 |
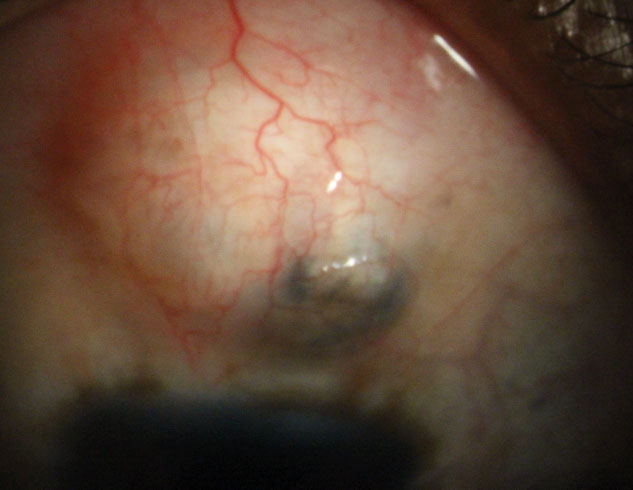
| In this study, the frequency of postoperative trabeculectomy complications did not differ between the groups with and without BCVA decline. Photo: Justin Schweitzer, OD. Click image to enlarge. |
The goal of trabeculectomy is to decrease IOP and maintain the quality of life of glaucoma patients. While the procedure is the most effective surgical intervention for lowering IOP and preventing progression, if IOP is lowered after trabeculectomy the surgery cannot be said to have a good outcome if best-corrected visual acuity (BCVA) decline occurs. Researchers in Japan investigated methods to predict decreased BCVA after trabeculectomy in glaucoma patients with good preoperative BCVA. They found that the assessment of preoperative swept-source OCT parameters in areas corresponding to the location of the papillomacular bundle could effectively predict VA decline 12 months after trabeculectomy.
This retrospective case-control study study included 35 eyes of 35 open-angle glaucoma (OAG) patients (21 male / 14 female, age: 64.0 years old, preoperative IOP: 15.9mm Hg, mean deviation: -18.1dB) with preoperative BCVA of 0.7 logMAR or better who underwent trabeculectomy and were observed for more than 12 months. The researchers defined BCVA decline as a loss of more than three lines of BCVA after 12 months.
The authors found that 11 cases (31.4%) experienced BCVA decline and that longer axial length was a significant associated factor, but that percentage reduction in IOP, severity of visual field defects, and the frequency of complications, including hypotony, choroidal detachment, the condition of the intraocular lens and hypotony maculopathy were not.
A single logistic analysis showed that the BCVA-decline group had significantly lower circumpapillary RNFL thickness than the non-BCVA-decline group (27.7μm vs. 45.1μm, cut-off value: 33.4μm), as well as lower ganglion cell complex thickness in a central strip between the disc and fovea (72.4μm vs. 87.5μm, cut-off value: 82.3μm). Multivariable logistic analysis showed that the BCVA-decline group had significantly lower temporal quadrant circumpapillary RNFL thickness and lower ganglion cell complex thickness in a central strip between the disc and fovea compared with the non-BCVA-decline group.
“These OCT scan areas that correspond to the location of the papillomacular bundle might be biomarkers that predict BCVA decline after trabeculectomy in OAG patients with good vision,” the researchers wrote in their paper.
More accurate algorithms and multimodal measurement techniques to predict BCVA decline after trabeculectomy would be valuable additions to future longitudinal glaucoma care.
“These findings suggest that objective, quantitative preoperative OCT evaluations are a useful part of glaucoma care,” the team concluded. “Clinicians should pay close attention to patients with severe damage in the papillomacular bundle when making decisions on whether to perform trabeculectomy in OAG patients with good vision.”
Takeda Y, Takahashi N, Kiyota N, et al. Predictive potential of optical coherence tomography parameters for the prognosis of decreased visual acuity after trabeculectomy in open-angle glaucoma patients with good vision. BMC Ophthalmol. 2023;23(1):399. |

