Most optometrists know very well that the members of the baby boom generation, and now even Generation X, who present to our offices have made near vision correction a priority. They feel the effects of accommodative loss every day—and they don’t like it. Our practices are filled with patients seeking, or at least amenable to, intervention. By the year 2020, 135 million Americans will be presbyopic.1 That’s a whopping 42% of the population.
What might be less well known, however, is that younger patients who are also current contact lens wearers but not yet presbyopic are just as committed to staying in contact lenses. The high rate of contact lens dropout doesn’t represent a loss of motivation—just an increase in frustration, in part due to issues with comfort, convenience and vision clarity.2 Given an option better suited to their visual and anatomic status, they would be elated to remain in contact lenses. Market research indicates that the number of patients who wear contact lenses peaks around those who are age 30 to 34, and then starts to dramatically decrease as these individuals enter their fourth decade of life (Figure 1). As their circumstances change, perhaps their lens modalities and care regimens should as well.
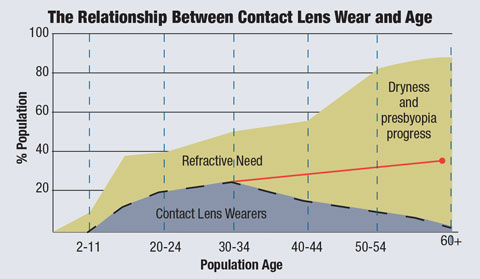 |
| Fig. 1. Contact lens wear begins to decline in conjunction with an increase in age, starting around age 30. The red line shows a projection of the potential lens-wearing population if dropouts could be eliminated. Source: Alcon. |
In short, our existing contact lens wearers don’t want to give them up, and presbyopes want to regain the visual function they have lost. These forces conspire to create an enormous opportunity for optometrists.
Surprisingly, of the approximately 40,000 optometrists in the United States, only 700 are fitting more than two multifocal contact lens patients per week—less than 2% total.3 With this large disconnect in adequately fulfilling the needs of the presbyopic patient, we need to ask ourselves: why do most of us shy away from proactively fitting multifocal lenses? Is it because of prior failures, increased chair time or preconceived assumptions about price sensitivity? Let’s dive into the nuts and bolts of what might hold us back, and discuss options for how we can overcome these obstacles.
An Expansion in Design
Available multifocal lens designs have historically fallen short of meeting either patient or doctor expectations. Early distance-centered lens designs failed to provide patients with adequate near acuity, while efforts to improve these lenses with the inclusion of multiple zones (i.e., concentric designs alternating distance and near) offered improved near vision but also distorted distance images, leaving patient satisfaction low. Additionally, available designs remained limited to select parameters while lens costs continued to run high, forcing many practitioners to return to more tried-and-true monovision fits as they enabled patients to function as efficiently as possible.
Fortunately, innovations made in the last decade in both designs and extended parameters have dramatically improved visual performance, providing us with better options with which to satisfy presbyopic lens wearers. Near-centered designs now overwhelmingly prevail, offering better near acuity, while peripheral distance zones typically now include smoother transitions.
These designs mimic the eye’s natural pupil function of miosis during accommodation to reduce interference with distance correction during reading; as such, when a patient wearing these lenses looks at a distance and their pupils widen, they receive adequate distance optics, allowing for less aberrations. The general increase in patient satisfaction—even the hard-to-fit emmetropic individuals can succeed with these lens designs—and the sheer number of presbyopes who are currently candidates for these lenses together has pushed the industry to continue with innovation in this lens category, offering wider parameters (in most cases +6.00 to -10.00 in 0.25 steps) and more materials than ever before in new aspheric designs. This portfolio helps to improve visual quality, comfort and convenience of wear, enabling more individuals then ever to enjoy these lenses, including those who might otherwise have worn glasses.
