 |
An 82-year-old woman presented to her local ophthalmologist for sudden and profound loss of vision in her right eye upon awakening. The doctor diagnosed right optic nerve edema, prescribed prednisone 60mg daily and referred the patient to a neuro-ophthalmologist. Unfortunately, the patient became symptomatic for vision loss in her left eye the very next day and sought care at our ophthalmic emergency department three days later.
Upon presentation, her vision was light perception with a dense RAPD in the right eye and 20/60 in the left eye. Extraocular motilities, intraocular pressures and external slit-lamp examination were all unremarkable. The dilated exam revealed optic nerve pallor OD>OS with disc edema OS>OD and fine peripapillary hemorrhages bilaterally (Figure 1).
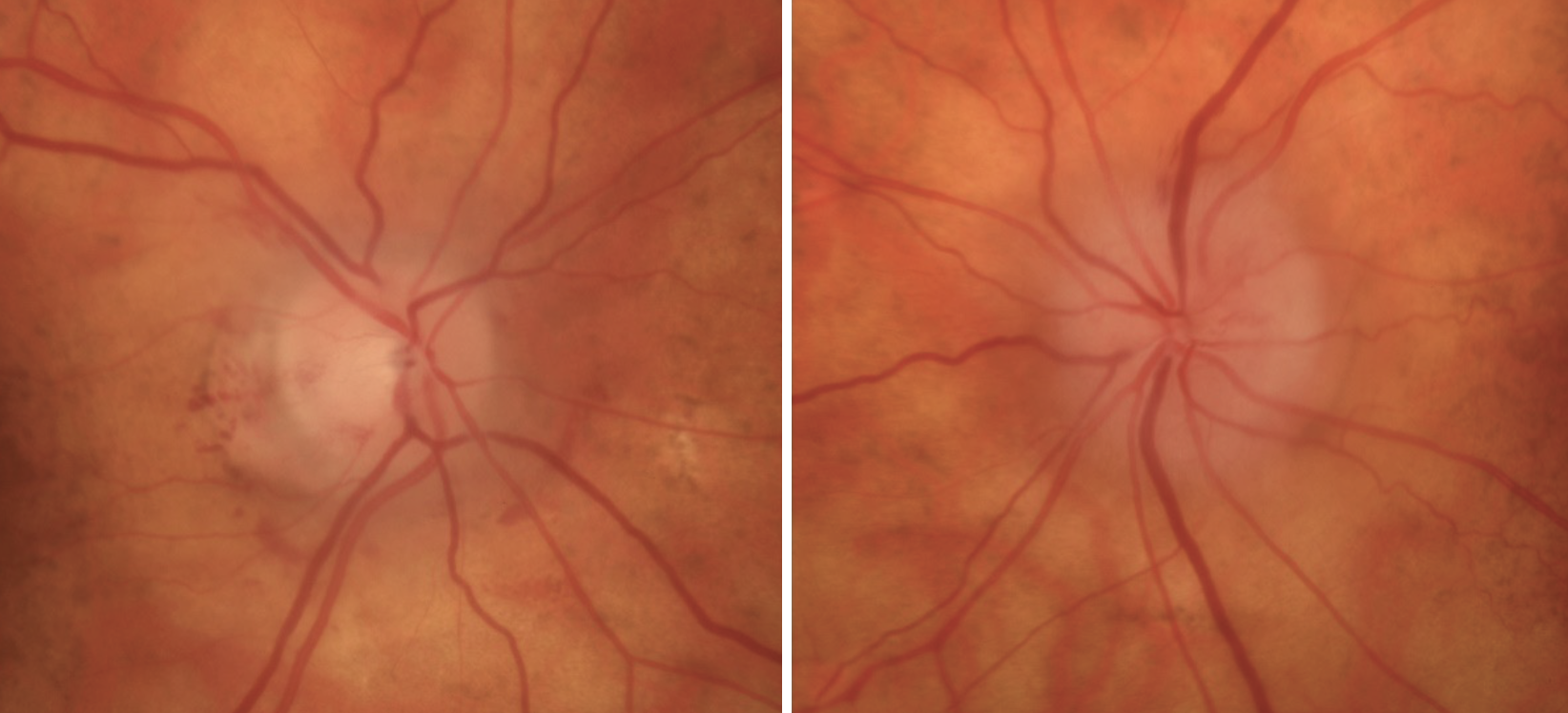 |
Fig. 1. Right (left) and left (right) optic nerves. The right nerve was pallid with resolving edema, and the left nerve was slightly pallid with significant edema. These clinical pictures support the time frame of the patient’s vision loss. Click image to enlarge. |
The clinical vignette of an elderly woman with bilateral pallid nerve edema in the setting of profound vision loss aroused suspicion for giant cell arteritis (GCA). A problem-focused review of systems was completed and revealed that the patient had been experiencing mild right brow and temporal headaches. She also endorsed 14 pounds of unintentional weight loss due to reduced appetite over the last six months, generalized fatigue and jaw claudication. Interestingly, four months prior to vision loss, she had been experiencing hand and hip girdle pain and was diagnosed with arthritis by her primary care provider; her symptoms abated with a course of oral steroids.
