It’s safe to assume the majority of you are thinking about skipping this article, believing it has absolutely nothing to do with the way you practice. Well, think again. Let’s take a step back for a moment and reflect on some of the technological changes to eye care over the past several years. Optical coherence tomography (OCT) came to the market in the early 2000s and quickly changed the way we diagnose and manage glaucoma and retinal conditions.1,2 The mid-2000s brought the ever-growing popularity of 1-800-CONTACTS. In 2007, Zenni Optical drastically changed the optical world when it started marketing online glasses at a fraction of the price. Skip ahead to 2013 and Opternative offers online refractive exams that it markets as being “as accurate as a traditional refractive exam performed by an optometrist or ophthalmologist using a phoropter.”3
As the landscape of medicine continues to evolve, telehealth is at the forefront. It is not inconceivable to envision a time when telemedicine becomes the norm. In 2015, Kaiser Permanente performed 14 million virtual visits.4 They predict that virtual visits will actually outnumber traditional in-person visits by 2018.4 As technology advances and the infrastructure for such examination modalities expands, one can only expect patients to continue to embrace this concept.
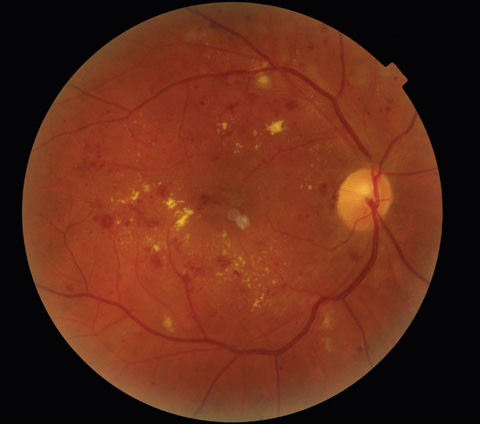 |
| This patient’s last reported eye exam was in July 2014 at an unknown location. Teleretinal imaging was performed in November 2014 and revealed severe nonproliferative diabetic retinopathy with probable clinically significant macular edema (CSME) in both eyes. Click image to enlarge. |
Telehealth appointments can improve access, offer cost savings, and provide convenience to patients. Optometry can embrace this by implementing teleretinal screening for diabetic patients and forming strong relationships with local primary care providers. Teleretinal screening programs are already being applied throughout the Veterans Affairs (VA) system, the Joslin Vision Network (JVN), and via web-based applications such as the Eye Picutre Archive Communication System (EyePACS).5,6 It’s time to start thinking of telemedicine like Darwinism: if you don’t adapt to our evolving profession, you may not survive.
Quick Diagnoses for Prompt Treatments
Diabetes is the leading cause of new blindness in adults in the United States.5,6 A 2014 CDC report shows more than 29 million Americans have diabetes but 27.8% of patients are undiagnosed.7 The American Diabetes Association recommends retinal examinations annually. However, despite this recommendation, only 60% of patients with diabetes have their eyes examined regularly.6,8 But while those studies show worrisome numbers, others suggest hope. For instance, effective blood glucose control and the early evaluation and treatment of diabetic retinopathy can lead to favorable visual outcomes.9,10
The VA and Indian Health Service have a disproportionate rate of diabetes patients (25% and 16% to 33.5%, respectively) compared with the general population (9%).7,11,12 This large cohort of patients requiring timely evaluation of diabetic retinopathy creates a major health care burden. In 2001, Congress recommended the VA collaborate with JVN, a leader in diabetic teleretinal imaging (TRI), to provide teleretinal services as a screening tool for patients with diabetes in the VA.13 Teleretinal imaging has since become commonplace at VA hospitals and community based outpatient clinics throughout the country. It’s an accurate and effective method of assessing the retina for the presence of sight-threatening diabetic retinopathy.14,15
 |
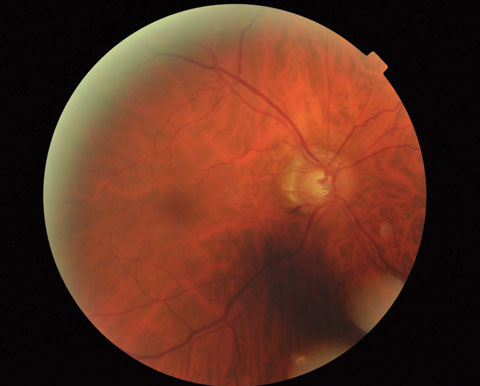
| This image shows the left eye of the patient above. The patient was referred to a retinal specialist where OCT confirmed the presence of CSME OU and widefield angiography demonstrated retinal capillary nonperfusion in the periphery. Panretinal photocoagulation and intravitreal bevacizumab were performed in both eyes at follow-up. Click image to enlarge. |
The primary goal of TRI is to screen for vision-threatening diabetic retinopathy and allow for prompt treatment. Moreover, TRI can reduce the risk of vision loss from diabetic macular edema and proliferative neovascularization.14,16 TRI does not take the place of a dilated eye examination. The VA continues to recommend dilated exams every one to two years in coordination with TRI. Teleretinal imaging is particularly valuable in the VA and other hospital systems in which patients must travel long distances for an ocular examination due to the large catchment area with remote and rural locations. Telehealth allows diabetes patients to have their annual retinal screening performed closer to home minimizing travel time—time away from work for the patient and their family, as well as improving convenience for those with mobility issues.
