 |
|
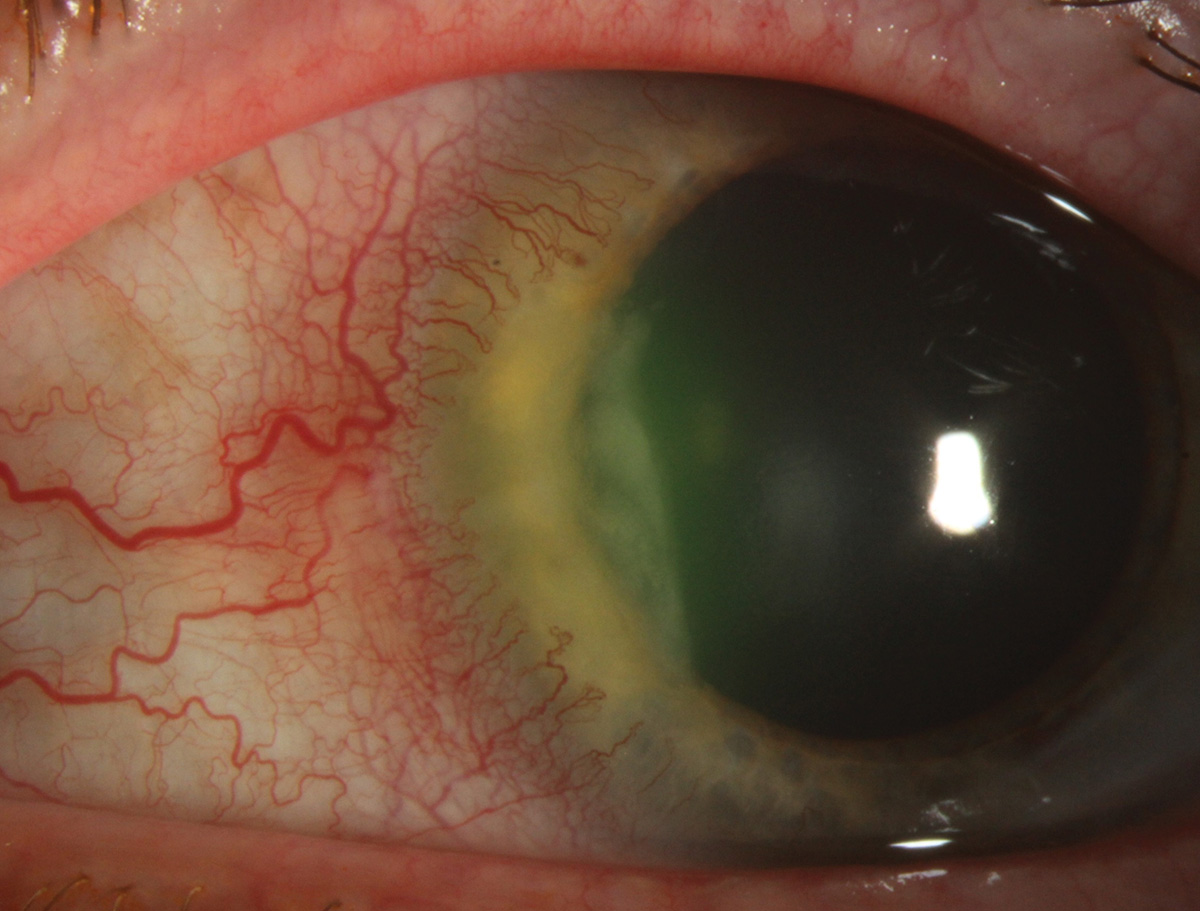
The clinical outcomes in PUK with underlying autoimmune disorders were observed to be better than nonautoimmune etiologies, which may be attributed to the early detection of the PUK-related changes and aggressive medical management in such patients. Photo: University of Iowa. Click image to enlarge. |
In a new study, researchers assessed the demographic characteristics, presentations and risk factors impacting the outcomes in patients diagnosed with peripheral ulcerative keratitis (PUK). A total of 58 eyes of 51 patients diagnosed with PUK at a single center (the University of Pittsburgh School of Medicine) were included; 58.8% were female. More than 85% of the patients had unilateral cases of PUK and presented with corneal thinning, recurrent epithelial defect and anterior chamber inflammation. A descriptive analysis of the demographics, clinical history and presentation was performed, and the influence of underlying autoimmune was explored. The authors also evaluated the correlation between treatment duration and final best corrected visual acuity (BCVA).
More than 60% of patients had a history of autoimmune disorders. Among these patients, 45% had a history of rheumatoid arthritis and a few patients had been diagnosed with more than one autoimmune disorder. Previous studies have reported rheumatoid arthritis to be the primary non-infectious cause of PUK, while Mooren’s ulcer was the second most common cause.
“The inflammatory responses that lead to PUK have been associated with history of previous traumatic events such as ocular trauma or surgery,” the researchers explained in their Cornea paper on the work. “Srinivasan et al. observed that patients with PUK had a history of ocular trauma (26%) and surgery (37%). Similarly, Sharma et al. also reported a history of ocular trauma (4%) and surgery (28%) in their study. A similar proportion of patients with PUK had a history of similar inciting factors, that is, ocular trauma (three patients, 5.88%) and surgery (11 patients, 21.57%) in our cohort.”
Only three patients presented with corneal perforation during the treatment and needed surgical intervention. BCVA in patients with nonautoimmune etiologies worsened, whereas the final BCVA in patients with an underlying autoimmune disorder was better than the presenting BCVA.
“Although the initial BCVA depended on the epithelial defect size, the visual outcomes in patients with PUK after treatment did not have a significant correlation with it,” the authors explained. “Interestingly, we observed the PUK resolution time in patients with underlying autoimmune etiologies was significantly shorter than in those with non-autoimmune etiologies, which we attribute to aggressive systemic immunosuppressive management in these patients supplemented by topical immunosuppression.”
The researchers concluded by noting that “patients with PUK often present with severe disease and require comprehensive ophthalmic and systemic evaluation to assess the underlying etiologies and tailoring an aggressive management plan accordingly. Since autoimmune disorders are the primary causes of PUK in many patients, high clinical suspicion and close coordination between the patient’s ophthalmologist and rheumatologist is necessary for timely management of PUK.”
Singh RB, Atta S, Srikumaran D, Jhanji V. Demographic characteristics, clinical presentations and risk factors impacting visual outcomes in peripheral ulcerative keratitis. Cornea. February 13, 2024. [Epub ahead of print.] |