Laboratory studies and ophthalmic imaging were completed during her emergency department visit (Figures 2 and 3). The erythrocyte sedimentation rate (ESR) was 21mm/hour, C-reactive protein (CRP) was 0.4mg/dL, and a complete blood count revealed thrombocytosis (platelets 414x103/µL) and neutrophilia. We suspected that her inflammatory markers could have been normalized by three days of oral corticosteroid use prior to presentation, and despite “normal” ESR and CRP values, an urgent temporal artery biopsy (TAB) was scheduled. Three days of intravenous (IV) corticosteroids were initiated.
Two days after her initial presentation, the TAB was completed and revealed transmural foci of granulomatous inflammation of the temporal artery, consistent with GCA. After receiving three days of IV corticosteroids, she was transitioned to 80mg prednisone. Although visual acuity did not significantly recover, the patient reported subjective improvement of vision OS. She was referred to a rheumatologist for continued management of GCA and continues follow-up care with our neuro-ophthalmology team.
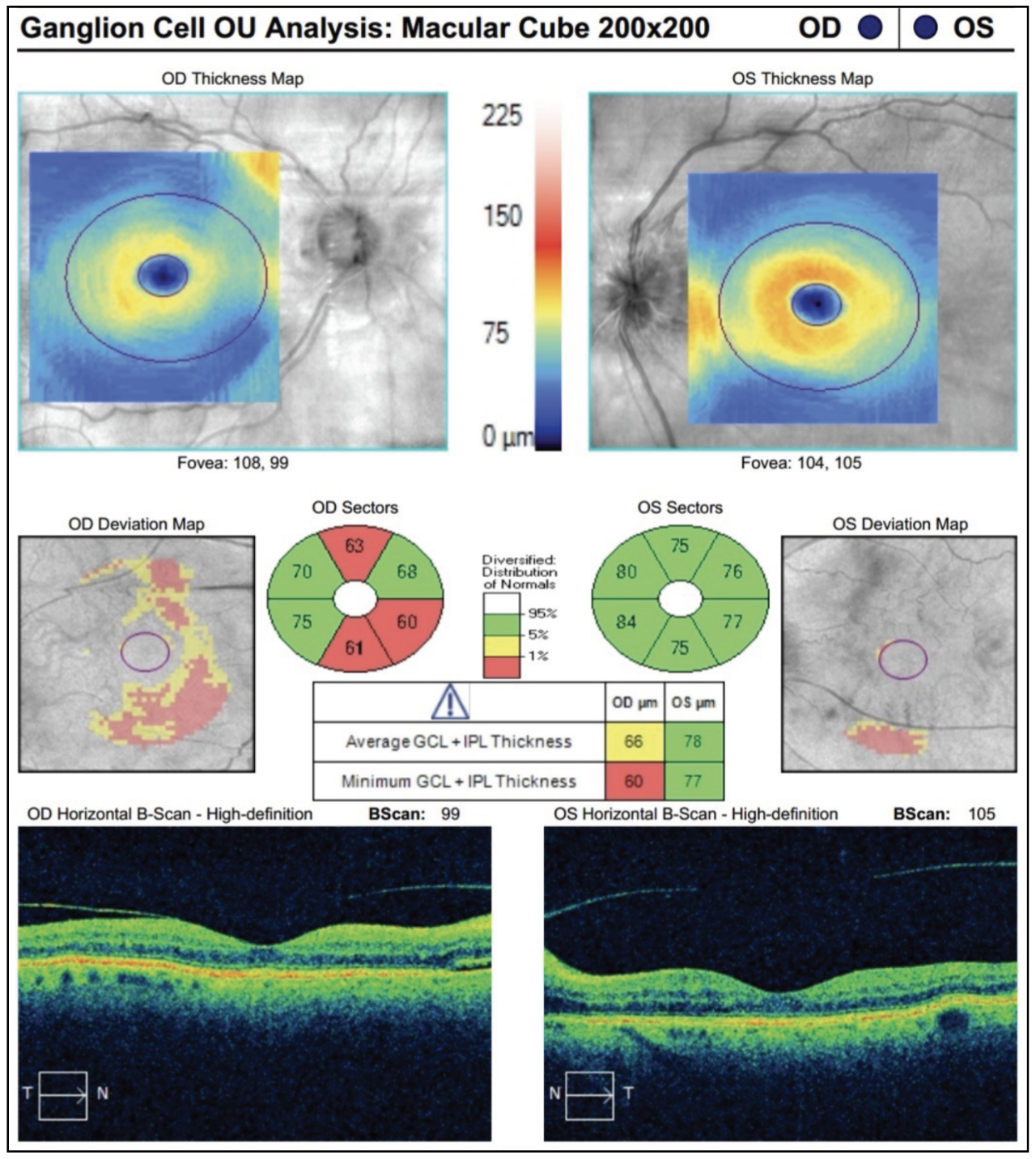 |
Fig. 2. The patient’s OCT ganglion cell analysis reveals early thinning in the right eye but a normal study in the left. Click image to enlarge. |
Clinical Presentation
Due to its potential to cause permanent vision loss within days, GCA is a true ophthalmic emergency. Rather than an ophthalmic condition, it is a systemic autoimmune condition caused by inflammation within the walls of medium and large arteries.1 It almost exclusively affects individuals aged 50 and older.
