Retinal Vascular Miniseries |
| Follow the links below to read the other installments in this miniseries: Part 2: Read the Retinal Vasculature Like a Pro Part 3: Imaging Motion: a Review of OCT-A Part 4: Identify and Manage Retinal Vascular Tumors |
The Retinal Vasculature: A Marker for Ocular, Neurologic and Systemic Disease
The retina is a unique and fascinating anatomical structure. It’s the only part of the central nervous system we can observe noninvasively, along with its associated retinal, systemic and cerebrovascular pathologies. Viewed through direct ophthalmoscopy, indirect ophthalmoscopy, indirect biomicroscopic ophthalmoscopy, ocular photography, fundus autofluorescence, optical coherence tomography (OCT), fluorescein angiography or OCT angiography, qualitative and quantitative retinal observations can reveal unfolding, worsening or impending retinal, systemic, neurologic or cerebrovascular disease.
Multiple studies demonstrate associations between newly forming and chronic retinal and cerebral vascular disease. Observable changes in retinal vascular architecture, such as increased retinal vein caliber (decreased artery-to-vein ratio), retinal vascular tortuosity, increased prominence of the retinal arterial reflex, venous nicking, “copper” or “silver wire” appearance as well as the discovery of cholesterol, calcium or thrombotic emboli are all associated with concurrent and future cerebrovascular events. These associations support the use of the retinal vasculature as a biomarker for discovering, predicting or monitoring patients for potential retinal, systemic, neurological and cerebral vascular morbidities and risks—essentially broadening the responsibilities of the optometrist.
This four-part series introduces some of the root concepts of the neuro-retinal-systemic connection, along with some normal and abnormal retinal vascular phenomena. I thank each of the author teams. Without their expertise and willingness to participate, this miniseries would not have been possible. I hope this educational experience becomes a useful resource for you in clinical practice.
—Andrew S. Gurwood, OD, Clinical Editor, retinal vascular miniseries
When performing fundus evaluations, you may be tempted to focus on the retina and optic nerve while overlooking the status of the retinal vessels. However, the retinal venules and arterioles can provide vital diagnostic information. The eye allows for direct, noninvasive visualization of the body’s microvasculature (giving insight into the patient’s overall vascular health). The retinal vessels should be studied during clinical examination. Changes in the shape, color and caliber of vessels can represent ocular manifestations of many systemic conditions. Examining the arteriolar-venular caliber ratio can assist in diagnosing vascular abnormalities and associated pathology. A reduced ratio could indicate retinal venular dilation, arteriolar attenuation or both.
Fundus photography can help monitor any changes in retinal vasculature and retinopathy. Using it, you can obtain a side-by-side comparison of the retinal vasculature in each eye—a valuable indicator of worsening or resolving pathology.
Identifying anomalous vasculature, coupled with understanding the fundamental causes of pathological changes, can be crucial for identifying systemic conditions.
Here, we address the pathophysiology and commonly associated conditions that occur when patients present with abnormal vasculature, such as dilated, tortuous retinal veins; dilated nontortuous retinal veins; dilated retinal arteries; tortuous retinal arteries; and narrowed retinal arteries.
 |
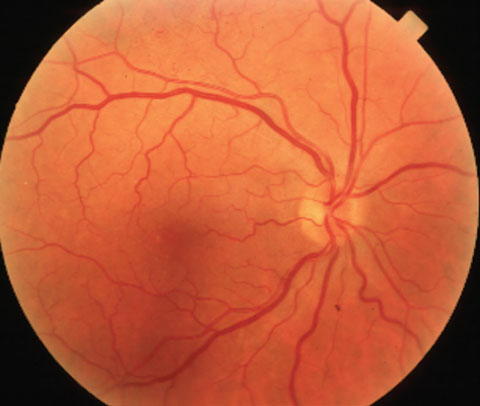
| Dilated, tortuous retinal veins in an impending vein occlusion. Click to enlarge. |
Dilated, Tortuous Retinal Veins
Vascular occlusion is the second most common cause of blindness due to retinal disease, following diabetes.1 The retinal venules typically present as both dilated and tortuous preceding and during a vascular occlusive event. Virchow’s triad—a term used to describe various etiologies of thrombosis—consists of hemodynamic changes (blood stasis), degenerative and mechanical changes to the vessel wall, and blood hypercoagulability.1,2 If you observe dilated, tortuous retinal venules, consider impending retinal vein occlusion. This condition occurs when a thrombosis exists within the venous circulation causing outflow obstruction within the retina. The thrombosis will cause a buildup of pressure within the venous and capillary system and can potentially cause the leakage of blood or serosanguinous fluid, or both, into the retina. Vision may be lost if leakage occurs in or near the macula, causing secondary edema or ischemia via capillary closure. Possible etiologies include: diabetes, hypertension, cardiovascular disease, hyperviscosity syndromes (anemia and antiphopspholipid antibody state), arteriosclerosis, carotid artery disease, collagen vascular disease and coagulopathies (sickle cell disease).
