Cataracts are one of the leading causes of blindness in the United States and the world, and a diagnosis we—as optometrists—likely encounter daily.1 When educating patients on their diagnosis and logistics of cataract surgery, patients can become easily overwhelmed, and that’s before even mentioning they have multiple intraocular lens (IOL) options. If cost is no object, when presented with the option of wearing glasses postoperatively vs. being glasses-free (or at least less dependent on them), most patients pick the latter. Luckily, improvements in IOL technology are helping us to deliver on that desire.
Along with keratometry and biometry measurements, a carefully executed, complete eye exam is an important step that can guide a physician in recommending a particular lens. Starting the conversation with patients begins by knowing how regular their ocular surface is, and whether there are conditions present that can impact post-op visual acuity and patient satisfaction.
Here, I’ll offer my perspective on five of the newest IOLs available today: Alcon AcrySof IQ PanOptix Trifocal IOL, Johnson & Johnson Vision Tecnis Synergy IOL, Alcon AcrySof IQ Vivity Extended Vision IOL, Johnson & Johnson Tecnis Eyhance IOL and the Light Adjustable Lens made by RxSight. These are my anecdotal impressions based on our patient base.
PanOptix
 |
| PanOptix and PanOptix Toric IOL. Click image to enlarge. |
PanOptix was the first trifocal IOL and FDA-approved in 2019; it can correct 1.03D to 2.57D of corneal astigmatism.2 It is designed to allow for clear distance, intermediate and near-vision. The manufacturer says optics behind the lens involve diffractive rings imprinted on the surface that bend and split light to allow all ranges of vision.3 The rings cause side effects such as glare and halos, which can be a problem while driving at night due to oncoming headlights and stoplights. Postoperative visual acuity is generally in the range of 20/20 to 20/25 while measuring the eyes independently, 20/20 with both eyes at distance and J1-J1+ at near.
Although patients can function without glasses, when one eye is working to see distance, intermediate and near the quality of the vision may be marginally worse than with a monofocal lens at whatever target it was intended to correct. Habitual hyperopes and high myopes are generally ecstatic with the quality of their near-vision, but myopes who were -2.00 D to -4.00 D preoperatively need to be educated that they will lose their “superpower near.”
In my experience, naturally near-sighted patients are still happy with the PanOptix lens, but more often than not they comment that they could see slightly clearer without their glasses preoperatively.
Although near acuity is great in the right environment, the PanOptix lens struggles in dim environments and/or when reading small, fine print. An example I give to patients is while reading a menu at a nice but dim restaurant, they may need to use a low-powered pair of readers. If patients are receptive to these sacrifices for a large degree of glasses independence, the PanOptix IOL is a fantastic option.
The aforementioned glare and halos are a side effect that, if not discussed preoperatively, has the potential to create an unhappy patient post-operatively. Most patients mention the dysphotopsias in the interim between their two surgeries. Once the lens is implanted in both eyes, the brain tends to adapt to the change over time and few patients mention them past one-month post-op. The ones who do notice them long-term are generally so happy with the quality of their uncorrected vision that the glare and halos are a sacrifice they’re willing to make.
If the patient is still happy with the idea of the PanOptix IOL after mentioning the expected vision and side effects, the rest of their ocular health needs to be essentially pristine with regular topography and normal macular and optic nerve OCT scans. Unfortunately, patients with history of LASIK, photorefractive keratectomy (PRK), radial keratotomy (RK) and any other refractive surgeries are also not great candidates for the PanOptix IOL. Every case is different, but typically once the cornea has been permanently altered, it makes choosing the power of the IOL more difficult and acuity more unpredictable. The Optiwave Refractive Analysis system (ORA) is a tool to improve postoperative results by measuring the refractive power of the eye in its aphakic state. The ORA can reduce the unpredictability of picking the lens power; however, I still err on the side of caution in recommending the PanOptix to patients with history of refractive surgery.
About 80% of every cataract evaluation I see also has some form of dry eye disease. It is imperative to treat dry eye prior to surgery to ensure the most accurate keratometry and biometry measurements. I typically keep patients on therapy for four to six weeks, then have them return to repeat measurements before the final lens is picked for surgery, ensuring the best outcomes. Depending on the patient and the degree of dry eye, I either recommend autologous serum tears or Restasis (cyclosporine A ophthalmic emulsion 0.05%, Allergan)/ Xiidra (lifitegrast ophthalmic solution 5%, Novartis) in combination with a steroid.