As an example, take this recent case seen at my practice: a 53-year-old female presented complaining of a change in near vision. She is in excellent general health and is not taking any medications other than nutritional supplements, but she has been a progressive spectacle wearer for the past four years. Though she reports that she does not mind the use of spectacles, she does point out that she is very active and involved in multiple sports and outdoor activities, which may not be the best place for spectacle wear. Her presenting uncorrected vision is 20/15 at distance and 20/60 at near with K readings of 42.50/42.50 OD and 42.25@030/42.50@120 OS and refraction values of +0.25-0.50x095 OD, +0.75-0.50x083 OS +2.00 add OU. Additionally, her slit lamp results indicated a reduced TBUT of eight seconds OD, six seconds OS and a grade 1 OD and grade 2 OS papillary response. Retinal exam findings were unremarkable OU.
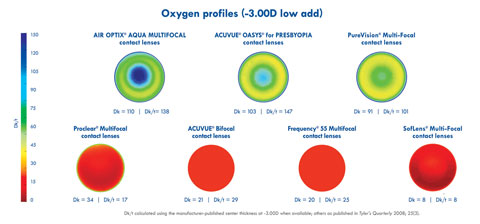 |
| Fig. 2. Oxygen transmissibility may be another factor in the determination of which multifocal lens to fit a patient with, as risk of dry eye may be a concern. Here are the oxygen profiles of several soft multifocal lenses on the market. Photo: Christine W. Sindt, OD, and Mandy Mataya Pietig, OD. Click to enlarge. |
She reported attempted use of soft contact lenses in the past (both in monthly and daily modalities) but ultimately had problems of unsuccessful comfort and fluctuating vision. The patient noted that along with not being able to read clearly through those lenses, she had also often developed redness and irritation after just one hour of lens wear. A daily disposable aspheric multifocal lens with BC 8.5, diam: 14.1, plano/med add OD, +0.25/med add OS; 20/20+ OU at distance; and 20/30 OU at near parameters was given to the patient at this point, with some fluctuations noted at near vision. Following the fitting process, a fit-guide recommendation and over-refraction data indicated that addition of a +0.25 OU did not blur distance vision and also enhanced her near vision to 20/30+ and decreased the fluctuations. The final lens dispensed to this patient was +0.25/med OD and +0.50/med OS, and she returned for follow-up at a later date reporting satisfaction with lens comfort and her new ability to experience a full day of wear without discomfort.
Chair Time
The historical failure of multifocal lenses has caused many practitioners to also believe that multifocal lens designs are complicated to fit and will significantly increase chair time to the point where it is not profitable. However, this scenario overstates the necessary time commitment. In reality, newer multifocal lens designs can achieve fitting success in less chair time than older designs. Though newer, better fitting guidelines are mostly responsible for this streamlining, it’s likely that eye care practitioners are also shedding old habits developed when fitting older designs. Much like any advancement in technology—be it cars, electronics, computers or medical devices—part of the product’s success is continued efforts to understand and incorporate it into daily life. As such, we must step back and familiarize ourselves with the optics of today’s multifocal lenses and have faith in the manufacturer’s guidelines.
However, the adjustments that a patient may need to enhance their vision are unique to the characteristics of both the individual and the lens they are wearing and must be approached with a trial-and-error mindset. Following the manufacturer’s fitting guidelines means that, for the most part, today’s multifocal fitting process should not take more than two patient visits; yet, this is not always the case. Take this patient example:
 |
| Table 1. Multifocal Soft Contact Lenses on the Market** Click to enlarge. Or click here to view PDF version. |
A 45-year-old female with a long history of successful gas permeable contact lens wear since her teenage years presented to the office with a complaint of decreased near vision with her single vision GP lenses. Vision with the lenses in question was 20/20 OU at distance and 20/40 OU at near. Her health history was negative, with no medications other than a multivitamin being taken, and her spherical GP lens fit appeared healthy with distance over-refraction recorded at plano in both eyes. Further examination revealed K readings of 41.75@021/42.50@111 OD and 41:50@167/42.25@077 OS and refraction values of -4.00, +1.00 add OU. The patient’s slit lamp and retinal examinations were both unremarkable OU.
