 |
|
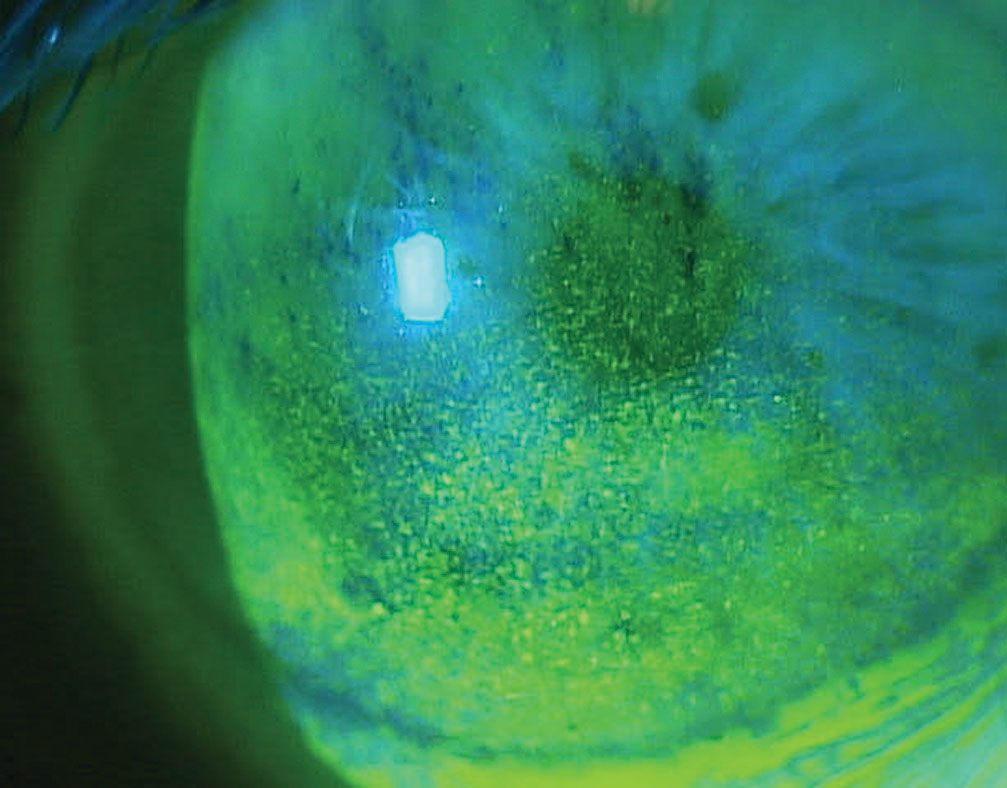
Switching to a preservative-free drop seems to cause less damage to the ocular surface in many glaucoma patients and helps prevent adverse events such as BAK toxicity, as shown here. Photo: Paul Karpecki, OD. Click image to enlarge. |
Despite many ongoing surgical advancements in the treatment of glaucoma, drop therapy remains the most common noninvasive intervention for lowering intraocular pressure (IOP) in affected patients. However, it’s known that frequent daily exposure of the tear film to these pharmaceutical agents can have negative implications for the health and stability of the ocular surface and may even increase a patient’s risk of developing dry eye disease. A team of researchers recently completed a review of current literature on the topic to help paint a clearer picture of how these drops can affect the ocular surface.
A total of 253 research articles from PubMed and Embase were included in the review. Each article contained any combination of these three key phrases: dry eye disease, meibomian gland dysfunction or meibography, topical medications or eye drops and glaucoma.
Several of the studies observed significant alterations in many ocular surface parameters in glaucoma patients on drop therapy compared with controls, including differences in Schirmer test score, tear film breakup time, conjunctival staining, corneal and conjunctival sensitivity, corneal clarity, ocular redness, lipid layer thickness and tear osmolarity.
Not surprisingly, the majority of drops used by patients in the studies contained preservatives, most commonly benzalkonium chloride (BAK). This ingredient has been highlighted as one of the main culprits behind ocular surface irregularities in topically treated glaucoma patients; specifically, one large study identified BAK as the leading cause of drug-induced cicatrizing conjunctivitis in these patients. Another factor that appeared to correspond with tear film instability was the number of drops prescribed.
“Positive correlations between the number of topical IOP-lowering medications administered and the severity of signs and symptoms have been reported,” the researchers noted in their paper published in Ocular Surface. “Further, a positive correlation between the number of BAC-containing eye drops, ocular surface disease index, tear film breakup time and osmolarity was described.”
Compared with non-preserved drops, those containing preservatives seemed to have a more detrimental effect on the ocular surface and the occurrence of dry eye signs and symptoms. The researchers reported that dry eye signs including conjunctival redness, superficial punctate keratitis and blepharitis were all more common among users of preserved IOP-lowering medications. In addition, they noted that in more studies than not, “Both signs and symptoms of dry eye decreased upon changing from preserved eye drops to a preservative-free alternative.”
The current prevalence of ocular surface disease among glaucoma patients on IOP-lowering medication is between 39% and 75%. The mechanisms responsible for ocular surface alteration from BAK and ocular hypotensives still need to be studied, although literature suggests these effects are exerted by both the active pharmaceuticals and preservatives.
The researchers concluded from their review that prescribing preservative-free drops appears to help reduce the incidence of dry eye disease among the growing population of glaucoma patients.
Fineide F, Lagali N, Adil MY, et al. Topical glaucoma medications – clinical implications for the ocular surface. Ocul Surf. July 31, 2022. [Epub ahead of print]. |