Even if a patient seems like the perfect PanOptix candidate on paper, it’s important to ensure they have realistic expectations. Those who demand high-quality distance vision, such as pilots, truck drivers and engineers, should steer clear of a trifocal lens due to the side effects. Patients who seem hesitant about the glare and halos should also select a different IOL because they will be more sensitive to being bothered postoperatively.
Although there are situations when the PanOptix is not the best choice, it is still the first premium lens I recommend to patients who are the right candidates. The “wow” factor at the day one postoperative visit and the quality of the vision are hard to question.
Synergy
 |
| The Synergy IOL can correct 1.03D to 2.57D of corneal astigmatism. Click image to enlarge. |
The Tecnis Synergy IOL was FDA-approved in April of 2021 and is the newest IOL from Johnson & Johnson Vision that incorporates technology of its family members, the Tecnis Multifocal and the Tecnis Symfony, that the manufacturers says will allow for improved near visual acuity and less nighttime glare and halos.4 The Toric Synergy lenses can correct 1.03D to 2.57D of corneal astigmatism. According to the company, the Synergy allows for the widest range of continuous vision with best near, continuous vision defined as a visual acuity of 20/32 or better.5
In practice, I find postoperative acuity to be similar to what the company states and competitive with that of the PanOptix lens. I’ve found the improved near visual acuity is a benefit to the -2.00D to -4.00D myopes who may be disappointed with the quality of near vision with the PanOptix.
The Synergy’s older sister, the Symfony, had a problem with nighttime photopic phenomena, including “spiderweb” effects that made it difficult to drive at night. The Synergy lens is said to have mitigated this effect from the combination of the echelette surface design and “achromatic technology,” which are said to reduce the intensity and incidence of glare and halos.5
Although my sample size is small because the IOL is so new, around half the patients I’ve seen have mentioned trouble driving at night even after the one-month post-op visit. However, most who had complaints were not good candidates for the Synergy due to mild refractive amblyopia, untreated dry eye or similar concerns. As previously mentioned, picking an ideal candidate for a multifocal lens is important for post-op success. Although I’ve had more experience with the PanOptix, I’m looking forward to managing more Synergy patients in the future.
Vivity
 |
| Vivity Toric IOL is the first non-diffractive extended depth of focus (EDOF) lens. Click image to enlarge. |
Alcon’s Vivity IOL was FDA approved in 2020 and is the first non-diffractive extended depth-of-focus (EDOF) lens. Vivity Toric IOLs can correct between 1.03D to 2.06D of corneal astigmatism.6 The extended vision comes from a design feature Alcon calls “X-Wave technology,” which adds a one micron elevated smooth plateau centrally that behaves like a monofocal lens.6 The non-diffractive nature of the lens greatly diminishes the incidence of nighttime photopic phenomena of the PanOptix and Synergy lens, with the sacrifice of less near visual acuity. Uncorrected distance visual acuity is comparable to that of a monofocal distance lens, intermediate acuity is 20/20 to 20/25, but the J1 acuity expected out of a PanOptix or Synergy, is J4-J5 with the Vivity.
Although the near acuity isn’t as impressive, the Vivity serves patients with a high-distance demand, such as truck drivers and hunters, extremely well due to the clarity of vision at distance and minimal glare and halos. On the other hand, patients who read often or work with numbers need to be educated that reading glasses will likely be required for those tasks.
Where the Vivity lens truly shines is in the presence of mild ocular disease and patients with history of refractive surgery. Given the absence of diffractive rings that split light, this lens is more forgiving for conditions such as mild glaucoma with a non-central visual field defect, mild dry age-related macular degeneration and mild Fuchs’ endothelial dystrophy. Because the Vivity has similar optics to a monofocal lens, most every patient who is a candidate for a monofocal is also a candidate for the Vivity.
In my experience, patients have been extremely happy with the range that the Vivity allows. The positive feedback has influenced me to recommend it to any patient who is not a candidate for a trifocal lens as long as they are counseled appropriately.
Eyhance
Johnson & Johnson’s Eyhance was FDA approved in February 2021; it is a monofocal lens designed to slightly extend depth of focus compared with the Tecnis monofocal ZCB00.7 Eyhance Toric IOLs can correct between 1.03D to 4.11D of corneal astigmatism, according to J&J.7 The lens is designed with an aspheric anterior surface that creates a continuous increase in power within the central 1mm diameter. Distance vision is equivalent to a monofocal lens, but patients can appreciate an increase in intermediate vision.
A study comparing the Eyhance to the Symfony found uncorrected monocular and binocular distance vision and binocular intermediate vision to be the same between the two.8 The Symfony lens had improved uncorrected near vision, but also had more incidence of halos and glare.8
Eyhance would benefit patients who cannot afford an EDOF lens, especially those that have high intermediate vision demands.