While typical patients who present with a central retinal vein occlusion (CRVO) include middle-aged individuals with a strong systemic history of hypertension, hypercholesterolemia or diabetes, atypical presentations may warrant referrals to rule out hypercoaguable diseases.1,2 A 25-year-old female presenting with a CRVO without any known vascular diseases would warrant evaluation for autoimmune factors, blood dyscrasia or dysproteinemia. First, rule out specific drugs that have the potential to cause retinal vascular occlusions. Diuretics, oral contraceptives and antipsychotics have all been linked to retinal vascular occlusions and should be considered in these cases.3
 | 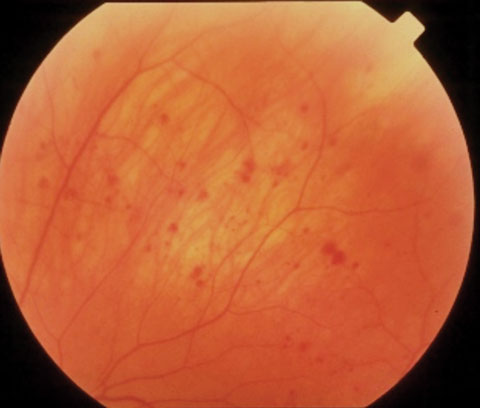 |
| At left, dilated, nontortuous retinal veins in a patient with blood dyscrasia. At right, midperipheral hemorrhages and dilated retinal veins in ocular ischemic syndrome. | |
Identifying the underlying systemic cause of this condition allows for early management and prevention of other harmful sequelae. Many causes of retinal vein occlusion have the potential to threaten systemic circulation and ultimately harm other organs in the body if not identified and treated early.
Venous beading is an ocular sign that connotes the shape and appearance of retinal venules. It is commonly associated with poorly controlled diabetes. This phenomenon is a strong predictor of progression to neovascular, or proliferative, diabetic retinopathy.2 The beaded appearance of the venule is caused by prolonged cycles of hypoxia with constant dilation and constriction of the lumen due to vascular autoregulation.4 Recognizing this beaded appearance during clinical examination should prompt a referral to a primary care physician or endocrinologist. Proper referral and management may prevent vision loss by preventing systemic worsening and debilitating retinopathy.
Many studies have reported an association between larger retinal venous caliber and increased risk for cardiovascular disease.5 Data from the Atherosclerosis Risk in Communities (ARIC) study shows that narrowed arterioles, dilated venules or both are associated with risk of incident stroke events and coronary heart disease events.5 Retinal venular dilation is hypothesized to reflect the effects of hypoxia, inflammation and endothelial dysfunction.5
Categories of Vasculature Abnormalities | |
| Dilated, tortuous retinal venules | Retinal vascular occlusion caused by: • Diabetes • Hypertension • Cardiovascular disease • Hyperviscosity states • Arteriosclerosis • Collagen vascular disease • Sickle cell disease |
| Dilated, non-tortuous retinal venules | Ocular ischemic syndrome caused by: • Atherosclerosis • Dissecting aneurysm of the carotid artery • Giant cell arteritis • Fibrovascular dysplasia • Takayasu arteritis • Aortic arch syndrome • Behçet’s disease • Trauma or inflammation causing stenosis of the carotid arteries |
| Dilated retinal arterioles | Retinal arteriolar macroaneurysm |
| Tortuous retinal arterioles | Possible association with systemic vascular diseases |
| Narrowed retinal arterioles | Hypertension, atherosclerosis, retinal artery occlusion |
Consider systemic signs if you suspect cardiovascular disease—shortness of breath, fatigue, irregular heartbeat, pain in chest area or dizziness.6 If you identify venular dilation in conjunction with other ocular or systemic signs of cardiovascular disease, recommend a cardiovascular workup in comanagement with the patient’s primary care provider or cardiologist.
