 |
History
A 42-year-old black male reported to the office with a chief complaint of red, irritated eyes that was present in both eyes, but worse in his left than his right. He explained that the redness had been progressively getting worse and was only temporarily relieved by an over-the-counter anti-allergy drop. His systemic and ocular histories were unremarkable and he denied exposure to chemicals or allergies of any kind.
Diagnostic Data
His best-corrected entering visual acuities were 20/20 OU at distance and near. His external examination was normal with no evidence of afferent pupillary defect. The pertinent anterior segment findings are demonstrated in the photograph. Goldmann applanation tonometry measured 15mm Hg OU. Dilated funduscopy was within normal limits in both eyes, revealing slightly asymmetric cup-to-disc ratios measuring 0.4/0.4 OD and 0.4/0.55 OS with normal peripheries.
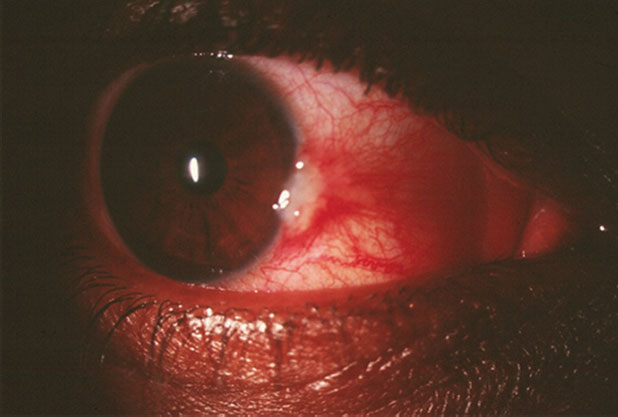 |
| This patient’s red eye has been getting progressively worse. Can anything about this image and the diagnostic data help explain why? Click image to enlarge. |
Discussion
Additional testing included the topical phenylephrine blanch test to ascertain the depth of the inflammation. Immediate blanching of the vessels indicates superficial involvement while persistence of injection indicates deeper inflammatory involvement as seen in episcleritis or scleritis. Additional history must include questions regarding pain. Indications of severe ocular pain, photophobia or pain upon eye movement suggest episcleral or scleral inflammation while minimal pain suggests superficial inflammation. In this instance, a lack of pain upon eye movement, even during the worst period of inflammation suggested a superficial process rather than a deeper one. Lid eversion should be done to rule out unforeseen foreign bodies and matter as well as permit inspection of the superior palpebral conjunctiva for papillae, follicles or scarring. Exophthalmometry could be considered to rule out proptosis and potential exposure with desiccation. Schirmer tear testing and Meibomian gland inspection could be completed to rule out ocular tear deficiency and evaporative ocular surface disease. Unrelated to the chief complaint visual fields (VF), optical coherence tomography (OCT) and photos should be obtained to establish a baseline for what could be considered a borderline glaucoma suspect based upon the asymmetric C/D ratio.
The diagnosis in this issue is pingueculitis. Pingueculae are characterized by yellowish, slightly raised, interpalpebral lipid-like deposits in the nasal and temporal limbal conjunctiva.1-3 They frequently are found in individuals who are middle-aged and who experience chronic exposure to the sun.1-3 The recent literature has uncovered evidence that suggests risk factors to their formation and severity include diabetes mellitus, the presence of thyroid orbitopathy and contact lens wear (rigid and soft).4-6 There is no predilection for sex or race.1,2 In most instances, pingueculae are an ancillary finding, causing little, if any, ocular symptoms. They can lead to the formation of pterygia. Both pingueculae and pterygia can become vascularized and inflamed, and may be associated with corneal punctate epitheliopathy and corneal dellen (corneal thinning secondary to dryness).1,2 Pingueculitis occurs when a pinguecula becomes acutely inflamed.3 The result is an acute vascularized, red, irritated and symptomatic red eye.3
Additional QuestionsWhen a patient with this kind of presentation is in your office, be sure to ask the right questions. You’ll want to ask if they experience:
|
Pinguecula formation is typically seen in the older population and is considered by most researchers to be a conjunctival degenerative processes initiated by exposure to both noxious environmental stimuli (solid, liquid or gas) and UV light.1,2,7 The presence of pinguecula can serve as an index to exposure of irradiation of ultraviolet rays and decreased antioxidant activities.7 Advanced glycation end (AGE) products are deposited in the target organ of ageing tissues.7 AGEs accelerate the process of ageing and have been detected in the subepithelial amorphous deposits of pinguecula.7 Pinguecula can be considered as an aggregation of AGE-modified proteins.7
