41st Annual Technology ReportFollow the links below to read other articles from annual update on technology: |
The wearable display industry is developing and commercializing headsets and eyewear that enable applications with broad benefits for health care, education, entertainment and more. However impressive they are, these technologies raise some concerns and opportunities for optometrists. What impact could these devices have on eye health and vision by potentially increasing blue light exposure, presenting new peripheral focal demands and creating untested strains on convergence and accommodation?
Eye care needs to define the categories of impact on the eye and vision and invite good research to investigate the reality of the emerging extended reality. Practitioners also have an opportunity for intervention when clinical signs and symptoms present.
 |
| Virtual reality headsets, such as the one seen here, fully occlude a room’s light and fit close to the user’s face. |
A New Reality
Extended reality (XR) is a term that encompasses virtual reality (VR), mixed reality (MR) and augmented reality (AR).1 Research into the development of wearable XR devices cites concern for convergence-accommodation conflict.2 The developers also cited the issues with size and weight of wearable headsets, along with the heat generation inherent with displays, like other light sources, that convert a portion of energy to heat.
Optometry is primarily concerned about high-energy blue light exposure, visual task-exacerbated dry eye, the role of sustained near-centered tasks on refractive error development and the role of peripheral focus or defocus on refractive error development.3-5 Other concerns include visual field obstruction, the potential for cybersickness, increased asthenopia and headache, fatigue and sleep disorders.6-8
A paucity of data and controlled studies support the concerns or estimate the risk levels from a safety perspective. Using a near eye display is clearly different from any normal visual task. Near eye display viewing is not something the natural eye can accomplish without optics in the system or novel imaging technology. Wearable displays represent a new manner of using the eyes, along with a new set of visual and perceptual stimuli.
A goal of wearable display design is to minimize the stimulus for accommodation for the plane of the display content. It is ideal if there is no, or at least minimal, demand for accommodation and, in the absence of three-dimensional scenes, no demand on convergence. The developers could argue that display use free of a demand on accommodation and convergence does not present a new manner of using the eyes. Even so, the display itself presents a proximal stimulus, the display content is dynamic and 3D is and will be a common property of display content.
The lack of controlled studies creates the need for conversation before drawing unsubstantiated conclusions on one side of the controversy or the other. It would be unfair and dangerous to move quickly from theory to doctrine and doctrine to dogma with regard to the safety or dangers of wearable display use.
How It Works
Wearable displays have two main components. The first is the means of generating the display; the second is the optics that allow viewing of the display. The digital display in the headset or eyewear is electronic and delivered in the spectacle plane or the plane of the headset. The optics are a means of providing the dioptric power needed to see the display content.
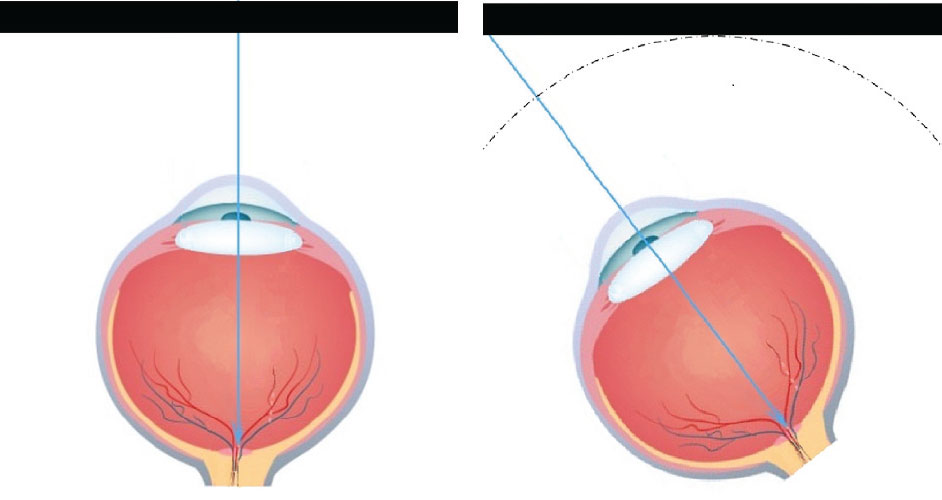 |
| The distance from the eye to the flat panel display is greater at the edge than in the center, resulting in a lower focal demand at the corners and edges than in the center. Click here to enlarge image. |
Displays can be occluded or transparent. All VR systems use occluded displays, many in the form of headsets that fully block the real world while providing wide field of view displays. The displays are flat panels that may one day be curved. The flat panel presents a challenge to have adequate depth of focus in the optical system because the corners of the display are a greater distance from the center of rotation of the eye than the center of the display when placed at the pupillary distance (PD) of the user.
