 |
A 72-year-old Caucasian female presented in November 2021 for a glaucoma progress evaluation as scheduled. She reported good compliance with her meds.
Case
She was initially seen as a new patient in the summer of 2018 with complaints of blurred vision OU. At that time, it had been approximately five years since her last visit to an eye care provider. Entering visual acuities were 20/40 OD and 20/60 OS. Best-corrected visual acuities through hyperopic astigmatic correction were 20/20 OD and 20/60 OS. Pupils were ERRLA, with a subtle APD noted OS. EOMs were full in all positions of gaze.
A slit lamp examination of the anterior segments was remarkable for slightly narrowed anterior chamber angles. Otherwise, the anterior segments were unremarkable. Gonioscopy demonstrated similar findings with slightly narrowed angles; on indentation gonioscopy, the angles were easily opened further. It was deemed that the patient was safe to dilate. Prior to dilation, applanation tensions were 19mm Hg OD and 24mm Hg OS.
Through dilated pupils, the crystalline lenses were characterized by mild nuclear sclerosis OD and slightly more advanced nuclear cataracts OS. Bilateral PVDs were present. The patient’s cup-to-disc ratios were judged to be 0.40x0.45 OD and 0.85x0.90 OS, with the left neuroretinal rim quite thinned temporally and eroded inferotemporally. A subtle wedge defect was seen clinically.
Her macular evaluations were essentially normal, with age-appropriate RPE granulation. Her retinal vascular examination was characterized by mild arteriolar sclerosis, consistent with her age and general health history of hypertension and hyperlipidemia, which was controlled by a calcium channel blocker and a statin. Her peripheral retinal evaluation was entirely normal. Fundus photos were obtained and, given the likelihood of glaucomatous damage, she was schedule for a follow-up in one to two weeks for a full glaucoma work-up.
She presented as scheduled, and her IOPs were essentially the same. Pachymetry readings were 562μm OD and 525μm OS. HRT 3 findings confirmed optic cupping asymmetry, and OCT baseline scans demonstrated a normal series of findings in the right eye, but thinned BMO-MRW values in the left, along with thinning of the circumpapillary RNFL tissue at three circle scan diameters. These OCT findings correlated with the clinical in vivo findings seen at the slit lamp.
Based on the findings, glaucoma was diagnosed in the left eye, with the right at that time being diagnosed only as suspect. Travatan Z (travoprost, Novartis) one drop HS OS was initiated, and the patient was asked to return for follow-up in about two to three weeks to assess the efficacy of the medical therapy and obtain baseline visual field studies.