The patient reported that she experienced high near demands while reading documents on the computer screen and expressed the desire not to sacrifice her distance vision or wear glasses over her GP lenses. She was refit into an aspheric GP lens design; however, upon return for follow-up, she reported the presence of shadows. Her distance vision and overall lens fit appeared adequate upon examination, but her near vision was reduced. The same lenses were ordered for a second time following a consultation with the GP lens lab, albeit this time with inclusion of a larger optic zone to improve the quality of the patient’s near vision. Parameters were BC 8.00, OAD 9.6, OZ 8.5, -4.50 with a +1.50 add OU; 20/30 OD, 20/25 OS and OU at distance; and 20/40 OU at near.
When questioned regarding the second pair of lenses, the patient said that she was content with her distance vision, but frustrated with her near ability. Wishing to improve her near vision and alleviate the continuing symptoms of shadow appearance, she was switched to a translating GP lens design with BC 8.10, OAD 9.5, Seg Ht 3.9 with a +1.00 add OU; 20/20 OU at distance; and 20/40 OU at near parameters. She reported achieving excellent distance acuity with the new translating lenses and also remarked that the shadows were gone, though now she had to move her head around to see clearly, which was leading to headaches at times.
Ultimately, the patient was moved to a monthly disposable silicone multifocal lens design, despite her history of successful GP lens wear. The new lenses were a three-zone aspheric design with parameters BC 8.5, Diam. 14.2, -4.00 Low Add OU; 20/20 OU at distance and 20/25 OU at near. The patient expressed resolution of all problems with wear of these lenses, as well as excellent distance vision and much-improved near acuity.
For this patient, the unique blend of the three-zone design was exactly what she needed to reduce the aberrations that the prior gas permeable lens designs had produced and the refit process took just two visits.
Matching the Lens to the Patient
Most manufacturers offer no-cost soft multifocal lens designs in a trial version to incorporate into practice. Because eye care practitioners often develop close bonds with their patients, however, in some cases lens costs can become a factor: fitting them into a trial lens and then discussing price later does not do them any favors. Additionally, withholding information about the latest technologies for fear of a price conversation is not the answer either.
Overall, practitioners must step back and actively inform patients of all current and new lens options and their prices prior to demonstrating any to them, so as to avoid any confusion. There are three distinct designs of multifocal lenses: concentric, aspheric and translating. Translating designs are predominantly used in rigid gas permeable fits and may require more customized placement of the segment height for near optics, while most soft multifocal designs incorporate aspheric designs with each manufacturer blending the near-center transition to distance zones in a proprietary way. Some patients fare better in some designs while others do well in others; materials may also play a factor in patient success (Figure 2). As such, it is beneficial for us to familiarize ourselves with all lens options available (Table 1).
Given the numerous innovations in multifocal contact lens design that have taken place in recent years, more comfortable new materials and the convenience of frequent lens replacement at a rate suitable to each patient’s lifestyle, our chances to succeed have never been greater. It is key to a practice’s success to approach these patients, and the multifocal lens category overall, with enthusiasm rather than trepidation. The state of the art will always continue to improve as manufacturers continue to refine their products, but today’s options are better than ever, and motivated patients fill our waiting rooms. Success is within your reach—and theirs.
|
1. Tan, J. Contact Lens Options for Presbyopia. Available at: www.siliconehydrogels.org/editorials/previous_editorial_jackie_tan.asp. Accessed July 15, 2016. 2. Reindel WT, Edmunds FR. A clinical assessment of presbyopic soft contact lens designs: comparing the impact of SofLens multifocal contact lenses and Acuvue bifocal contact lenses on successfully adapted monovision patients. Rev Optom. 2003 Apr 15;140(4). 3. Data on file, Alcon. |

