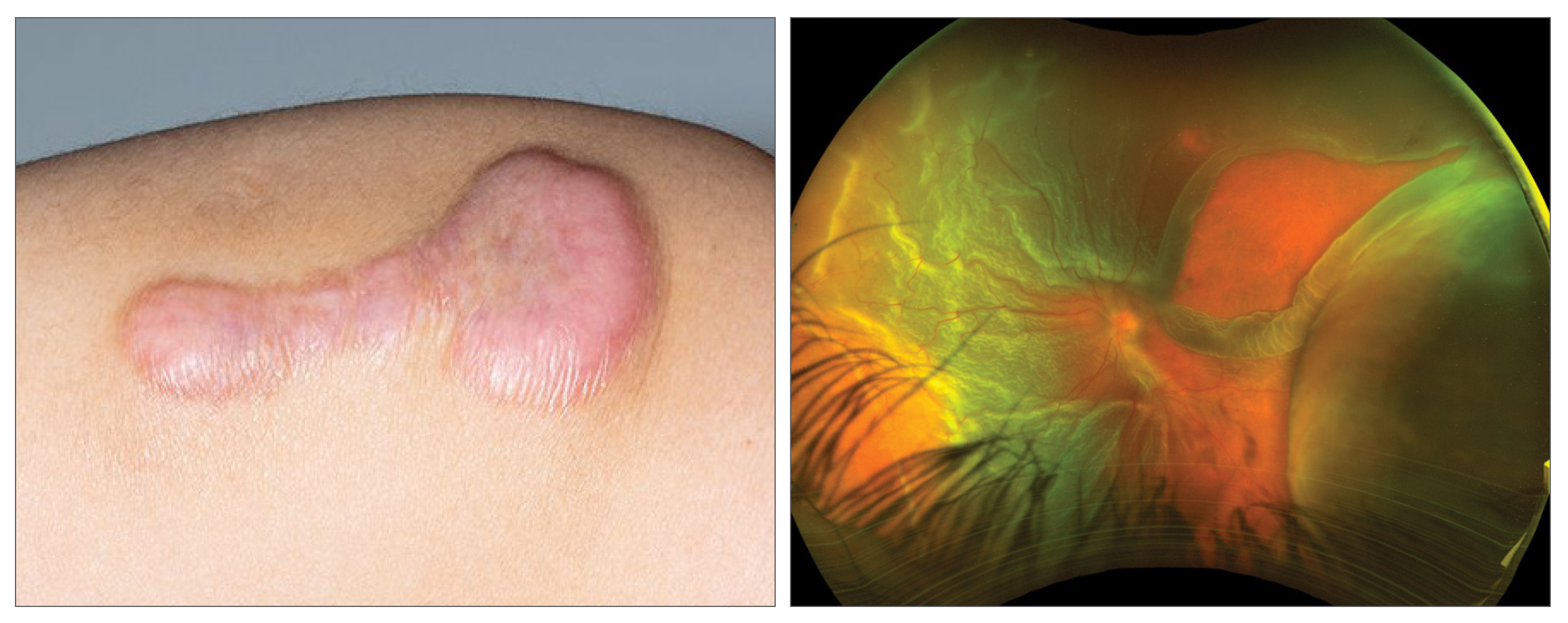
Aggressive cutaneous wound healing can produce keloids and hypertrophic scars of the skin, both resulting in thickened, raised lesions. In particular, keloids uniquely expand horizontally (whereas hypertrophy remains confined to the borders of the injury), do not regress and may present years after initial injury. Keloids and hypertrophic scars have recently been associated with a variety of health conditions and more interestingly surgical complications, and researchers explored whether there was an association between cutaneous keloids, hypertrophic scarring and fibrosis with risk of postoperative proliferative vitreoretinopathy (PVR) after rhegmatogenous retinal detachment (RRD) repair. They found that such a dermatologic history may be a risk factor.
 |
|
When including all retinal detachment repair types, the rate of PVR diagnosis was still significantly greater in the cohort with keloids, hypertrophic scars and fibrosis within 180 days from surgery. Photo: UK National Health Service; Mark Dunbar, OD. Click image to enlarge. |
The retrospective cohort study, which was published in Ophthalmology, assessed patients ≥ 18 years over a 20-year period who underwent initial retinal detachment repair with pars plana vitrectomy with or without scleral buckle, pneumatic retinopexy and primary scleral buckle for prevalence of proliferative vitreoretinopathy and complex retinal detachment repair within 180 days after RRD repair. The researchers organized the cohort into two groups of 1,061 patients, one with history of cutaneous keloids, hypertrophic scarring and fibrosis and one without. The mean age was 60.7 years.
Within 180 days, 10.1% of patients in the keloid, hypertrophic scar and fibrosis cohort and 3.4% in the other cohort had a diagnosis of PVR. (odds ratio; OR= 3.2). The study also found that 8.3% of patients in the keloid cohort and 5.4% of patients in the other cohort underwent complex retinal detachment repair (OR= 3.2). When including all retinal detachment repair types, the rate of PVR diagnosis was still significantly greater in the keloid, scar and fibrosis cohort (9.0% vs 4.2%; OR= 2.28).
“The growth factors and cytokines associated with keloids and hypertrophic scarring draw parallels with those implicated in PVR,” the study authors suggested in their paper. “Given the results of our study and the similarities in underlying pathophysiology, there may be a compelling association between these seemingly distinct conditions although a link is still speculative at this point.”
The dermatologic findings may be a noteworthy risk factor to be alert for in preoperative settings. “This carries potential prognostic implications for our RRD patients with preexisting keloids, hypertrophic scars and fibrosis; it also adds to the list of risk factors for PVR which can help guide vitreoretinal surgeons using pharmacologic treatments to either prevent or regress PVR,” they added.
The researchers noted that further research is necessary to explore whether or not these patients may benefit from current and future therapies aimed at preventing or treating PVR.
Mammo DA, Wai K, Rahimy E, et al. Association of cutaneous keloids, hypertrophic scarring and fibrosis with risk of post-operative proliferative vitreoretinopathy. Ophthalmology. January 29, 2024. [Epub ahead of print]. |

