 |
|
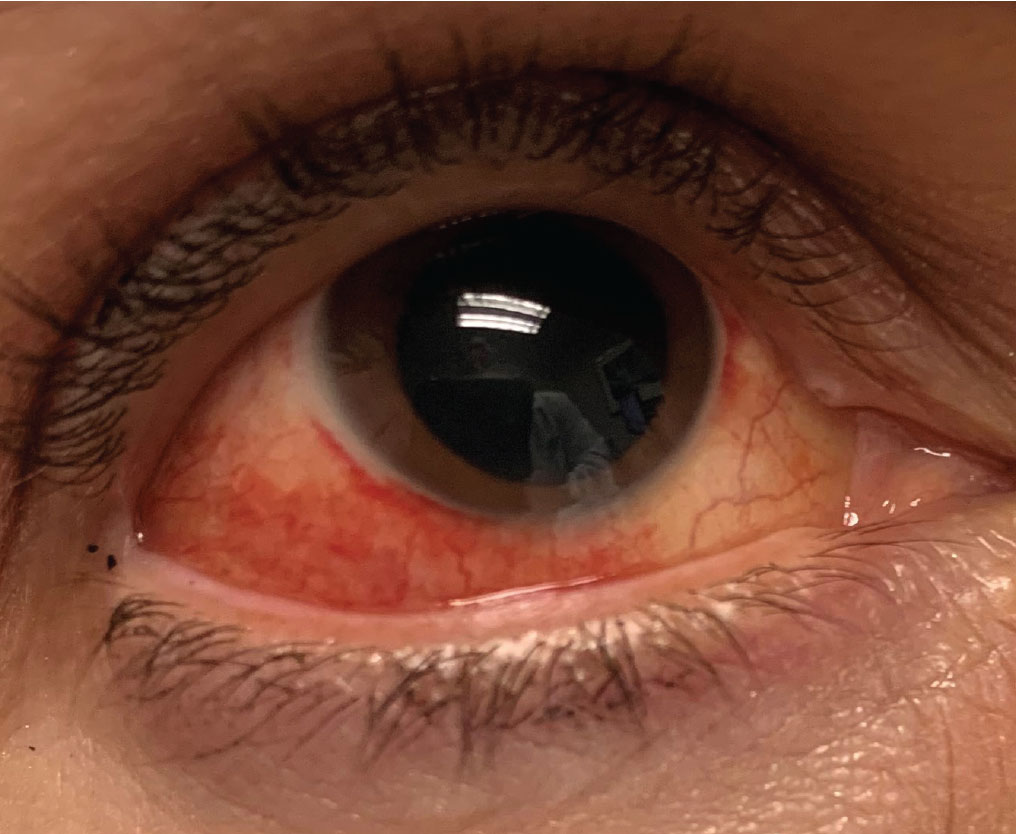
Using a dynamic algorithm to determine the urgency of red eye cases may be more effective than using a static flowchart, researchers found. Photo: Joseph W. Sowka, OD. Click image to enlarge. |
Primary care physicians, tasked with triaging virtually any condition, typically rely on static flowcharts as a diagnostic aid when evaluating patients with red eye. However, these tools only offer clinicians a general idea about a patient’s disease and fail to describe the next steps necessary to confirm the urgency of the condition. This cookie-cutter approach to triage can lead to extraneous referrals and delayed treatment.
In search of a more reliable way to diagnose cases of red eye, a team of researchers recently put a novel Bayesian algorithm to the test, which was developed as a mobile application called Pickle. “Clinical specialists’ diagnostic ability stems from Bayesian thinking,” the researchers explained in their paper for the journal Vision. “Their differential diagnosis is continuously adjusted at each step of decision-making by history or physical exam findings (pre-test odds), which inform their next clinical step.”
Here's how it works: the app first presents the clinician with three to four questions that can be answered with “yes,” no” or “I don’t know” and then produces a differential diagnosis ranked by likelihood based on the responses. Artificial intelligence is then used to determine the next step for the workup. The question rounds continue to repeat—re-sorting the differential list after each response—until the user terminates the program or “the level of suspicion for the top diagnosis heavily outweighs that of the others,” the researchers explained. Once a differential is chosen, symptoms and medical history factors that are either associated with the condition or, conversely, don’t support the diagnosis are presented on the screen.
The research team conducted a prospective study to see if this dynamic approach to red eye workups yields greater diagnostic accuracy than traditional flowcharts. They distributed a paper version of the questionnaire to emergency departments in Ontario, Canada, that referred 57 adult patients with red eye to an ophthalmology urgent eye clinic. The diagnoses made by the urgent care (referring) physicians using the algorithm were then compared with the diagnoses made by an independent ophthalmologist.
This is what the researchers found: “The referrer’s diagnostic accuracy was 70.2%, while the algorithm’s accuracy was 68.4%, increasing to 75.4% with the algorithm’s top two diagnoses included and 80.7% with the top three included,” they reported in their paper. “In urgent cases of red eye, the referrer diagnostic accuracy was 76.9%, while the algorithm’s top diagnosis was 73.1% accurate, increasing to 84.6% (top two included) and 88.5% (top three included).”
The team concluded that the algorithm may help non-ophthalmologists better handle and refer cases of red eye—plus, the approach doesn’t require slit lamp findings aside from noting white opacities and fluorescein uptake. The novelty of the approach, according to the researchers, “lies in its dynamic nature: it adjusts the sequence of workup steps as it receives clinical findings, mimicking a specialist’s approach.” Additionally, it’s useful and unique in its ability to provide a list of potential diagnoses rather than only one.
“This study obtained a referring diagnostic accuracy of 70.2%,” the researchers wrote. “Using Pickle’s Bayesian algorithms, diagnostic accuracy was improved to a range of 68.4% to 80.7%. It may, therefore, be used in primary care settings as an adjunct to clinical judgment to optimize referral decisions for serious and urgent conditions,” they concluded.
Deans AM, Basilious A, Hutnik CM. Assessing the performance of a novel Bayesian algorithm at point of care for red eye complaints. Vision. October 24, 2022. [Epub ahead of print]. |