Transparent displays are produced by using a combiner. The combiner can be something like a beam splitter in a biomicroscope that allows a camera to capture the same image that is being viewed by the practitioner. This form of combiner requires focusing optics. Other forms of optical combiners exist and wave-guides are the most frequently used systems. Light is guided by nano-channels in the spectacle lens to reflecting elements that direct each pixel of the display to the eye without a focal demand. Most wave-guide displays do not require optics to focus the light.
Light-field technology is another method of producing a transparent display that does not require optics between the display and the eye. In an oversimplified description, this employs layers of transparent displays to produce pixels that can accommodate different refractive states and focal demands and does not require focusing optics.9
Not all transparent displays impact the eye and vision in the same way. Each must be studied clinically to understand the relative impact regarding binocular vision demands, field obstruction, cybersickness, asthenopia, headache, fatigue, blue light hazard, dry eye and mood and sleep disorders.
The second display component is the optical element that allows for viewing the near eye display.
All commercialized VR systems employ geometric optics in the form of high plus lenses in their headsets, similar to a Keystone stereoscope. The designers use adaptive optics to control the distortions of high plus lenses and manage the problem of the variation from the center to the corners of the flat panel distance from the eye. The inherent reduced size of the exit port or eye-box limits users’ ability to make full versions when viewing. This narrow range of eye movement may be an issue with long-term use of VR headsets. Even so, humans rarely make versions greater than 25 degrees due to the phenomenon of head movement propensity.
Contact lenses and intraocular lenses (IOLs) are in development to eliminate the need for optics in the display system.10 One design incorporates a central micro-lens to focus the display and incorporates a light-polarizing or spectral filter that prevents the display light from passing through the normal refractive correction optic zone. The eye-borne optics are engineered for wide field of view and extended depth-of-field.11 This optical solution potentially allows any display otherwise requiring geometric optics to be viewed in the spectacle plane without the geometric optics in the system. The eye-box limitation of geometric optics in a VR system is thereby eliminated, and the eye is free to make full versions.
Commercialized XR display headsets and eyewear products can be binocular or monocular. Of the binocular products, only a few offer limited pupillary distance (PD) adjustments. The need for a range of PD for the wearable display headsets and eyewear is expected, due to the distribution of PD across the population. The chromatic aberration of the high-powered geometric optic increases with the angle of off-axis viewing, and a relative vergence demand increases with a user’s PD that departs significantly from the average or pre-set PD. Clinicians can help patients understand the limitations of the XR devices when they have a PD that is significantly wider or narrower than the mean PD incorporated in the device.
Most all XR display headsets and eyewear to date do not incorporate individual prescriptions. Refractive errors affect an estimated 68% of American adults, with 66% wearing some type of eyewear (eyeglasses, contact lenses, reading glasses).12 Users must wear additional eyewear behind the headsets, wear contact lenses or perform the task without their respective refractive corrections when the prescription is not incorporated in the headsets or display eyewear. Companies are producing refractive correction lenses for placement between the geometric optics or displays and the eye as an alternative to wearing conventional spectacles in addition to the headset.13 The solution of wearing contact lenses to manage refractive correction with wearable displays may support a forecast for a new reason for consumers to wear contact lenses. Providing refractive correction with XR devices is a clear opportunity for eye care practitioners and strong reason for adding a case history question regarding the use of XR headsets and eyewear.