In addition, you may see a few uncommon causes of retinal vein occlusions. One such cause is retinal arteriovenous malformations (Wyburn-Mason syndrome), a rare retinal anomaly in which abnormal blood flow occurs between retinal arterioles and venules, bypassing the capillary bed. This condition is usually congenital and typically presents as a unilateral, dilated and tortuous vascular loop.7 Retinal malformation can be a presenting sign of simultaneous systemic malformations that occur in the brain.7
 |
 |
| Above, arteriolosclerosis and venous compression in hypertension. Below, arterial attenuation and arteriovenous nicking in hypertension. Click images to enlarge. |
Dilated Nontortuous Retinal Veins
Degenerative changes to the vessel wall can occur secondary to chronic hypertension and atherosclerosis. Blood hypercoagulability can occur due to a blood dyscrasia, dysproteinemia and sickle cell disease, as well as other diseases that cause a hypercoagulable state.8
Ocular ischemic syndrome (OIS) is caused by decreased blood flow to the ocular blood vessels, which is due to stenosis or occlusion of the common or internal carotid arteries.9 The decreased blood flow from the retinal arterioles to the capillaries causes a significant decrease in vascular pressure and secondary venous stasis.9 In OIS the retinal venules are typically dilated but not tortuous.9
Other nonatheromatous causes of OIS include: dissecting aneurysm of the carotid artery, fibrovascular dysplasia, Takayasu arteritis, aortic arch syndrome, Behçet’s disease, giant cell arteritis, trauma or inflammation causing carotid artery stenosis.9
Ocular hypoperfusion leads to clinical signs of dilated retinal venules as well as unilateral hemorrhages in the mid-periphery of the retina.9 In addition, OIS patients will usually present with a plethora of anterior segment-related findings—uveitis, hypotony, neovascularization, corneal edema and cataract.9 Considering the high risk of cardiovascular disease, it is imperative to quickly refer these patients for a full cardiovascular work-up, paying particular attention to the ipsilateral common or internal carotid artery.9 Clinically, we can evaluate the carotid arteries by auscultation using the bell side of a stethoscope and listening for a bruit—a sound signifying turbulent blood flow due to plaque buildup of the carotid artery. However, a bruit will not be heard if the carotid artery is significantly stenosed.10
A similar pathophysiology occurs in patients who suffer from a blood dyscrasia or dysproteinemia. Changes in blood composition can lead to a disturbance in blood flow causing potential thrombus formation and vessel occlusion. Blood dyscrasias can present as dilated nontortuous retinal veins with or without retinal hemorrhages.3
Dilated Retinal Arteries
The retinal arterioles may also present as dilated, tortuous or narrowed. Retinal arteriole macroaneurysms (RAM), for instance, present as focal dilations in retinal arterioles and are usually caused by systemic hypertension.11 This condition usually presents within the first three bifurcations in the retina and may be difficult to detect during clinical examination if significant retinopathy exists.11
Hemorrhage, exudates and edema all have the potential to affect vision, especially if the lesion is in proximity to the fovea. The lesions tend to occur unilaterally in female patients older than 60 years.11 Fundus photography, OCT and optical coherence tomography angiography (OCT-A) are ancillary tests that could be useful in imaging the retinal microvasculature documenting RAM location. Prompt evaluation with a retinal specialist is adequate if macular edema or significant retinopathy exists.