The most common symptom of GCA is headache, usually temporal or occipital and acute or subacute in onset. Others include lethargy, weight or appetite loss, fever, stroke symptoms, pain and stiffness in the hip girdle and shoulders and jaw claudication. Ask patients about each symptom specifically; most people would not associate unintentional weight loss or hip pain to an ophthalmic condition.
The most widely recognized ophthalmic manifestation of GCA is vision loss (amaurosis fugax or permanent) due to anterior ischemic optic neuropathy (AION). This is termed arteritic AION (A-AION) to differentiate it from non-arteritic AION (NA-ION), a much more common condition seen classically in patients with cardiovascular risk factors. A-AION presents with chalky white disc edema and profound vision loss in one or both eyes. There may or may not be disc hemorrhages and cotton wool spots.
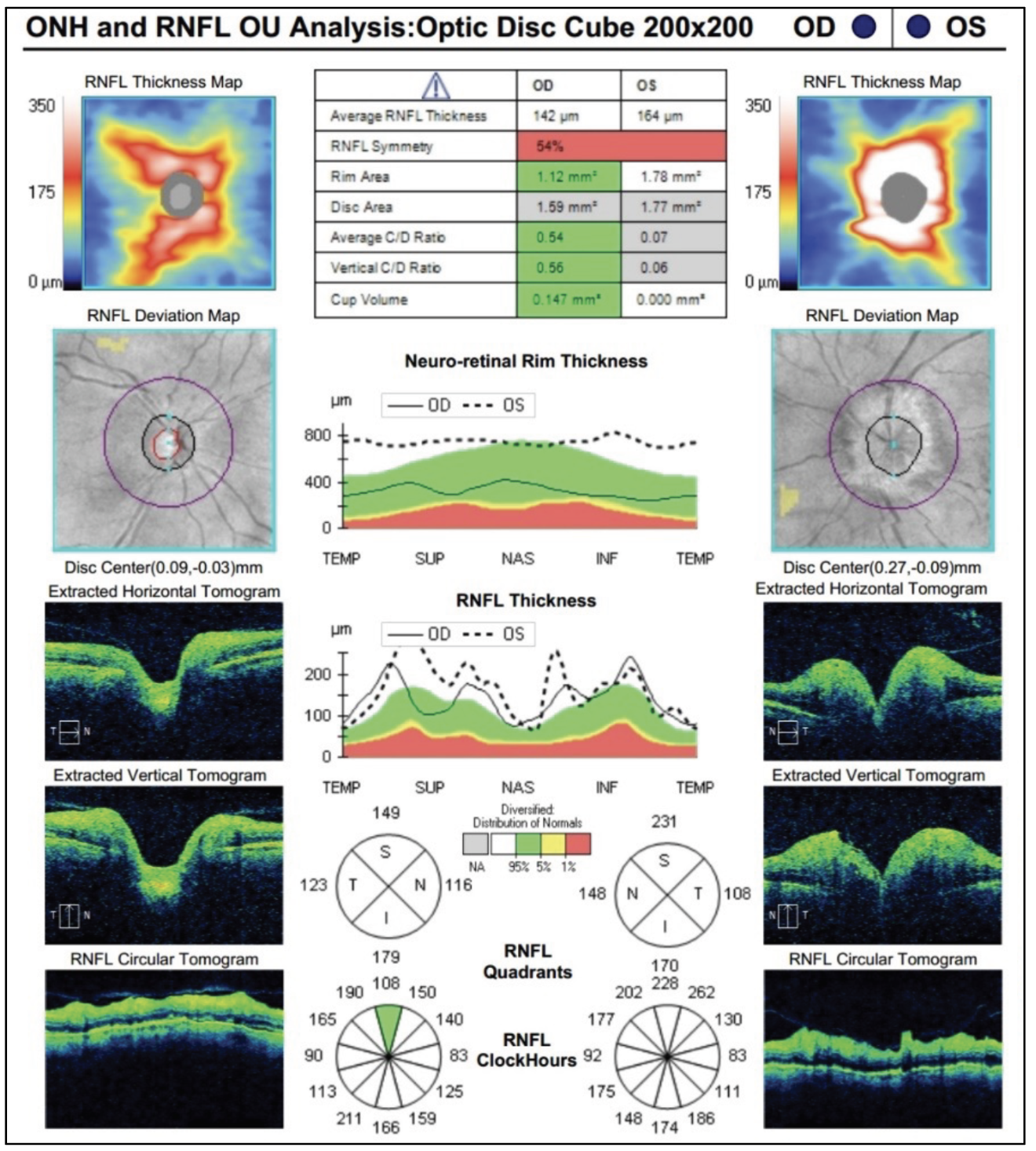 |
| Fig. 3. OCT RNFL revealed thickening circumferentially, greater in the left eye than in the right. Click image to enlarge. |
Visual field testing may be helpful in distinguishing A-AION from NA-AION, but it is not diagnostic. An inferior altitudinal defect is common in NA-AION, but it may also be the presenting field defect in A-AION. We cannot, therefore, rely on any one clinical finding such as a lack of pallor or near-normal visual acuity, as this could misplace our suspicion and cause us to miss this critical diagnosis. I have seen a patient with GCA presenting with disc edema and 20/20 vision who unfortunately progressed to permanent and severe vision loss despite timely treatment.
Other neuro-ophthalmic symptoms of GCA include diplopia and scintillating scotoma. Consider this diagnosis in patients with new cranial neuropathies or visual aura-like symptoms, particularly if their review of systems is suggestive.2 Lesser-known ophthalmic manifestations are those secondary to severe ocular ischemia, some of which include corneal edema, retinal artery occlusions, dilated pupils, peripheral retinal hemorrhages and Amalric choroidal infarcts.3-6 Posterior ischemic optic neuropathy can also be a diagnostically challenging feature of the disease, presenting with severe vision loss and a normal-appearing fundus exam.7
