 |
A 64-year-old Hispanic male presented with complaints of dryness and blurred vision in both eyes. He was vacationing in Europe a month earlier and noted difficulties focusing and seeing clearly.
His ocular history is significant for having had cataracts extracted from both eyes 10 years earlier with excellent visual outcomes.
He also reported being told that he has keratoconus, but that had not caused any issues beyond needing glasses. His last eye exam was approximately 18 months earlier.
His past medical history is significant for lung cancer, which was diagnosed approximately two years earlier, and hypertension, which was well controlled. He had been on a chemotherapy medication, but that had been discontinued approximately three months prior due to being put on a study medication for the lung cancer.
On examination, his entering acuities measured 20/30 in each eye; however, he was easily refracted to 20/20. Confrontation visual fields were full to careful finger counting in both eyes. His pupils were equally round and 3+ reactive with no afferent pupillary defect. The anterior segment was significant for 1+ punctate epithelial erosions in both eyes and well-positioned posterior chamber intraocular lenses (IOLs). A dilated fundus exam showed small cups with good rim coloration and perfusion in both eyes. In the right eye, there were changes temporal to the macula (Figure 1). An SD-OCT was also performed (Figure 2). The left eye was completely normal.
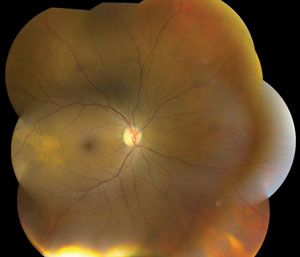 | |
| Fig. 1. Montage image of the right eye of our patient—what do you see? |
Take the Retina Quiz
1. What does the SD-OCT show?
a. It’s normal.
b. Irregularity of the RPE.
c. A PED temporal to the macula.
d. A choroidal mass.
2. What additional testing would be helpful in establishing a diagnosis?
a. Visual field.
b. Fluorescein angiography.
c. Standardized ultrasound.
d. Fine-needle biopsy.
3. What is the correct diagnosis?
a. Amelanotic choroidal melanoma.
b. Amelanotic choroidal nevus.
c. Idiopathic central serous chorioretinopathy.
d. Metastatic carcinoma to the choroid.
4. How should this patient best be managed?
a. Observation only.
b. Refer the patient to an oncologist.
c. Anti-VEGF injection.
d. Plaque radiotherapy.
For answers, see below.
Diagnosis
Upon clinical exam of the right eye, we observed a poorly circumscribed, creamy yellow lesion that appeared slightly elevated. In addition, near the ora serrata inferior nasally at 5 o’clock, we observed another creamy yellow lesion that also appeared depigmented. The latter lesion appeared flat.
The SD-OCT through the lesion near the macula confirmed the subtle elevation that was seen on clinical exam. What is particularly interesting is the contour of the RPE in that area, which is being bowed, or pushed, anteriorly. This is due to a mass within the choroid that was pushing forward and causing a dome-shaped elevation. Given our patient’s history of having lung cancer, and the multiple cream-colored lesions, we felt certain this represented choroidal metastasis.
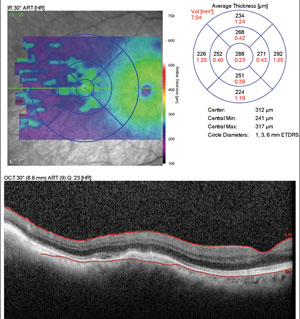 | |
| Fig. 2. This is the patient’s SD-OCT image temporal to the macula. |
Standardized echography was performed, which showed a 1mm thick choroidal mass measuring 10mm x 7.5mm. The internal reflectivity showed moderate reflectivity, which was consistent with choroidal metastasis.
Choroidal metastasis is the most common malignant tumor of the eye with a reported incidence of 2% to 9%, with the majority of the cases being due to breast cancer in women, followed by lung cancer in males.1 The choroid is one of the principal sites for development of metastasis in the eye due to its abundant arterial supply and favorable microenvironment for ‘‘seeding’’ of the cancer cells.2
The vast majority of patients who develop metastasis of the eye will have a known site of the primary tumor at the time of diagnosis. But that is not always the case. In some instances, the discovery of metastasis in the eye may be the presenting sign of cancer. In one report of 420 patients with choroidal metastasis, 34% had no history of cancer at the time of diagnosis. The tumors were unilateral in 76% of patients, and multiple lesions were seen in 20% of eyes, with a mean number of two lesions.3
Our patient already had a confirmed diagnosis of lung cancer, so it was not difficult to make the connection between the findings in his eye and his lung cancer.
The clinical features of choroidal metastasis are that of an ill-defined creamy-yellow lesion at the level of the choroid. There may be multiple lesions and, as indicated, they may be bilateral.
Depending on size and extent, non-rhegmatogenous retinal detachment may be present. A metastatic lesion arising from skin melanoma may be darker in color, and a lesion developing from renal cell carcinoma may appear reddish-orange in color.
Once a diagnosis of metastatic carcinoma is made, coordinated care with the oncologist and eye care provider is important. Treatment options generally center around systemic platinum-based chemotherapy or localized ocular therapy, such as external beam radiation (EBRT) or plaque therapy. For bilateral tumors, EBRT is the treatment of choice.4
The patient’s oncologist was notified of our findings and referred him to an ocular oncologist. The patient was put back on his chemotherapy regimen and by the time he saw the ocular oncologist, it was felt the metastatic tumor was beginning to regress, so no localized treatment was initiated. He continues to be followed.
1. De Potter P. Ocular manifestations of cancer. Curr Opin Ophthalmol. 1998 Dec;9(6):100-4.2. Ningh N, Kulkarni P, Aggarwal AN, et al. Choroidal metastasis as a presenting manifestation of lung cancer; a report of 3 cases and systematic review of the literature. Medicine. 2012;91:179-94.
3. Shields CL, Shields JA, Gross NE, et al. Survey of 520 eyes with uveal metastases. Ophthalmology. 1997 Aug;104(8):1265-76.
4. Kanthan GL, Jayamohan J, Yip D, Conway RM. Management of metastatic carcinoma of the uveal tract: an evidence-based analysis. Clin Experiment Ophthalmol. 2007;35:553–65.
Retina Quiz Answers:
1) d; 2) c; 3) d; 4) b.