The initial lesion results from chronic solar radiation, which alters the collagen and elastic tissues of the conjunctival stroma leading to elastotic degeneration of collegen fibers and deposition of abnormal elastic fibers in the conjunctival substantia propria with an increased population of metabolically active stromal fibrocytes.1,3
Once a pinguecular elevation forms, depending upon its size, the tear film may become thin and discontinuous in that zone, producing a bed of dryness. This can lead to corneal dehydration and dellen formation. As pinguecula is a condition of abnormal epithelial differentiation, squamous cell proliferation and cellular metaplasia produce instability of the tear film.7 When these lesions succumb to various environmental factors they become inflamed, allowing the release of histamine, seratonin, bradykinin and prostaglandins, producing the acute symptoms that characterize pingueculitis.1-3 In severe cases the conjunctival surface may become sufficiently dry to cause microulceration of the conjunctival epithelium.1 When this occurs, the eye protects itself by attempting to cover the erosion, leading to pterygium formation.1,8
Management of pinguecula based on symptomatology.1-3 For patients with occupations or hobbies that increase the risk of pinguecula, counseling should be provided on the preventative benefits of sunwear, UV-blocking coatings or goggles that limit dust exposure.
In cases of mild pingueculitis, where symptoms are mild or when dellen are present, the use of cold compress and ocular lubricating drops or ointments are indicated. When symptoms and inflammation become more significant, appropriate short term use of topical steroids, used Q2H to QID will assist in resolution.
Surgical resection is indicated in severe cases where pterygia are present and are interfering with vision, contact lens wear or corneal wetting.
Chronic renal failure has the ability to produce calcification within the conjunctiva. This can be clinically indistinguishable from pingueculitis.9,10 In these patients, calcium phosphate salts deposit as the kidneys fail. Histopathologically polymorphonuclear leucocytes are also present in the inflamed tissues.9,10 Historically speaking this condition must be investigated to rule out the need for life saving interventions.
In this case, the patient was treated with Tobradex ST (tobramycin, dexamethasone, Alcon) QID and lubrication with reassessment in one week. The patient was counseled to use ultraviolet light (UV) protection in their spectacles or don sun wear with UV protection and avoid dusty environments or protect against them with safety eyewear. At the one-week follow-up, significant improvement was apparent. The antibiotic-steroid combination was discontinued because it was determined there was no reason to continue the antibiotic portion of the therapy. The steroidal portion of the therapy was continued in a slow taper over two weeks with prednisolone acetate. Intraocular pressure was monitored at all visits and the condition resolved without complication.
1. Sowka J, Gurwood A, Kabat A. The Handbook of Ocular Disease Management, 9th edition. Review of Optometry (Supplement). 2007;144(3):1A-64A. 2. Mimura T, Usui T, Obata H, Yamagami S, et al. Severity and determinants of pinguecula in a hospital-based population. Eye Contact Lens. 2011;37(1):31-5. 3. Azhar SS. Acute red eye. Pingueculitis. Am Fam Physician. 2007;76(6):857-8. 4. Mimura T, Obata H, Usui T, Mori M, et al. Pinguecula and diabetes mellitus. Cornea. 2012;31(3):264-8. 5. Mimura T, Usui T, Mori M, et al. Pinguecula and contact lenses. Eye (Lond). 2010;24(11):1685-91. 6. Ozer PA, Altiparmak UE, Yalniz Z, et al. Prevalence of pinguecula and pterygium in patients with thyroid orbitopathy. Cornea. 2010 ;29(6):659-63. 7. Kaji Y, Oshika T, Amano S, et al. Immunohistochemical localization of advanced glycation end products in pinguecula. Graefes Arch Clin Exp Ophthalmol. 2006 ;244(1):104-8. 8. Dong N, Li W, Lin H, et al. Abnormal epithelial differentiation and tear film alteration in pinguecula. Invest Ophthalmol Vis Sci. 2009 ;50(6):2710-5. 9. Klaassen-Broekema N, van Bijsterveld OP. The red eye of renal failure: a crystal induced inflammation? Br J Ophthalmol. 1992;76(10):578-81. 10. Klaassen-Broekema N, van Bijsterveld OP. The role of serum calcium in the development of the acute red eye in chronic renal failure. Eur J Ophthalmol. 199;5(1):7-12. |