The TRI procedure consists of retinal images of the posterior pole, superotemporal arcade, nasal retina and anterior segment taken by a trained technician.13,14,17 Images are remotely reviewed by a credentialed reading specialist (optometrist or ophthalmologist) who grades the level of retinopathy based on established guidelines from the Early Treatment Diabetic Retinopathy Study (ETDRS).10 Patients with levels of mild diabetic retinopathy or greater are referred to the eye clinic for a dilated exam. Incidental ocular findings such as hypertensive retinopathy, retinal emboli, macular degeneration, choroidal nevi and suspicious optic disc cupping also prompt referrals. Those without diabetic retinopathy, or other ocular findings, are typically evaluated by an eye care provider within one to two years.
TRI: A Screening Companion
Teleretinal imaging has limitations and is not suitable for all patients. It can be difficult to obtain high quality images on individuals with small pupils, media opacities, and physical and/or mental impairments. Image quality is also highly dependent on the skill level of the imaging technician. Telehealth technicians undergo specific camera training and learn to manipulate the camera with difficult images. Overall, however, the image quality with teleretinal screening is highly successful and several studies boast rates of readable images (i.e., free of artifacts and aberrations) greater than 85%.14,15,18 Additionally, traditional in-office examinations in conjunction with TRI has helped the VA evaluate an astounding 90% of its diabetes patients on a yearly or biannual basis as medically indicated.19
 |
| This teleretinal photograph demonstrates a highly suspicious case of glaucoma in the patient’s right eye. Despite the shadow, there is obvious rim thinning inferiorly with an adjacent Drance hemorrhage. Click image to enlarge. |
Teleretinal imaging has the capability to overcome many of the obstacles impeding traditional diabetic retinopathy surveillance, including: socioeconomic factors, lack of patient and physician awareness to the importance of annual retinal exams, and geographic challenges.16 However, barriers exist to implementing TRI in many primary care clinics. One of the largest impediments to widespread adoption of TRI is equipment cost. On average, a nonmydriatic retinal camera costs $15,000 to $25,000.20 Moreover, there are additional costs of training, IT support, infrastructure and software. Reimbursement for TRI can also be a challenge.
Teleretinal imaging does not take the place of a comprehensive eye examination. There is a common misconception that the use of telemedicine will result in fewer referrals for eye care services. The goal of TRI is to capture the 40% of diabetes sufferers who are noncompliant with annual retinal examinations.6,8 It has been found that establishing a TRI program with primary care actually generates more workload for the affiliated eye clinic.19 Several cohort studies have found that approximately 25% to 43% of patients screened through TRI are referred for additional ophthalmic care.6,14,19 The most common reasons for referral are diabetic eye disease, optic nerve-related disease, lens opacities and macular degeneration.23-25 Studies have also shown that TRI has excellent sensitivity and specificity when screening for these common ocular conditions.23-25
This premise is also closely held by Gerald Selvin, OD, Chief of Optometry, Boston Healthcare System—a national leader in the VA TRI program—who notes, “Teleretinal imaging for diabetes risk management is the tip of the iceberg. In short order we should be screening for many other commonly occurring conditions, including AMD and glaucoma and other conditions as well. Our job is to make sure it is safe, but I think telehealth will occupy a much bigger part of VA and non-VA health care in the future.”