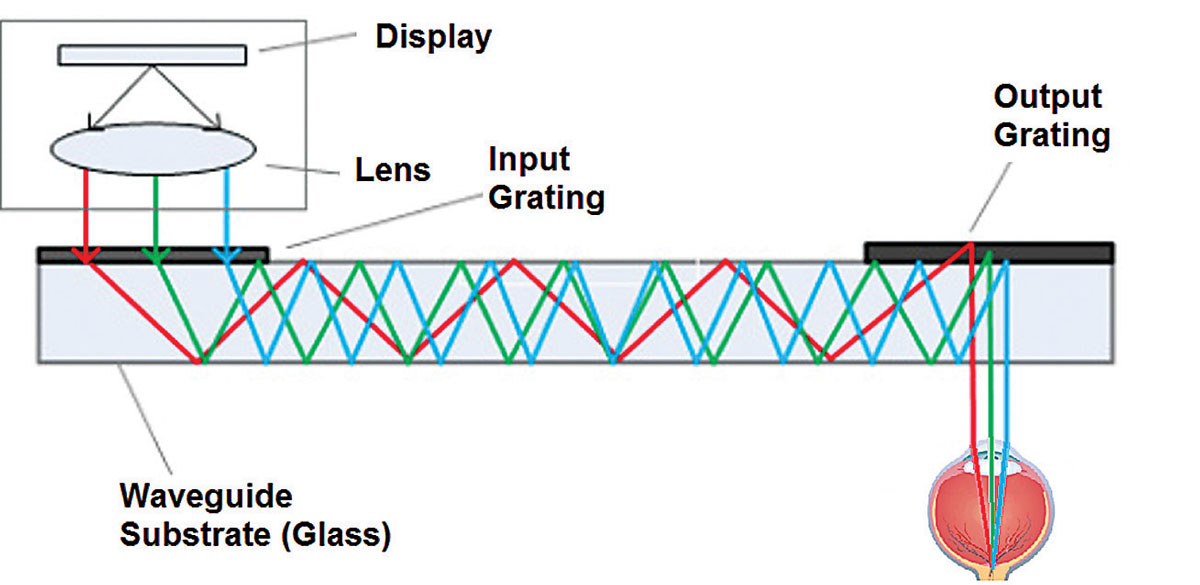 | |
| Above, wave-guide channels and reflectors direct individual pixels of light toward the eye to create a transparent display that also allows simultaneous viewing of the real world. At right, a beam splitter as a combiner allows for simultaneous viewing of virtual content and the real world. | 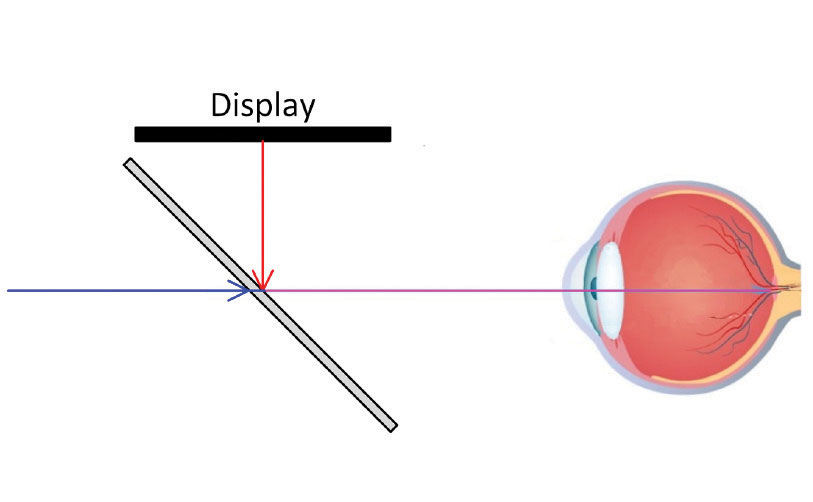 |
Are Wearables Bearable?
The most well-understood concern with binocular wearable displays is convergence-accommodation conflict.14 The display is in a fixed plane in a headset or in the spectacle eyewear. While demand on accommodation is fixed, the binocular content can vary in its stimulus for convergence. The disparity that produces stereovision, or 3D, can stimulate convergence, which in turn stimulates accommodation. The fixed plane of the display does not allow accommodation without blurring of the image. The result is a conflict wherein the image can be blurred and single or clear and with a vergence demand.