The patient presented as asked. Applanation tensions were 17mm Hg OD and 15mm Hg OS. There were no localized inflammatory side effects from the medication in the left eye, and she reported good compliance. Threshold visual field studies were essentially clear OD. The left demonstrated above and below arcuate defects, with fixation involvement in the superior field. UBM studies of the anterior chamber angles demonstrated classic findings of plateau iris configuration OS>OD. Best-corrected visual acuities remained at 20/20 OD and 20/60 OS.
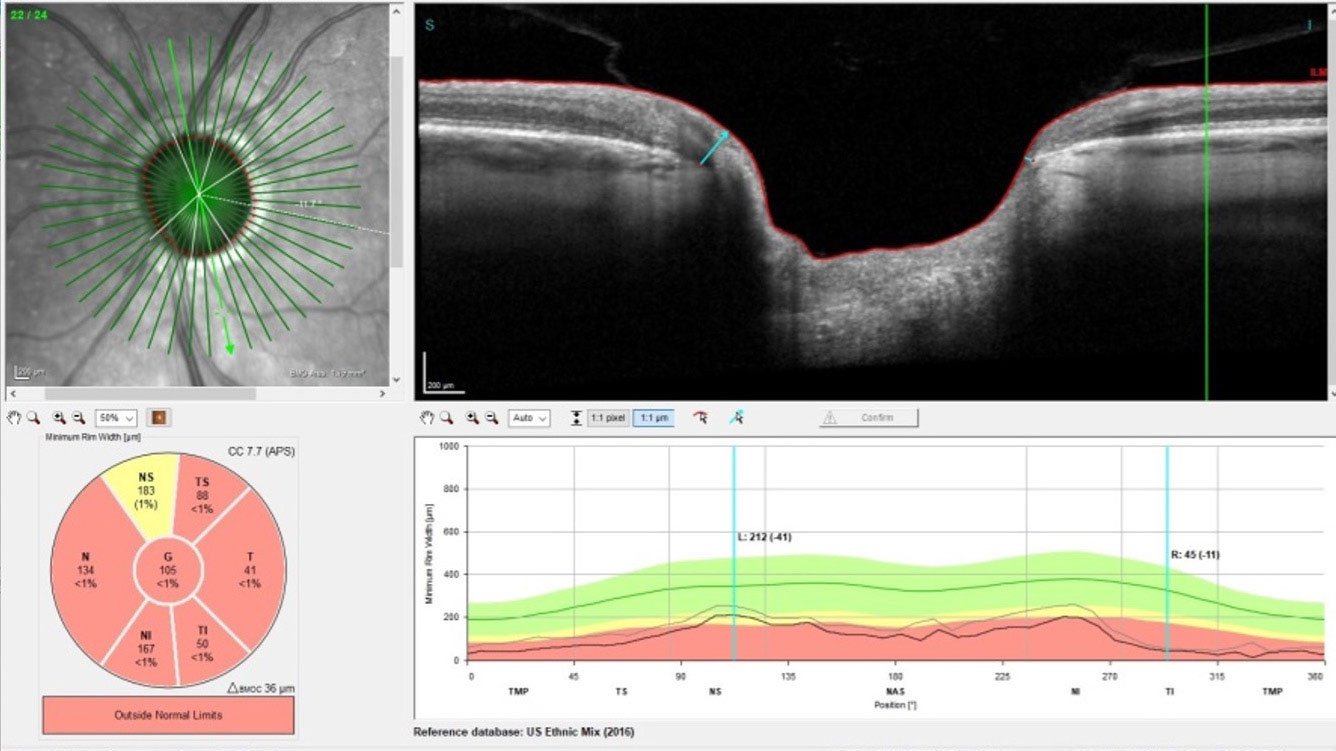 |
| Progression can be seen in the damage to the neuroretinal rim OS. Click image to enlarge. |
Progression
While the initial response to the Travatan Z was encouraging, stability of glaucoma that is medicated cannot be determined over one or two visits. In fact, it needs to be continually assessed at each follow-up, as the condition may progress in spite of therapy. So, in essence, especially in new patients such as this one, there should be a period of close assessment to ensure that the patient is in fact stabilized. During this period, both structural and functional testing is repeated to determine stability. And of course, as in cases such as this where there is significantly advanced disease, there is a higher likelihood that the more advanced eye will progress to a greater extent than the fellow, less advanced eye.
Over the subsequent 18-month period, there were some adjustments to the patient’s medication schedule, and ultimately, she was also put on medication in her right eye, as subtle changes were seen on OCT. Due to the decreased acuity in the left eye and the cataract being somewhat denser than the right, we opted to proceed with cataract surgery. The procedure was performed without complication and two iStents (Glaukos) were implanted into the left nasal anterior chamber angle. Unfortunately, visual acuity was not significantly improved with cataract extraction, owing to the visual field defects OS that involved fixation.
As far as glaucoma stability was concerned, several adjustments were made to her medications during this period until we were finally able to develop a therapeutic combination that resulted in stability. Usually, but not always, once I feel comfortable that the patient has been stabilized, we tend to space out our follow-up visits so they don’t become a burden to the patient. That said, each follow-up is still accompanied by the appropriate testing needed to ensure stability and no further progression. After much time and effort, we finally got to that point.
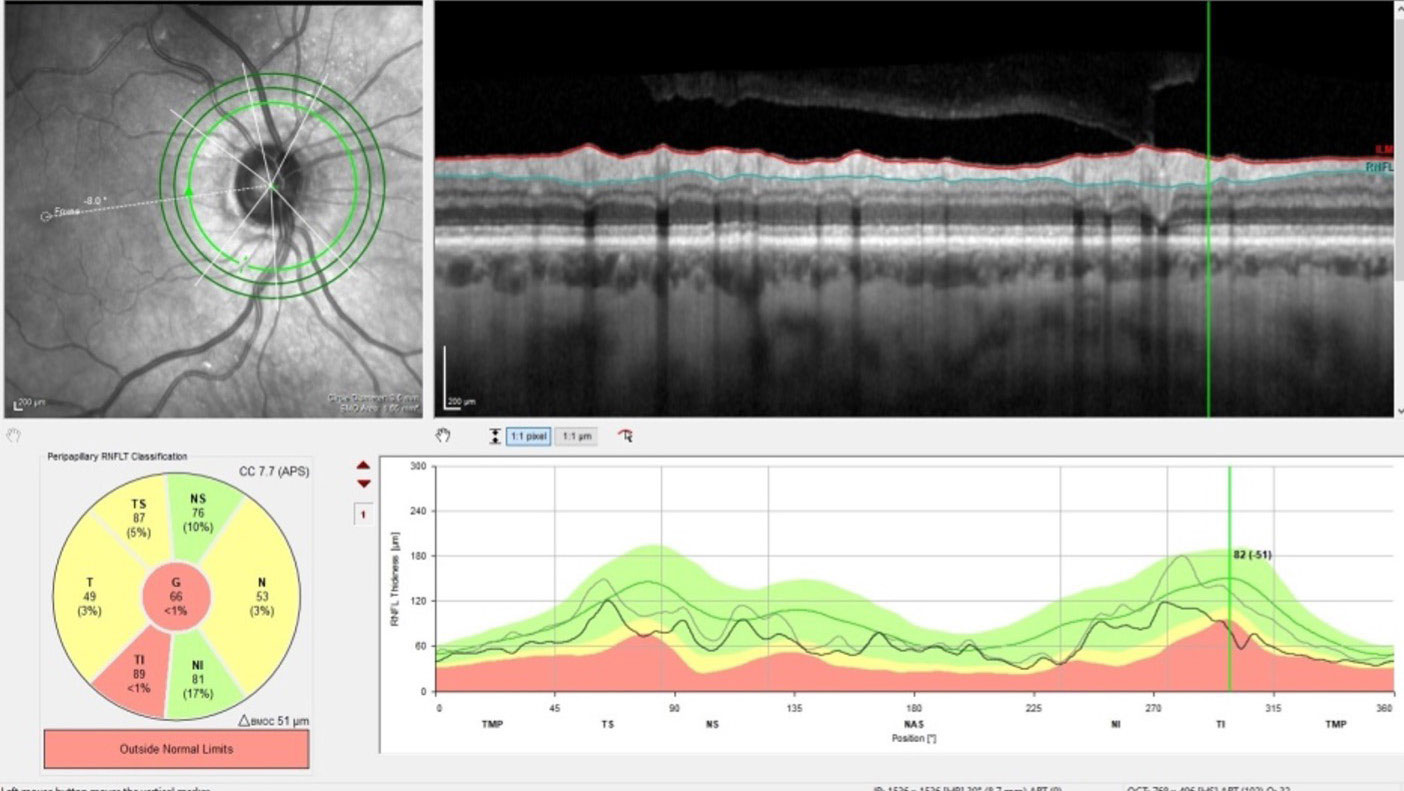 |
| Changes in perioptic RNFL indicate conversion to frank glaucoma. Click image to enlarge. |
And then COVID-19 hit and interfered with patient care. Unfortunately, for the better part of 2020, the patient did not feel comfortable coming into the office for follow-up visits, but we did stay in communication, her medications were refilled appropriately and she reported good compliance with no overt changes to her vision.
