 |
A 69-year old white female presented for an eye exam and reported difficulty reading fine print for the past several months. Her last eye exam was approximately three years earlier. The patient received her current eyeglass prescription at that visit. Also, she underwent successful cataract surgery in each eye about five years earlier.
The patients medical history is significant for a primary left breast carcinoma in 1999 for which she underwent a mastectomy and chemotherapy. She also had a primary bladder carcinoma. Both cancers, she said, were in remission, and she claimed to otherwise be in good health.
Best-corrected visual acuity at this exam measured 20/20 in each eye. Confrontation visual fields were full to careful finger counting in both eyes. Extraocular motility testing was normal. Both pupils were equally round and reactive to light, and there was no afferent pupillary defect in either eye. The patients anterior segment exam was unremarkable.
Dilated fundus exam revealed that the optic nerves were healthy in both eyes, with small cups and good rim coloration and perfusion. The vessels and maculae were normal in each eye.
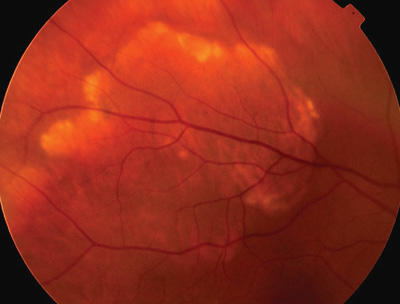 |
| Dilated fundus exam revealed this suspicious white lesion along the superior temporal arcade of the right eye. |
Take the Retina Quiz
1. What additional testing would be most helpful in making the correct diagnosis?
a. Optical coherence tomography.
b. Fluorescein angiography.
c. Echography.
d. Chest X-ray.
2. What is the likely etiology of this patients condition?
a. Idiopathic.
b. Primary malignancy.
c. Metastatic disease from the breast or bladder.
d. Thyroid.
3. What is the correct diagnosis of this patient?
a. Sclerochoroidal calcification.
b. Metastatic carcinoma.
c. Choroidal melanoma.
d. Osteoma.
4. How should this patient be managed?
a. Observation.
b. Plaque radiation followed by chemotherapy.
c. Workup to determine abnormal calcium deposition.
d. Enucleation.
5. What is the patients overall prognosis with this condition?
a. Excellent.
b. Fair with appropriate treatment.
c. High probability of death within five years.
d. Death within one year.
For answers, go to bottom of page.
Discussion
On clinical examination, calcium deposition was evident along the edges of the large plaque-like lesion. Also, the retinal pigment epithelium (RPE) was thinned and atrophic in the center, allowing us to easily see the choroidal vasculature.
Although we were concerned that these findings were a metastatic lesion, sclerochoroidal calcification was at the top of our differential diagnosis list based on the clinical appearance and calcium deposition. We obtained an ultrasound, which showed a high reflective area of fundus calcification typical for sclerochoroidal calcification.
Sclerochoroidal calcification is a relatively newly identified entity. Early reports associated it with hyperparathyroidism, but by the mid-1990s, clinicians recognized it as a distinct ophthalmic entity.1,2
This benign condition typically occurs in the elderly population. However, it can also be seen in younger patients who have one of several systemic associations, as discussed below.
The hallmark feature of sclerochoroidal calcification: white areas of calcification that can appear as a yellow halo around an area of RPE atrophy, as in our patient, or as a solitary yellow homogeneous lesion. They are usually located along the superior or inferior arcades and are often bilateral.3
The origin of the lesion likely begins in the sclera and ultimately extends into the choroid. In some instances, the external extension of the lesion is seen near the horizontal rectus muscles, giving an appearance similar to senile hyaline plaques. In fact, senile hyaline plaques seen in the elderly also show calcium deposition.
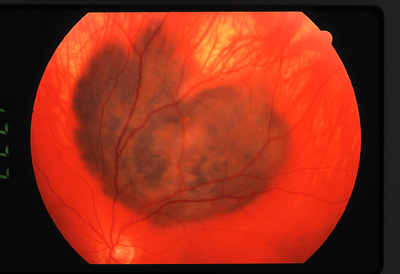
The differential diagnosis includes metastatic carcinoma, choroidal melanoma and osteoma. At the ocular oncology service at Wills Eye Hospital, Philadelphia, the referring diagnosis in more than a quarter of the patients who have sclerochoroidal calcification is choroidal metastasis followed closely by choroidal melanoma.3
 |
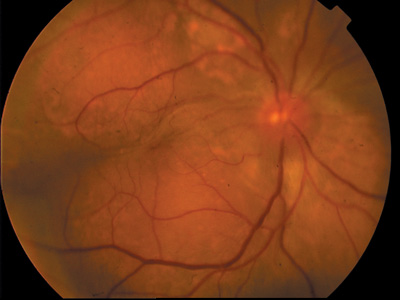 |
|
The differential diagnoses for our patient include primary malignant choroidal melanoma (left), as seen here in another patient, and choroidal metastasis (right), as seen in a patient who has a history of thyroid cancer. |
We can usually diagnose the patient based on clinical appearance, but standardized ultrasound (echography) and computed tomography (CT) can provide the most useful information to confirm the diagnosis.
On B-scan, the calcific plaque can be easily seen at the level of the sclera and choroid; these appear as a high reflective spike on A-scan. Calcium also shows up on CT scan.
Most cases of sclerochoroidal calcification are idiopathic in nature. Still, we must rule out several systemic associations, such as hyperparathyroidism and pseudohypoparathyroidism; these were present in the patient in whom researchers initially identified sclerochoroidal calcification.
Abnormal calcium metabolism can also lead to the development of these lesions. Calcium pyrophosphate deposition disease (pseudogout) is one such disease that is associated with abnormal calcium metabolism.3
The overall prognosis is very good in a patient who has the idiopathic form of sclerochoroidal calcification. Thats because the lesions rarely change, and they do not affect visual acuity.
Our patient was given a new prescription for glasses. In addition, she underwent a workup to determine if she had abnormal calcium metabolism, but the workup was negative. We continue to observe her without any change in the lesion. She remains free of any metastatic disease from her breast or bladder carcinoma.
1. Goldstein BG, Miller J. Metastatic calcification of the choroid in a patient with primary hyperparathyroidism. Retina 1982;2(2):76-9.
2. Sivalingam A, Shields CL, Shields JA, et al. Idiopathic schlerochoroidal calcification. Ophthalmology 1991 May;98(5):720-4.
3. Shields JA, Shields CL. CME review: sclerochoroidal calcification: the 2001 Harold Gifford Lecture. Retina 2002 Jun;22(3):251-61.
Answers: 1) c; 2) a; 3) a; 4) c; 5) a.

