 |
With ebola, and now Zika, making headlines around the globe, it’s clear vector-borne infection has become a significant public health threat. Travel and changing land use have increased the risk of new pathogens emerging, as well as existing agents previously confined to small, remote areas re-emerging and crossing borders.
Infection, Transmission and Disease
In infectious disease, the absence or presence of the etiological agent is the main determining factor in the epidemiology of the condition. While disease cannot occur in the absence of the agent, disease may not always result from the presence of the agent. The distinction between infection and disease is important:
Infection is the invasion of a living organism (the host) by another living organism (the agent).1
Disease is a derangement in the function of the whole body of the host, or any of its parts.1
A vector is an invertebrate animal that actively transmits an infectious agent between infected and susceptible vertebrates.1 To prevent and control vector-borne disease in humans, we must first understand the agent and its vectors, modes of transmission between vectors and humans and among humans, and the natural history of the resulting disease.
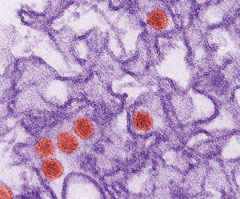 |
| Fig. 1. This is a transmission electron micrograph of ZIKV. Virus particles (in red) are 40nm in diameter, with an outer envelope and an inner dense core. Photo: CDC / Cynthia Goldsmith. |
Vectors can transmit infectious agents in two ways. For mechanical transmission, the vector serves as a vehicle whereby the infectious agent is conveyed from one host to another without undergoing a stage of development or multiplication.1 In biological transmission, the agent undergoes some stage of development or multiplication in the vector.1 In the latter, the vector serves either as an intermediate or definitive host.
The Zika Challenge
Zika virus (ZIKV) is a mosquito-borne Flavivirus isolated from the Zika forest of Uganda in 1947.2 Flaviviridae is a family of positive, single-stranded, enveloped RNA viruses found in arthropods such as ticks and mosquitoes, and can infect humans (Figure 1). Members of this family belong to a single genus, Flavivirus. Mosquito species within the Aedes genus (primarily Ae. aegypti) carry the ZIKV. Aedes mosquitoes usually bite during the day with peaks during early morning and late afternoon/evening.2,3 Sexual transmission of ZIKV has been reported.2,3 A pregnant mother can transmit the virus to her fetus, and other modes of transmission such as blood transfusion may be possible.2-4 ZIKV does not appear to spread from casual contact.
Until now, ZIKV had remained an obscure agent confined to a narrow equatorial belt running across Africa and into Asia. In 2007, the first large outbreak was reported from the Island of Yap (Federated States of Micronesia).2,3 The Pan American Health Organization issued an alert in May 2015 regarding the first confirmed ZIKV infection in Brazil.
In February 2016, the World Health Organization declared ZIKV a Public Health Emergency of International Concern because of clusters of microcephaly and other neurological disorders in some areas.2-4 ZIKV has now circled the globe, arriving not only in the Americas—including the United States—but also in Cape Verde in West Africa, near its presumed ancestral home (Figure 2). There have been 43 locally acquired mosquito-borne cases reported in the continental United States, all of which occurred in Florida (Figure 3).
 |
| Fig. 2. All countries and territories with active ZIKV transmission. Photo: CDC. Click image to enlarge. |
Symptoms and Signs
More than 80% of ZIKV infections are asymptomatic. In those that do develop symptoms, the incubation period is typically a few days.5,6 The systemic symptoms of ZIKV infection are usually mild and last for several days to a week after being bitten by an infected mosquito. Symptomatic patients typically have a mild course of disease characterized by: fever, maculopapular skin rash, joint pain, red eye or a combination of all of these. Severe disease and fatalities due to ZIKV are rare.5,6
Guillain-Barré syndrome has been reported in patients with suspected ZIKV infection.6 There may also be a link between ZIKV and acute disseminated encephalomyelitis, an autoimmune disorder that affects the brain and spinal cord similar to multiple sclerosis.7 ZIKV infection during pregnancy can cause microcephaly, which stunts proper formation of the head and brain, causing severe and sometimes fatal brain damage, miscarriage or stillbirth.4,5 Pregnant women in areas where ZIKV have been reported are advised to take steps to prevent mosquito bites.6
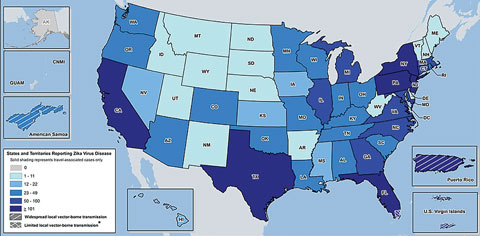 |
| Fig. 3. Laboratory-confirmed Zika virus disease cases reported to ArboNET by state or territory as of September 14, 2016. Photo: CDC.Click image to enlarge. |
Ophthalmic Complications
Investigators in Brazil have reported macular and optic nerve abnormalities in a study of 29 infants with microcephaly associated with ZIKV congenital infection.4,5 In another report, ophthalmic findings included gross macular pigment mottling, chorioretinal atrophy, optic nerve hypoplasia, increased cup-to-disc ratio, iris coloboma and lens subluxation.8 Additional findings of blood vessel changes, hemorrhagic retinopathy and torpedo maculopathy in infected infants have been described. It is not known if these findings are a direct result of the ZIKV infection or a consequence of microcephaly. Infected adults have presented with clinical signs of uveitis and a nonpurulent conjunctivitis (Table 1).9,10
Table 1. Ophthalmic Signs of Zika Viral InfectionZIKV in adults
ZIKV in infants with microcephaly
|
Diagnosis and Management
Individuals should see their health care provider if they have any of the symptoms described and have visited an area with reported ZIKV.