Workup for Suspected GCA
The recommended basic lab studies are ESR, CRP and complete blood count with differential. While there is no strict cutoff value for these tests, higher ESR and CRP values (especially simultaneously) increase the suspicion of GCA. One study revealed that the odds ratio of a positive TAB was 1.5 times greater with ESR >47mm/hour, 5.3 times greater with CRP >2.45mg/dL and 4.2 times greater with platelet counts >400x103/µL.8,9 Normal values do not rule out a GCA diagnosis, but they do make it less likely.10
The American College of Rheumatologists set the following criteria for GCA diagnosis (at least three must be met):
- age ≥50 years at onset,
- new onset of localized headache,
- tenderness of temporal artery or decreased temporal artery pulsation,
- elevated ESR and
- positive TAB
These guidelines have a sensitivity of 93.5% and a specificity of 91.2%.11 In the United States, a TAB is usually completed by oculoplastics and vascular surgeons and less often by general and plastic surgeons.12 It is generally performed ipsilateral to the affected eye. There is emerging evidence that non-invasive duplex sonography of the temporal arteries or high-resolution MRI can be useful in diagnosis.13 A TAB, if performed, should be completed within one to two weeks of initiating corticosteroids, as waiting too long can result in a false negative.14,15 In one study, the rate of positive test results fell from about 90% to 50% after only five or more days of corticosteroid use.16
If you don’t have a laboratory on-site, send the patient to the emergency department for proper workup and treatment. Convey the suspected diagnosis and necessary labs to the receiving physician either via printed letter or phone call, but preferably both. It may also be helpful to provide your telephone number to facilitate the patient’s care and field any questions that may arise. Remember that since the clinical vignette of GCA may mimic that of a stroke (i.e., acute monocular or binocular vision loss, diplopia, amaurosis fugax), the emergency department provider may choose to also perform a stroke assessment.