 |
| This teleretinal image shows a retinal plaque in the superotemporal arcade at the second bifurcation. The patient was examined in clinic and an additional plaque was noted along the inferotemporal artery. A carotid duplex revealed 80% to 99% stenosis in the right internal carotid artery. The patient underwent a successful carotid angioplasty and stenting to relieve the stenosis. Click image to enlarge. |
Partnering With PCPs
Introducing teleretinal screening at the point of care of the primary care provider improves the detection rate of diabetic retinopathy, and optometry needs to be closely involved.16,19 Welch Allyn is now marketing a small, portable retinal camera to primary care providers (PCPs) to improve the management of their diabetes patients at a fraction of the cost of a full nonmydriatic camera. The RetinaVue100 (Welch Allyn) imager transfers nonmydriatic images via a secure network to a board-certified retinal specialist; reports and referral plans are even generated the same day for the PCP.21 Other companies have developed software to analyze the retinal photographs without the use of a certified reader. It is able to detect diabetes-related retinal anomalies (i.e., microaneurysms, intraretinal hemorrhages, neovascularization, and cotton wool spots) and also perform a serial analysis to identify retinal changes from year to year.26,27
Optometry should embrace telehealth services, not as a substitution to face-to-face patient care but as an additional avenue to reach patients and achieve the common goal of minimizing preventable visual impairment. Creating a partnership with our primary care colleagues will generate new referrals and provide diabetic retinal screenings to those unlikely to follow-up independently. Now is the time to strengthen bonds with other physicians. Now is the time to exert yourself in the field. Now is the time to step into 21st century eye care. Now is the time to act. Will you adapt to our ever-changing profession or will you be left behind?
Dr. Zimbalist practices at the Harry S. Truman Memorial Veterans’ Hospital in Columbia, Mo.
Dr. Scharnweber practices at the St. Cloud VA Health Care System in St. Cloud, Minn.
|
1. Dunbar, M, McSoley J. The OCT in retina and glaucoma. Lecture Presented. Minnesota Association of Optometrists and Opticians. 2009. Available at http://maoo.org/wp-content/uploads/2009/08/GL-Retx6.pdf. 2. Jaffe G, Caprioli J. Optical coherence tomography to detect and manage retinal disease and glaucoma. Am J Ophthalmol. 2004 Jan;137(1):156-69. 3. Dow CT. Opternative: Clinical trial summary report. Available at www.opternative.com/clinical-study. Accessed August 29, 2016. 4. Pearl R. Engaging physicians in telehealth. New England Journal of Medicine: Catalyst. Available at http://catalyst.nejm.org/engaging-physicians-in-telehealth/. Updated March 29, 2016. Accessed September 13, 2016. 5. Fox C, Kronenberg K, Chu G, Bakir B, et al. Increasing eye care screening and referral for people with diabetes via telehealth programs. Available at http://dhhs.ne.gov/publichealth/Documents/Vision121010.pdf. Accessed August 25, 2016. 6. Ogunyemi O, George S, Patty L, et al. Teleretinal screening for diabetic retinopathy in six Los Angeles urban safety-net clinics: final study results. AMIA Annu Symp Proc. 2013 Nov 16;2013:1082-8. 7. National Center for Chronic Disease Prevention and Health Promotion, Division of Diabetes Translation. CDC: Center for disease control and protection. 2014 National Diabetes Statistics Report. Last updated: May 15, 2015. Available at www.cdc.gov/diabetes/data/statistics/2014statisticsreport.html. Accessed September 1, 2016. 