When she did finally present to the office in January 2021, IOPs were 18mm Hg OD and 19mm Hg OS. Unfortunately, there was documented progression of neuroretinal rim and RNFL thinning. IOPs over the next two visits averaged 15mm Hg OD and 18mm Hg OS. Given the amount of damage that was present in the left eye, these IOPs were not at an adequate level to prevent further damage. We discussed options regarding medication modification, SLT and surgical intervention. Jointly, we decided to explore a medication change to the left eye to bring about stability, with the understanding that surgery may be likely.
Fortunately, we were able to obtain a significant decrease in pressure OD and OS with a change involving a nitrous oxide inhibitor. Visual fields, OCTs and HTR 3 studies performed throughout the second half of the year demonstrated no change or progression. We were finally back at the point where I felt she was stable enough to spread out her visits.
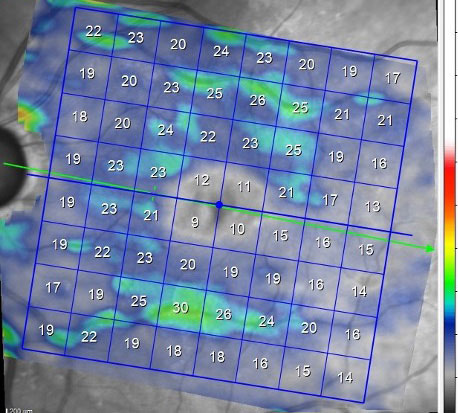 |
| Note the paucity of the ganglion cell layer in the macula OS. Click image to enlarge. |
Discussion
It’s a relief to the provider and certainly to the patient when we reach that point of relative stability. Though it may not last forever, it does give us some breathing room. However, what happens at the end of the year to our Medicare Part D patients who are on chronic medical therapy? They get notified that the cost of their medications is changing, and usually not for the better. And that is exactly what the patient told me in December: her medication costs were changing, and she would not be able to afford one of the two medications that were keeping her stable.
A frustrating situation for the patient and myself indeed. The patient is finally stable, but then an insurance issue interferes with patient care. What do you do? These situations are difficult, and this patient was educated previously that surgical intervention may be in her future. Can you argue with the insurance company? Sure, just like you can argue with a stop sign. Can the patient change their coverage? Yes, and many do play the year-end game of looking for a plan that better covers their medications, but what is going to happen next year? The same thing, of course.
With some commercial insurances that require prior authorization, sometimes using the wording, “the patient will undisputedly lose vision without XYZ medication,” is enough to give the patient access to the medication they need. With Medicare, unfortunately, that usually does not work.
Who gets shorted in these situations? The patient, of course. Our job is to provide the best care we can, in spite of the hurdles in our way. So, we figure out a way. How you proceed depends on several factors, as each case is different, but we proceed nonetheless.
Dr. Fanelli is in private practice in North Carolina and is the founder and director of the Cape Fear Eye Institute in Wilmington, NC. He is chairman of the EyeSki Optometric Conference and the CE in Italy/Europe Conference. He is an adjunct faculty member of PCO, Western U and UAB School of Optometry. He is on advisory boards for Heidelberg Engineering and Glaukos.

