 |
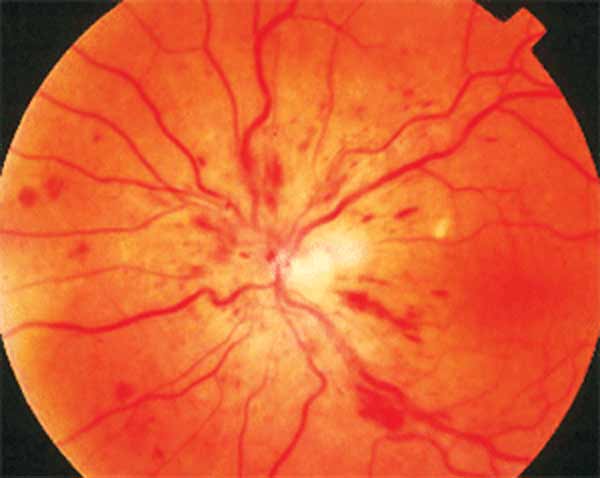
In the study, patients experiencing CRVO (seen here) with good VA didn’t respond to anti-VEGF treatment, although those with BRVO did. Photo: Joseph W. Sowka, OD. Click image to enlarge. |
The first-line therapy for macular edema due to retinal vein occlusion (RVO) is intravitreal anti-VEGF injections, but it’s unclear whether those with good visual acuity at diagnosis should begin immediately or remain closely monitored. To paint a more complete picture of the appropriate treatment protocol, researchers recently analyzed the visual and anatomical outcomes from anti-VEGF treatment among RVO patients with good vision at baseline, defined here as BCVA ≥20/32.
A total of 131 eyes of patients diagnosed with macular edema secondary to RVO were evaluated. Three groups were compared based on management approach: no anti-VEGF treatment, delayed anti-VEGF and immediate anti-VEGF. Central subfield thickness (CST) and best-corrected visual acuity (BCVA) were collected at diagnosis and six, 12 and 24 months of follow-up.
Among the three groups, there was no significant difference in average visual acuity after 24 months. The number of patients with good vision (BCVA ≥20/25 and ≥20/40) after 24 months also did not differ. While some patients in the delayed treatment group lost at least one line of vision after 24 months, there was no significant difference in CST changes of at least 10%.
For RVO patients with good vision at baseline, average visual acuity at all follow-up visits was similar regardless of initiation and timing of anti-VEGF treatment.
“While some patients who delayed anti-VEGF treatment for more than 30 days after diagnosis lost at least one line of vision over 24 months, these patients also had a higher average BCVA at diagnosis, potentially explaining the greater change in vision over time,” the authors suggested in their paper on the study for the journal Eye. “Moreover, patients who did not receive anti-VEGF treatment after diagnosis started at a lower average BCVA at diagnosis and experienced little change over time.”
Vision and retinal anatomy changed according to different treatment parameters for some patients. “While delaying anti-VEGF treatment for some patients correlated with lines of vision lost, this did not affect retinal thickness changes of at least 10%,” the authors wrote. “In fact, patients who experienced on average the greatest change in CST were those who did not receive any anti-VEGF treatment at all.
The authors went on to say this isn’t uncommon, as previous studies have found little correlation between BCVA and CST.
Lastly, it should be noted that central RVO patients didn’t respond to immediate anti-VEGF treatment, but branch RVO patients did. They had a significantly decreased retinal thickness at 24 months and were less likely to lose lines of vision with immediate anti-VEGF treatment.
“This study suggests that while some patients who delay anti-VEGF treatment can experience vision loss, overall visual acuity over two years is comparable between patients who receive immediate, delayed or no anti-VEGF treatment,” the authors concluded in their paper. “Close observation with initiation of treatment when appropriate may be recommended in the setting of routine clinical practice for RVO patients with good vision at diagnosis.”
Liu JC, Vatti T, Seth K, et al. Outcomes in patients with retinal vein occlusion with good baseline visual acuity. Eye. March 2, 2023. [Epub ahead of print]. |