Light Adjustable Lens
RxSight’s Light Adjustable Lens (LAL) was FDA approved in 2017 and is the only IOL that can be adjusted after cataract surgery to optimize uncorrected visual acuity.9 Because it is a monofocal, all astigmatism and any residual spherical correction is treated postoperatively. The lens is composed of ultraviolet (UV) light–sensitive polymers that the manufacturer says migrate when exposed to UV, changing the shape of the lens and allowing physicians to treat myopia, hyperopia and astigmatism.9
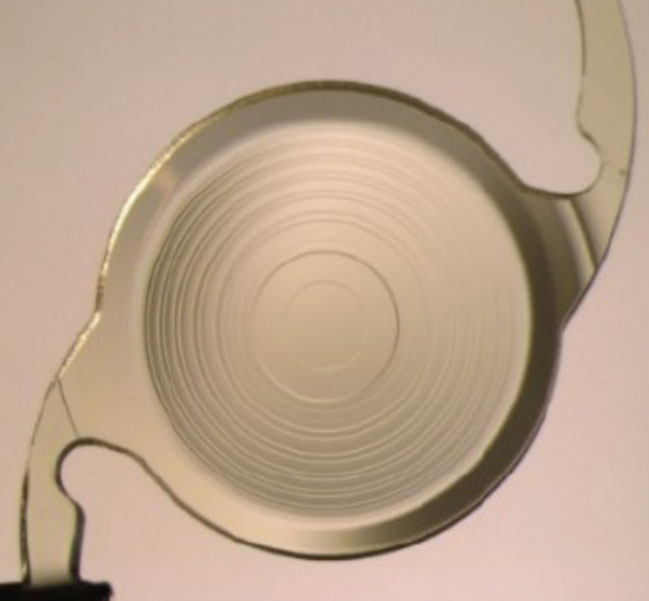
 |
| RxSight’s Light Adjustable Lens (LAL) is composed of UV light–sensitive polymers. An advantage to LALs is that ODs have the ability to adjust the lens postoperatively. Click image to enlarge. |
The company’s Light Delivery Device (LDD) is used to deliver the treatment, the first adjustment generally occurring two to three weeks after cataract surgery, with each subsequent adjustment occurring in three-day increments. Between three to five treatments can be made, each lasting 40 to 120 seconds. For the lens to maintain its shape between adjustments, patients must wear UV-blocking glasses while indoors and sunglasses while outdoors during all waking hours. Optometrists are able to handle this step.
With each LDD adjustment, physicians can treat -2.00D to +2.00D sphere and up to 2.00D of astigmatism. Once desired refraction is achieved, the patient will receive either one or two lock in treatments, in which the UV-sensitive macromers will be used to prevent refractive changes in the future.9
The biggest advantage to the LAL is spelled out in its name: the ability to adjust the lens. Practitioners who have trouble measuring consistent keratometry and biometry readings in patients who have had refractive surgery, especially RK, can pick the IOL power with more peace of mind knowing it can be adjusted. If a patient is not a candidate for an EDOF or multifocal implant, the LAL—although a monofocal—can help give patients some degree of spectacle independence through a monovision approach.
I hesitate to set a patient’s target to monovision if they have not had success in the past with contact lenses due to problems with adaptation. The ability to adjust the prescription makes it easier to ease a patient into monovision and gives us the opportunity to switch back to a distance or near target with poor adaptation. In my experience, most patients tolerate monovision and end up somewhere around 20/20 and J1 at distance and near, respectively.
Because the IOL is susceptible to UV light, patients must wear UV-blocking glasses full-time indoors and outdoors until their prescription is locked in. If patients are not compliant with the glasses, the polymers in the lens can move and make the subsequent light adjustments more difficult to achieve. This can lead to poor uncorrected visual acuity. So, if patients are hesitant about the glasses, it may be more beneficial to steer them toward a different option.
Patients must also be aware that their visual acuity prior to any treatments will be limited by their uncorrected astigmatism. If a patient requires excellent visual acuity within one-week post-op for whatever reason, the LAL is not the best option.
Although many are candidates for the LAL, there are several situations in which a candidate is not eligible to receive it. Patients taking systemic medications that can increase sensitivity to UV light such as tetracyclines, amiodarone, hydrochlorothiazide are not candidates for the LAL due to potential phototoxic effects to the eye.9 Similarly, patients taking medication that can be toxic to the retina, such as tamoxifen, are at risk for retinal damage during light treatments. Those with a history of ocular herpes simplex virus are at risk of reactivation from UV light exposure, and patients with nystagmus may not be able to fixate during treatments which can lead to poor uncorrected visual acuity.
