 |
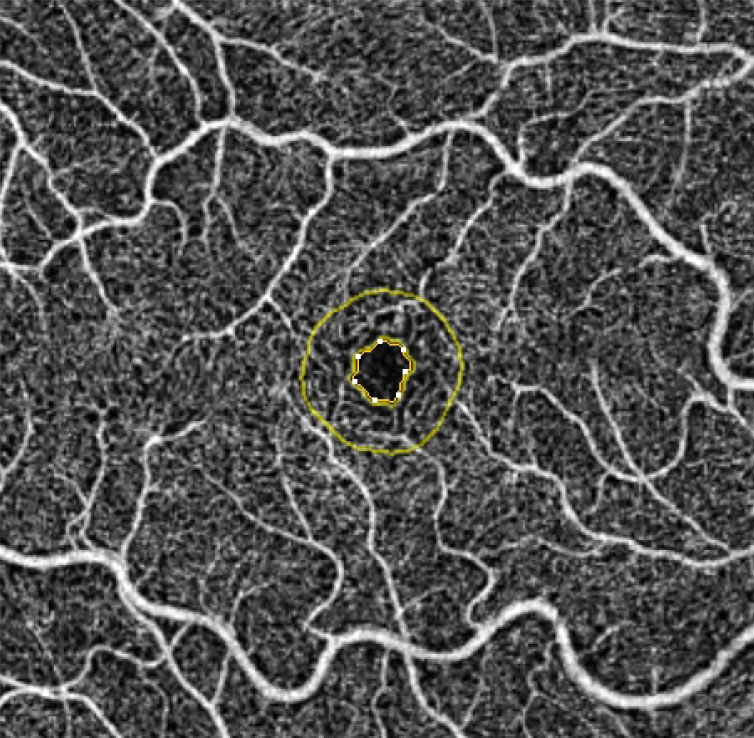
| This study found genetically predicted higher retinal vessel density leads to smaller global cortical thickness. Photo: Julie Rodman, OD. Click image to enlarge. |
A recent analysis of genome-wide association studies that included measurements of retinal vessel density and distribution further illuminates the link between the eyes and the brain.
Features of cortical thickness and surface area were able to be extracted from 51,665 patients across 60 cohorts from the UK Biobank. Both these features were measured globally and in 34 functional regions using MRI. The study researchers found higher retinal vessel density was related to decreased cortical thickness at the global level. Specific retinal vessel branching patterns were related to cortical thickness within the superior temporal sulcus and transverse temporal region at the functional level. Surface area was correlated with vessel density for subregions of the frontal and temporal lobes, as well as to the cortical thickness of the inferior temporal, entorhinal and pars opercularis regions. Also, causation was observed between surface area of the parahippocampal and cauda middle frontal gyrus and retinal vessel density.
In their paper on the work for Ophthalmology Science, the researchers point out that the causal relationship remained even when accounting for BMI and blood pressure. They continue that the rationale for this study is based on the idea of retinal vascular health mirroring cerebral circulation, since the brain and retina have numerous similarities.
Explaining each major finding, the researchers start by expanding upon vessel density’s influence of entorhinal cortical thickness. This area exhibits functional and histological alterations in preclinical Alzheimer’s disease. Similarly, the surface areas of the caudal middle frontal region and inferior parietal region, along with the cortical thickness of the banks of the superior temporal sulcus, were all causally impacted by retinal vessel alterations—all structures that present with morphological changes in Alzheimer’s.
The cingulate gyrus is also affected early in Alzheimer’s onset, participating in emotion and memory changes. The surface area of the caudal anterior cingulate, rostral anterior cingulate and posterior cingulate were all causally related to retinal microvasculature. What’s more, this is the first study to date finding a direct causal link between organ-specific pathologies, like with surface areas of parahippocampal and caudal middle frontal regions influencing retinal vasculature. These two cerebral regions are implicated in Alzheimer’s, but previous research has only observed concomitance of the disease with retinal vascular anomalies, not a direct link.
The study also revealed a connection between retinal vessel integrity and specific brain functions. The inferior temporal cortex is crucial in visual perception and was causally affected by vessel density. The findings indicate microvascular deterioration of the retina may cause impairments beyond basic visual deficits and into sophisticated aspects of visual interpretation.
Along with more specific observations, the authors concluded: “These findings reinforce the prospective utility of retinal vasculature as a surrogate marker for neuropathological states, proposing that affordable and noninvasive fundus imaging could serve as a viable screening tool for neuropsychological diseases. This study could provide immediate value for clinical research and afford a robust foundation for the innovation of predictive methods and risk assessment tools for neuropsychiatric disorders.”
Wei X, Iao WC, Zhang Y, Lin Z, Lin H. Retinal microvasculature causally affects the brain cortical structure: a Mendelian randomization study. Ophthalmol Sci. January 23, 2024. [Epub ahead of print]. |