This conflict is known to cause fatigue and discomfort for some users.15 Efforts to increase the depth of focus of the optical system can mitigate this conflict by allowing the eye to accommodate with convergence without the concomitant blur, as an increased depth of focus should keep the image clear with convergence accommodation. Some wearable display systems are expected to have more or less convergence accommodation conflict than others.16
Many questions will remain unanswered: Will we find a higher incidence of symptoms in patients who are also found to have weaker binocular vision measures? What intervention strategies do we envision beyond suggesting discontinuation of use of the XR devices?
Thus far, the eyewear form factor wearable displays have frames that house the display technology, including the electronics and, in some cases, the power supplies. Field obstruction results when the frame end-pieces and temples are larger than conventional frame designs and occlude a portion of the visual field. Safety concerns may arise from the reduced peripheral awareness when performing activities while wearing display eyewear that obstructs the visual field.
Computer Blues
The ophthalmic industry has embraced a concern for risks of exposure to high-energy visible blue light.17 The wavelength of high-energy visible blue light that was studied on explanted retinal tissue is 405nm.18 The range of wavelength for the theoretical risk to photoreceptors includes 400nm to 430nm. liquid-crystal display (LCD) and organic light-emitting diode (OLED) displays are different from each other in that an LCD display is back-lit, while the OLED emits the light directly. The blue light emitted in each case is centered in the range of 445 to 465nm and not in the 400nm to 430nm range.19
Sunlight and micro-displays are not equivalent with regard to the significant spike in the range of theoretical concern. The spectral power distribution comparison must also be analyzed in the context of the luminance to understand the relative exposure of photoreceptors to the theoretically harmful visible blue light. Sunlight, on an average day, has a luminance of 35,000 candela per meter squared, while the average display brightness when used indoors has a luminance of 250 candela per meter squared.20 The luminance difference alone in the absence of the fact that the spectral power distribution has more visible blue light in the 400nm to 430nm range in sunlight suggests that the total retinal exposure to high-energy visible blue light is greater in five minutes of average daytime sunlight than it is in more than 11.5 hours of wearable display use.21 The outcome is similar for computer monitors that have a luminance in the range of 250 to 500 candela per meter squared.22
The concern for visible blue light hazard will become more relevant when display luminance increases above the 1,000 candela per meter squared level and if the band of blue light shifts to lower wavelengths. The Laws and Regulations for Radiation Emitting Products of the Food and Drug Administration provide guidance for display products issues related to electromagnetic radiation.23 Blue light hazard is not listed as a specific consideration in this guidance.
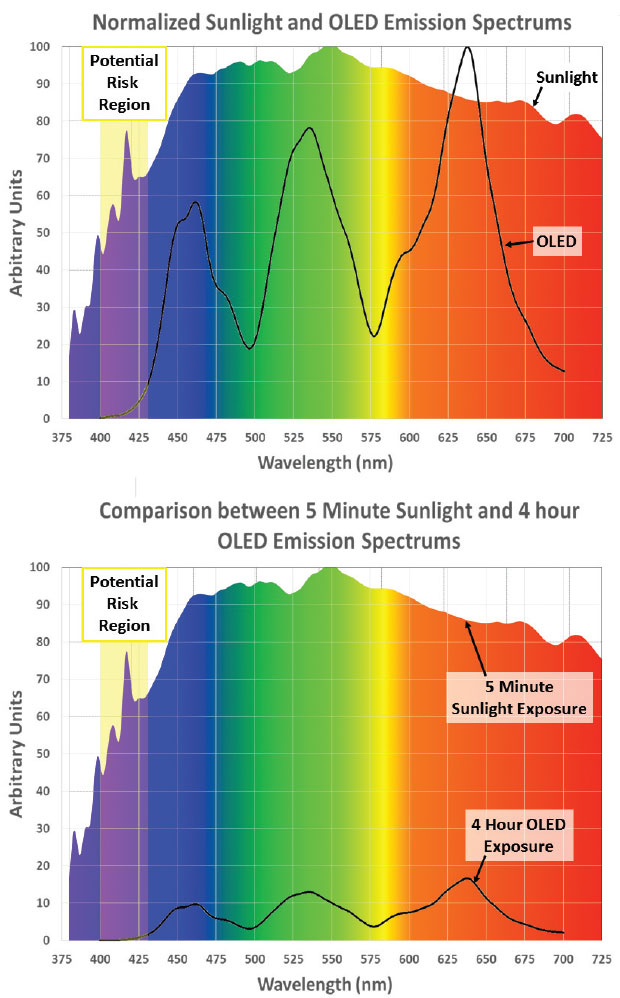 |
| Display blue light’s peak wavelength has lower energy, and the relative intensity of display light is significantly lower. |
The correlation of use of computer displays in general with sleep disorders is a current concern.24 The same is expected with the use of wearable displays. The wavelength of light known to suppress melatonin through the non-visual retinal pathway of the intrinsically photosensitive ganglion cells is 460nm to 480nm.25 The wavelength emitted by electronic micro-displays, including those used in wave-guide and light-field technology, fall in this range. Sleep disorders are one known result of continual visible blue light exposure in this wavelength. The absence of exposure to wavelengths in this range also causes sleep disorders due to the need for circadian rhythm that is made possible by alternate suppression and subsequent production of melatonin. It is straightforward to create smart eyewear that reduces the blue light emission based on a pre-determined sensing or signal, to shift the exposure to the visible red light to stop the melatonin suppression in an effort to restore normal circadian rhythm.