Due to the amount of follow-up appointments and necessity for UV-blocking glasses full-time in the postoperative period, I recommend the LAL most often to patients who have had RK. As previously mentioned, their amount of astigmatism is unpredictable. Through use of the LDD, data shows only 1.3% of patients are left with uncorrected visual acuity of 20/32 or worse, compared to 10.9% with the Tecnis toric and 16.6% with the AcrySof toric.10-12 Time spent in office with adjustments can be a burden to the patient as well.
I must carefully refract the patient and, if trialing monovision, ensure they are happy with their vision with a trial frame. After the patient and I are happy with the target, the pupils must be dilated to 7mm to receive full treatment, which can sometimes take two or three doses of mydriatic drops. Although the time in front of the LDD is only minutes, on a busy clinic day the patient can be in the office for up to three hours. If a patient is a candidate for any of the other options discussed, I have a hard time recommending the LAL due to the demanding post-op care.
Takeaways
With the advent of new IOLs, many cataract patients can live a life less dependent on glasses. As the practitioner who generally spends more time with patients, it is our responsibility to ensure they know what their options are and what lens you recommend for them based on their lifestyle, personality and needs. Communicating that information to the surgeon will help make the sometimes stressful process easier and faster.
As long as patients are educated appropriately and expectations are set up for what to expect before surgery, there is no reason to avoid recommending these lenses.
Dr. Rojas graduated cum laude from University of the Incarnate Word Rosenberg School of Optometry. She completed her residency in ocular disease and refractive surgery at Eye Center of Texas in Houston and practices at Slade & Baker Vision, a refractive and cataract surgery practice in Houston. She has no financial disclosures.
1. Causes of blindness and vision impairment in 2020 and trends over 30 years: evaluating the prevalence of avoidable blindness in relation to Vision 2020: the Right to Sight: an analysis for the Global Burden of Disease Study. Lancet Glob Health. 2021;99(2):e144-60. 2. Acrysof IQ PanOptix Trifocal and Toric Trifocal Intraocular Lens. U.S. Food and Drug Administration. www.fda.gov/medical-devices/recently-approved-devices/alcon-laboratories-inc-acrysofr-iq-panoptixr-trifocal-intraocular-lens-model-tfnt00-and-acrysofr-iq. September 19, 2019. Accessed November 30, 2021. 3. Sudhir RR, Dey A, Bhattacharrya S, Bahulayan A. AcrySof IQ PanOptix intraocular lens vs. extended depth of focus intraocular lens and trifocal intraocular lens: a clinical overview. Asia Pac J Ophthalmol (Phila). 2019;8(4):335-49. 4. Tecnis Synergy Intraocular Lenses– P980040/S124. U.S. Food and Drug Administration. www.fda.gov/medical-devices/recently-approved-devices/tecnis-synergytm-intraocular-lens-iol-model-zfr00v-tecnis-synergytm-toric-ii-iol-models-zfw150. Accessed November 30, 2021. 5. J&J Vision. Tecnis Synergy IOL. www.jnjvisionpro.com/synergy. Accessed November 30, 2021. 6. Alcon Vivity EDOF Lens starts its rollout in the United States. Rev Ophthalmol. www.reviewofophthalmology.com/article/alcon-vivity-edof-lens-starts-its-rollout-in-the-united-states. February 12 2021. Accessed November 30, 2021. 7. J&J Vision. Tecnis Eyhance IOL. www.jnjvisionpro.com/eyhance. Accessed November 30, 2021. 8. Corbelli E, Iuliano L, Bandello F, Fasce F. Comparative analysis of visual outcome with three intraocular lenses. J Cataract Refract Surg. May 26, 2021. [Epub ahead of print.] 9. RxSight. www.rxsight.com/us. Accessed November 30, 2021. 10. RxSight P160055: FDA Summary of Safety and Effectiveness Data. www.accessdata.fda.gov/cdrh_docs/pdf16/P160055B.pdf. Accessed November 30, 2021. 11. Tecnis Toric PMA P980040/S039: FDA Summary of Safety and Effectiveness Data. www.accessdata.fda.gov/cdrh_docs/pdf/P980040S039B.pdf. Accessed November 30, 2021. 12. AcrySof Toric P930014/S45: FDA Summary of Safety and Effectiveness Data. www.accessdata.fda.gov/cdrh_docs/pdf/P930014S045b.pdf. Accessed November 30, 2021. 13. Ajamian PC. Near and Far. Rev Optom. 2021;158(1):26. |