Consider a referral to a specialist for a full work-up for hypertension, lipid evaluation and a full systemic vasculitis work-up.12
Tortuous Retinal Arteries
The significance of tortuous retinal arterioles has been hotly debated in the literature for decades. While some studies suggest that tortuosity may be strongly associated with systemic vascular conditions, others have disproved this theory and have found no apparent correlation.13 One study concluded that older age, higher blood pressure, alcohol consumption, greater BMI, diabetes and higher HbA1c level are significantly associated with less tortuous arterioles.13 A smaller study of 218 healthy young Caucasians associates straighter retinal arterioles with higher blood pressure and BMI.13 Conversely, two small clinic-based studies associate elevated blood pressure with increased retinal arteriolar tortuosity. Therefore, additional larger population-based studies are needed to further evaluate the relationship between arteriolar tortuosity and vascular diseases.
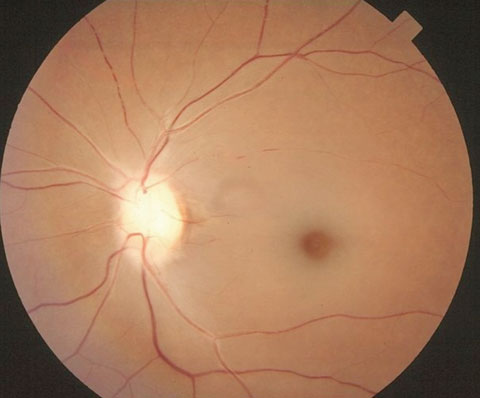 |
| Narrowed, attenuated retinal arterioles in retinal artery occlusion. Click images to enlarge. |
Narrowed Retinal Arteries
Narrowed retinal arteries can occur secondary to atherosclerosis, hypertension or both.14 Chronic hypertension has the potential to cause many types of ocular findings, including: arteriolar attenuation, arteriole-venule nicking, cotton wool spots, hemorrhage, maculopathy, and optic nerve edema if severe.14 Retinal arteriolar attenuation is a defining sign of hypertensive retinopathy.14 The finding is considered an autoregulatory, physiological response to retinal artery vasospasm.14
Chronically elevated blood pressure can cause irreversible arteriolar narrowing and hardening of the arteriolar wall, with an apparent broadening of the arterial light reflex.14 “Copper” and “silver wiring” are exaggerated forms occurring secondary to increased optical density of the vessel.
The major anatomical difference between retinal arterioles and venules are that arterioles have thicker vessel walls capable of compressing and reducing blood flow through the underlying venule. The sclerotic changes in vessel wall structure from chronic hypertension may have the potential to indent the underlying venule when crossing over it in the retina.14 This crossing change, known as arteriovenous nicking, can change the hemodynamics within the venule. This condition should be watched closely and managed cautiously, as patients are at increased risk for thrombus formation and secondary branch retinal occlusion. Managing them with periodic evaluation as well as comanaging systemic risk factors with a primary care provider or cardiologist is crucial to prevent future manifestations of the disease.
Retinal artery occlusion is an important consideration when a patient presents with narrowed retinal arteries. These occlusions are commonly caused by emboli, thrombi, trauma or inflammation causing a blockage within the retinal arteriole. Recognizing arteriolar attenuation, in conjunction with other signs of a retinal artery occlusion (pallid edema of the retina, correlating visual field or visual acuity loss, presence of an afferent pupil defect) supports the diagnosis. Fundus photography can aid in side-by-side retinal comparison and identification of reduced retinal perfusion and arteriole attenuation. OCT-A can image the abnormal blood flow through the arteriole system.