Incorporating technology that modulates the chromaticity of the display output such as f.lux and Apple’s Night Shift feature can also regulate the different bands of visible blue light toward these same ends. Eye care practitioners may choose to investigate the number of hours per day of their patients’ use of XR headsets and eyewear and consider recommendations for reducing the time of exposure to visible blue light or the use of contact lenses that filter the majority of the band between 400nm and 430nm while exercising caution in over-filtering the band between 460nm and 480nm.
On the Blink
Dry eye symptoms or disorders are a concern with sustained visual tasks. One cause is a reduced blink rate or quality that occurs with concentrated visual tasks.26 The reduced blink rate is correlated with greater evaporation of the tears. Observations with the use of VR headsets appear to support that they are sealed and warm. It is possible the VR headsets may have a therapeutic benefit due to the goggle effect, known to increase the relative humidity around the eye is known to have therapeutic value for evaporative dry eye.27 Even so, there is an opportunity to investigate signs and symptoms of dry eye in patients who report multi-hour use of XR devices.
Cybersickness—also called simulator sickness—is a form of motion sickness associated with VR environments.28 A disagreement with visually perceived movement and movement sensed by the vestibular apparatus is the likely cause.29 The otoliths and semicircular canals, along with proprioceptors within muscles of the body, may not send the same movement signals as the visual system during wearable display use.30 The vestibular apparatus may signal a stationary position while the visual content signals rapid motion or shifts in the position of objects relative to ego-centric localization. The experience of cybersickness may be different with fully occluded VR systems than with AR and MR systems that allow a peripheral lock on the real world. There is an opportunity to investigate vision therapy strategies for patients who use XR headsets and eyewear and report symptoms of cybersickness.
Use of near eye displays may also play a role in refractive error development. One study reported correlation between sustained near centered tasks and development of myopia.31 The correlation of sustained near tasks and myopiagenesis is without a well understood mechanism. Correlation and causation are not the same. The cause may be the absence of outdoor activity in individuals who engage in near work for long periods. More research is needed to strengthen the evidence basis for the role of sustained close work and myopiagenesis in general and to see if a correlation also exists with wearable display use in particular.
A second factor in myopiagenesis is the peripheral focus, or defocus, of the optical system of the wearable display. The evidence of the role of peripheral defocus in regulating myopia supports the value of a myopic peripheral defocus while the central image falls on the fovea.32 A myopic peripheral defocus occurs when on- and off-axis peripheral imaging is focused in front of the peripheral retina and is held to be advantageous in reducing the progression of myopia. The flat panel display in conjunction with all geometric optics including eye-borne optics results in the peripheral retinal image of a VR display being focused in front of the retina, because the peripheral display is further from the eye and, therefore, has a lesser focal demand while being focused by the same dioptric power.