8. Diabetic Retinopathy PPP-Updated 2016. American Academy of Ophthalmology Preferred Practice Patterns: Retina/Vitreous Panel, Hoskinzs Center for Quality Eye Care. Available at www.aao.org/preferred-practice-pattern/diabetic-retinopathy-ppp-updated-2016. Accessed August 30, 2016. 9. The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993;329:977–86. 10. Early Treatment Diabetic Retinopathy Study Research Group. Early photocoagulation for diabetic retinopathy. ETDRS report number 9. Ophthalmology. 1991 May;98(5 Suppl):766-85. 11. Veterans Health Administration. Close to 25 percent of VA Patients Have Diabetes. American Diabetes Month — Time to Take Action. Updated: April 17, 2015. Available at www.va.gov/health/NewsFeatures/20111115a.asp. Accessed September 1, 2016. 12. National Center for Chronic Disease Prevention and Health Promotion, Division of Diabetes Translation. CDC: Center for disease control and protection. Diabetes among American Indians and Alaska Natives. 2011. Available at www.cdc.gov/diabetes/data/statistics/2014statisticsreport.html. Accessed September 27, 2016. 13. Conlin P, Fisch B, Orcutt J, et al. Framework for a national TRI program to screen for diabetic retinopathy in Veterans Health Administration patients. J Rehabil Res Dev. 2006;43:741-8. 14. Cavallerano A, Cavallerano J, Katalinic P, et al. Joslin Vision Network Clinical Team. A telemedicine program for diabetic retinopathy in a Veterans Affairs Medical Center--the Joslin Vision Network Eye Health Care Model. Am J Ophthalmol. 2005;139:597-604. 15. Cavallerano A, Conlin P. Teleretinal imaging to screen for diabetic retinopathy in the Veterans Health Administration. J Diabetes Sci Technol. 2008 Jan;2(1):33-9. 16. Garg S, Zimmer-Galler I. Telemedicine and remote imaging for diabetic rettinopathy evaluation: an update. Retinal Physician. March 2013. 30-32. Available at: http://www.med.unc.edu/ophth/files/GargTelemedicineRetinalPhysicianMag.pdf. Accessed: August 25, 2016. 17. Cavallerano J, Aiello L, Cavallerano A, et al. Joslin Vision Network Clinical Team. Nonmydriatic digital imaging alternative for annual retinal exam in persons with previously documented no or mild diabetic retinopathy. Am J Ophthalmol. 2005; 140:667-73. 18. Ogunyemi O, Terrien E, Eccles A, et al. Teleretinal Screening for Diabetic Retinopathy in Six Los Angeles Urban Safety-Net Clinics: Initial Findings. 2011;1027–35. 19. Chasan J, Delaune B, Maa A, et al. Effect of a teleretinal screening program on eye care use and resources. JAMA Ophthalmol. 2014 Sept; 132(9):1045-1051. 20. Veatch Ophthalmic Instruments. Non-mydriatic retinal cameras. Available at www.veatchinstruments.com/Non-Mydriatic-Retinal-Cameras. Accessed September 28, 2016. 21. WelchAllyn. RetinaVueTM Network. Available at www.welchallyn.com/en/products/categories/population-health-management-technologies/diabetic-retinopathy-screening/retinavue-network.html. Accessed September 7, 2016. 22. Aetna. Retinopathy Telescreening Systems. Available at www.aetna.com/cpb/medical/data/500_599/0563.html. Accessed August 25, 2016. 23. Gangwani R, McGhee SM, Lai JS, et al. Detection of glaucoma and its association with diabetic Retinopathy in a Diabetic Retinopathy Screening Program. J Glaucoma. 2016 Jan;25(1):101. 24. Duchin KS, Asefzadeh B, Poulaki V, et al. Teleretinal imaging for detection of referable macular degeneration. Optom Vis Sci. 2015 Jun;92(6):714-8. 25. Maa AY, Patel SP, Chaan JE, et al. Retrospective evaluation of a teleretinal screening program in detecting nondiabetic eye disease. Telemedicine and e-health. 2017 Jan;1:1-8. 26. Walton OB, Garoon RB, Weng CY, et al. Evaluation of automated teleretinal screening program for diabetic retinopathy. JAMA Ophthalmol. 2016;134(2):204-9. 27. Sim DA, Keane PA, Tufail A, et al. Automated retinal image analysis for diabetic retinopathy in telemedicine. Curr Diab Rep. 2015 Mar;15(3):14. |