Detecting ZIKV RNA is the gold standard of confirmation of infection. ZIKV can be isolated in cell culture from urine, semen, saliva and breast milk. More recently, investigators detected and isolated ZIKV from conjunctival fluid.11 Also order blood tests to look for similar viruses such as dengue and chikungunya.6,10
A person diagnosed with ZIKV infection should try to prevent mosquito bites for the first week of the illness. The virus usually requires non-specific treatment. Patients should be advised to get plenty of bed rest, drink clear fluids and treat pain and fever accordingly.10 There is no specific antiviral treatment for ZIKV at this time.
Our Role Beyond Clinical Care
The CDC encourages all providers to report suspected cases of ZIKV infection to their state health department to help reduce the risk of local transmission. As part of an examination of all patients with possible congenital ZIKV infection, the CDC recommends an eye examination be performed, including retinal evaluation, either in the hospital or within one month after birth.6,10
Pregnant patients during any trimester should postpone travel to an area with ongoing ZIKV transmission.6,10 Testing for the virus can be offered to any asymptomatic pregnant patients who have traveled to areas with ongoing ZIKV transmission, pregnant patients who exhibit two or more symptoms consistent with ZIKV disease and pregnant patients who reside in areas with ongoing ZIKV transmission. The CDC Laboratory and several state health departments are performing ZIKV virus testing.
Currently there is no vaccine. The arbovirus pandemics suggest the one-bug-one-drug approach is inadequate.12 Broad-spectrum pharmacotherapies effective against whole classes of viruses are needed.
|
1. National Institutes of Health, Biological Sciences Curriculum Study. NIH Curriculum Supplement Series. 2007. Understanding Emerging and Re-emerging Infectious Diseases. Available at www.ncbi.nlm.nih.gov/books/NBK20370/. 2. Hennessey M, Fischer M, Staples JE. Zika virus spreads to new areas—region of the Americas, May 2015–January 2016. Am J Transplantation. 2016;16(3):1031-4. 3. Kindhauser MK, Allena T, Franka V, et al. Zika: the origin and spread of a mosquito-borne virus. Bull World Health Organ. 2016:171082. [Epub]. 4. de Miranda HA, Costa MC, Frazão MAM, et al. Expanded spectrum of congenital ocular findings in microcephaly with presumed Zika infection. Ophthalmology. 2016;123(8):1788-94. 5. Meissner HC. Fragile but potentially deadly: Mosquitoes transmit illnesses to millions every year. AAP News. June 2016. 6. Petersen EE, Staples JE, Meaney-Delman D, et al. Interim guidelines for pregnant women during a Zika virus outbreak—United States, 2016. MMWR Morb Mortal Wkly Rep. 2016;65:30-3. 7. Mécharles S, Herrmann C, Poullain P, et al. Acute myelitis due to Zika virus infection. The Lancet. 2016 Apr 2;387(10026):1481. 8. de Oliveira Dias JR, Rosenfeld PJ. Zika Virus and the Eye. Retina Specialist. 2016 June:14-15. 9. Furtado JM, Espósito DL, Klein TM, et al. Uveitis associated with zika virus infection. N Engl J Med. 2016;375(4):394-6. 10. The Centers for Disease Control and Prevention. Key Messages—Zika Virus Disease. September 14, 2016. Available at www.cdc.gov/zika/pdfs/zika-key-messages.pdf. 11. Sun J, Wu D, Zhong H, et al. Presence of Zika virus in conjunctival fluid. JAMA Ophthalmology. September 15, 2016. [Epub]. 12. Fauci AS, Morens DM. Zika virus in the Americas—yet another arbovirus threat. N Engl J Med. 2016;374(7):601-4. |