The optical modeling of the current flat panel and geometric optics supports that the use of wearable displays is expected to inherently provide a therapeutic myopic defocus image shell. Such an effect will be produced even when a curved display is available with curvature equivalent to the base curve of a spectacle lens, since the periphery of the display will be further from the eye than the center of the display.
In the long-term, the eye care community will benefit from studying refractive error development in users of XR systems to determine if there is therapeutic value or otherwise.
What to Watch and What to Do
It’s the job of clinical researchers to evaluate the impact these wearable displays may have on visual performance and eye health. The potential for harnessing this technology for personal and professional use in surgical visualization, situation awareness, patient engagement while accessing electronic medical records, visual rehabilitation, low vision and continuing education is significant. Consumers are already adopting the technology at a high rate and will seek our care when symptoms and challenges to adaptation occur. There are pitfalls in making hasty causal conclusions whether positive or negative with regard to the impact of the technology. The XR industry has already spent billions of dollars in research and development and is aiming high. They are expected to do anything and everything they can to mitigate real problems.
Controlled clinical investigations are needed, along with peer-reviewed case studies, to provide an evidence basis for conclusions about the technology that is emerging and that will usher in a widespread change in how our patients will be using their eyes and vision. In the meantime, practitioners have an opportunity to apply the art and science of vision care as intervention for patients who struggle to adapt to the XR headsets and eyewear, and who report symptoms or have clinical signs related to the anticipated problems with convergence accommodation conflict, high-energy visible blue light exposure, visual task-exacerbated dry eye, emerging myopia, cybersickness, field obstruction, increased asthenopia and headache, fatigue and sleep disorders.
Dr. Legerton is the co-founder of SynergEyes and Innovega.
Ms. Segre has served in eye care journalism for 24 years and is the founding editor of allaboutvision.com.
Mr. Marsh has a Masters in Mechanical Engineering, Cal Poly Pomona and serves as the vice president, engineering for Innovega.
|
1. Fink C. War of AR/VR/MR/XR Words. Forbes. www.forbes.com/sites/charliefink/2017/10/20/war-of-arvrmrxr-words/#7f99f4b58d07. October 20, 2017. Accessed August 28, 2018. 2. Zhang S. The obscure neuroscience problem that’s plaguing VR. Wired. www.wired.com/2015/08/obscure-neuroscience-problem-thats-plaguing-vr/. August 11, 2015. Accessed August 11, 2018. 3. Tosini G, Ferguson I, Tsubota K. Effects of blue light on the circadian system and eye physiology. Molecular Vision. 2016;22:61-72. 4. Moon J, Kim K, Moon N. Smartphone use is a risk factor for pediatric dry eye disease according to region and age: A case control study. BMC Ophthalmol. 2016;16:1:188. 5. Mutti D, Mitchell G, Moeschberger M, et al. Parental myopia, near work, school achievement, and children’s refractive error. Invest Ophthalmol Vis Sci. 2002;43(12):3633-40. 6. LaViola J. A discussion of cybersickness in virtual environments. SIGCHI Bulletin. 2000;32(1):47-56. 7. Rebenitsch L, Owen C. Review on cybersickness in applications and visual displays. Virtual Reality. 2016;20(2):101-25. 8. Christian C. Evening exposure to a light-emitting diodes (LED)-backlit computer screen affects circadian physiology and cognitive performance. J Appl Physiol. 2011;110(5):1432–8. 9. Simonite T. How magic leap’s augmented reality works. MIT Technology Review. www.technologyreview.com/s/532001/how-magic-leaps-augmented-reality-works/. October 23, 2014. Accessed August 17, 2018. 