Retinal artery occlusion is a significant indicator of systemic disease.15 All acute cases of retinal artery occlusion warrant immediate referral to a stroke unit for evaluation. It is essential to suspect certain cases of retinal artery occlusions may be caused by giant cell arteritis. Should suspicion be high, immediate evaluation with erythrocyte sedimentation rate and c-reactive protein is required as 5% to 10% of all central retinal artery occlusions are caused by giant cell arteritis.15
Atherosclerosis is caused by the hardening of the vessel wall due to the build-up of fatty plaque, causing a reduced arteriole lumen size. The Blue Mountains Eye Study and the Beaver Dam Eye Study revealed smaller arterioles and larger venules were associated with a 20% to 30% increased risk of coronary heart disease (CHD) mortality independent of cardiovascular risk factors.16 Another study showed that women with larger retinal venules or narrower arterioles each had a 30% higher risk of CHD, even after adjusting for other known cardiovascular risk factors.16
Understanding the various conditions that may change the appearance of the retinal vasculature will allow for early management and possible prevention of sight-threatening sequelae. Aside from direct clinical examination, the newly developed OCT-A may prove to be a useful, noninvasive imaging technique of the retinal microvasculature. OCT-A is capable of direct, high resolution imaging of blood flow using the motion from red blood cells within the vessel. Using advanced imaging modalities such as fundus photography and OCT-A will allow for monitoring and detection of vascular changes over time. The status of the retinal vessels can provide much information about our patients’ systemic health. The retinal vascular system has a story to tell if you are willing to listen.
Dr. Rousso is a faculty member at Nova Southeastern University’s College of Optometry.
Dr. Sowka is chief of advanced care and director of the glaucoma service at Nova Southeastern University College of Optometry.
|
1. Kolar P. Risk factors for central and branch retinal vein occlusion: A meta-analysis of published clinical data. J Ophthalmol. 2014;2014(4):724-80. 2. Kumar D, Hanlin E, Glurich I, et al. Virchow’s contribution to the understanding of thrombosis and cellular biology. Clin Med Res. 2010 Dec;8(3-4):168-72. 3. Citirik M, Haznedaroglu I. Clinical risk factors underlying the occurrence of retinal vein occlusion. International Journal of Ophthalmic Research. 2016;2(1):91-5. 4. Harrison W, Yevseyenkov V. Early interventions to prevent retinal vasculopathy in diabetes: a review. Clinical Optometry. 2015;7:71-80. 5. Wong T, Kamineni A, Klein R, et al. Quantitative retinal venular caliber and risk of cardiovascular disease in older persons. Arch Intern Med. 2006;21:2388-94. 6. Stern S, Behar S, Gottlieb S. Aging and diseases of the heart. Circulation. 2003;108:99-101. 7. Reck S, Zachs D, Eibschitz-Tsimhoni M. Retinal and intracranial arteriovenous malformations: Wyburn-Mason syndrome. Journal of Neuro-Ophthalmology. 2005;25(3):205-8. 8. Bonanomi M, Lavezzo M. Sickle cell retinopathy: diagnosis and treatment. Arq Bras Oftalmol. 2013;76(5):320-7. 9. Terelak-Borys B, Skonieczna K, Grabska-Liberek I. Ocular ischemic syndrome—a systematic review. Med Sci Monit. 2012;8:RA138-44. 10. Ratchford E, Jin Z, Tullio M, et al. Carotid bruit for detection of hemodynamically significant carotid stenosis: the Northern Manhattan Study. Neurol Res. 2009;31(7):748-52. 11. Speilburg A. Ruptured retinal arterial macroaneurysm: Diagnosis and management. J Optom. 2014;7:131-7. 12. Birkholz E, Johnson T, Russell S. Retinal artery macroaneurysm (RAMA). Eyerounds.org. 2010. Available at http://webeye.ophth.uiowa.edu/eyeforum/cases/113-RAMA.pdf. Accessed December 13, 2016. 13. Cheung C, Zheng Y, Hsu W, et al. Retinal vascular tortuosity, blood pressure and cardiovascular risk factors. J Ophthalmol. 2011:118(5):812-18. 14. Bhargava M, Wong T. Current concepts in hypertensive retinopathy. Retinal Physician. 2013;10:43-54. 15. Varma D, Cugati C, Chen S. A review of central retinal artery occlusion: clinical presentation and management. Eye. 2013;27:688-97. 16. Ikram M, Ong T, Cheung C. Retinal vascular caliber measurements: clinical significance, current knowledge and future perspectives. Ophthalmologica. 2013;229:125-36. |