10. Legerton J. Technology in your practice; contact lenses of the future are not as far off as you might think. Contact Lens Spectrum. 2017;32(8):28-34. 11. Sprague R, Schwiegerling J. Full field-of-view augmented reality using contact lenses. Paper presented at the Interservice/Industry Training, Simulation, and Education Conference, November 29-December 2, 2010; Orlando, Fla. 12. National Eye Institute & Lions Clubs International Foundation. 2005 survey of public knowledge, attitudes, and practices related to eye health and disease. Bethesda, MD: National Eye Institute. (2007). 13. Luxexcel to 3D print optical prescription lenses for Vuzix AR headsets. 3ders. www.3ders.org/articles/20180105-luxexcel-to-3d-print-optical-prescription-lenses-for-vuzix-ar-headsets.html. Jan. 5, 2018. Accessed August 17, 2018. 14. Kramida G, Varhney A. Resolving the vergence-accommodation conflict in head mounted display. University of Maryland. www.cs.umd.edu/sites/default/files/scholarly_papers/Kramidarev.pdf. Accessed August 17, 2018. 15. Hoffman D, Girshick A, Akeley K, Banks M. Vergence–accommodation conflicts hinder visual performance and cause visual fatigue. J Vis. 2008;8(3):33.1–30. 16. Lanmann, D. Near-eye light field displays. NVIDIA Research. talks.stanford.edu/douglas-lanman-near-eye-light-field-displays/. October 9, 2013. Accessed August 17, 2018. 17. Flint Ford H. Learn the science and key clinical points to help educate—and ultimately protect—your patients. Rev Optom. 2016;153(4):88-93. 18. Roehlecke C, Shumann U, Ader M, et al. Influence of blue light on photoreceptors in a live retinal explant system. Molecular Vision. 2011;17:876-884 19. Triggs R. AMOLED vs LCD: differences explained. Android Authority, February 8, 2016 https://www.androidauthority.com/amoled-vs-lcd-differences-572859/. Accessed August 15, 2018. 20. Guttag K. ODG R-8 and R-9 Optic with a OLED Microdisplays (Likely Sony’s). Karl Guttag on Technology. January 4, 2017. www.kguttag.com/2017/01/04/odg-r-8-and-r-9-optic-with-a-oled-microdisplays-likely-sonys/. Accessed August 15, 2018. 21. Halsted C. Brightness, luminance, and confusion. Information Display. 1993;9(3):21-4. 22. Dohrman P. How to measure the brightness of computer monitors. Techwalla. www.techwalla.com/articles/how-to-measure-the-brightness-of-computer-monitors. Accessed July 7, 2018. 23. Radiation Control Act. FDA. www.fda.gov/radiation-emittingproducts/electronicproductradiationcontrolprogram/lawsandregulations/ucm2007155.htm. March 22, 2018. Accessed August 17, 2018. 24. Volpi D. Heavy technology use linked to fatigue, stress and depression in young adults. Huffington Post. October 2, 2012. Accessed August 17, 2018. 25. Turner P, Van Someren E, Mainster M. The role of environmental light in sleep and health: Effects of ocular aging and cataract surgery. Sleep Med Rev. 2010 Aug;14(4):269-80. 26. Acosta M, Gallar J, Belmonte C. The influence of eye solutions on blinking and ocular comfort at rest and during work at video display terminals. Exp Eye Research. 1999;68(6):663-9. 27. Korb D, Blackie C. Using goggles to increase periocular humidity and reduce dry eye symptoms. Eye & Contact Lens. 2013;39(4):273-6. 28. Virre E. Virtual reality and the vestibular apparatus. IEEE Engineering in Medicine and Biology Magazine. 1996;15(2):41-43, 69. 29. Barrett G, Thornton C. Relationship between perceptual style and simulator sickness. J Applied Psychol. 1968;52(4):304-8. 30. Mittelstaedt J. Effects of display type and motion control on cybersickness in a virtual bike Simulator. Displays:51.2018:43–50. 31. Jones-Jordan L, Sinnott L, Cotter S, et al. Time outdoors, visual activity, and myopia progression in juvenile-onset myopes. Invest Ophthalmol Vis Sci. 2012 Oct 1;53(11):7169-75. 32. Smith E. Prentice award lecture 2010: a case for peripheral optical treatment strategies for myopia. Optom Vis Sci. 2011;88(9):1029-44. |