Treatment
When GCA is suspected, time is of the essence. While a biopsy-proven diagnosis is the gold standard, we cannot afford to await the results. Positive lab testing combined with clinical suspicion is enough to initiate treatment. Recall that GCA is an autoimmune inflammatory disorder, so the treatment is immunosuppressive (high-dose corticosteroids). Patients with visual symptoms are generally treated with 500mg to 1,000mg IV methylprednisolone for three days followed by oral corticosteroids, usually starting with 60mg to 80mg prednisone daily with a protracted taper over two to three years. Some clinicians also advocate for low-dose aspirin use (100mg daily).17
Another therapeutic option is tocilizumab (Actemra, Genentech), an IL-6 receptor antagonist that is FDA-approved as a once-weekly subcutaneous injection to treat GCA, particularly when reduction of dependence on corticosteroids is desired. These patients should be comanaged with rheumatology, as well as neuro-ophthalmology, if possible.
A relapse of disease occurs in roughly 50% of GCA cases, so monitoring for this potential and educating patients about it is critical.
When patients present with any of the signs or symptoms discussed, it is important that we maintain GCA on our differential diagnosis list, ask appropriate follow-up questions and refer emergently for further testing and treatment. We have the potential to save patients’ vision with this diagnosis.
Dr. Bozung currently practices at Bascom Palmer where she primarily sees patients in the hospital's 24/7 ophthalmic emergency department. She also serves as the optometry residency program coordinator. Dr. Bozung is a fellow of the American Academy of Optometry and a member of the Florida and American Optometric Associations. She is a founding board member of Young OD Connect and serves on the editorial board for Review of Optometry. She has no financial interests to disclose.
|
1. Smith JH, Swanson JW. Giant cell arteritis. Headache. 2014;54(8):1273-89. 2. Caselli RJ, Hunder GG, Whisnant JP. Neurologic disease in biopsy-proven giant cell (temporal) arteritis. Neurology, 1988;38(3):352-9. 3. Tran AQ, Yannuzzi NA, Motulsky EH, et al. Swept-source optical coherence tomography angiography of an Amalric choroidal infarction in a rare presentation of giant cell arteritis with bilateral corneal edema. Ophthalmic Surg Lasers Imaging Retina. 2018;49(10):e157-60. 4. Pellegrini F, Prosdocimo G, Bonsanto D, Machin P, Foroozan R. Thick corneas, large pupils, and a giant problem. Surv Ophthalmol. 2018;63(4):595-9. 5. Fineman MS, Savino PJ, Federman JL, Eagle RC Jr. Branch retinal artery occlusion as the initial sign of giant cell arteritis. Am J Ophthalmol. 1996;122(3):428-30. 6. Williams ZR, Wang X, DiLoreto DA Jr. Central retinal artery occlusion with subsequent central retinal vein occlusion in biopsy-proven giant cell arteritis. J Neuroophthalmol. 2016;36(3):290-1. 7. Albarrak AM, Mohammad Y, Hussain S, Husain S, Muayqil T. Simultaneous bilateral posterior ischemic optic neuropathy secondary to giant cell arteritis: a case presentation and review of the literature. BMC Ophthalmol. 2018;18(1):317. 8. Walvick MD, Walvick MP. Giant cell arteritis: laboratory predictors of a positive temporal artery biopsy. Ophthalmology. 2011;118(6):1201-4. 9. Foroozan R, Danesh-Meyer H, Savino PJ, et al. Thrombocytosis in patients with biopsy-proven giant cell arteritis. Ophthalmology. 2002;109(7):1267-71. 10. Parikh M, Miller NR, Lee AG, et al. Prevalence of a normal C-reactive protein with an elevated erythrocyte sedimentation rate in biopsy-proven giant cell arteritis. Ophthalmology. 2006;113(10):1842-5. 11. Hunder GG, Bloch DA, Michel BA, et al. The American College of Rheumatology 1990 criteria for the classification of giant cell arteritis. Arthritis Rheum. 1990;33(8):1122-8. 12. Micieli JA, Micieli R, Margolin EA. A review of specialties performing temporal artery biopsies in Ontario: a retrospective cohort study. CMAJ Open. 2015;3(3):E281-5. 13. Hellmich B, Agueda A, Monti S, et al. 2018 Update of the EULAR recommendations for the management of large vessel vasculitis. Ann Rheum Dis. 2020;79(1):19-30. 14. Maz M, Chung SA, Abril A, et al. 2021 American College of Rheumatology/Vasculitis Foundation guideline for the management of giant cell arteritis and Takayasu arteritis. Arthritis Rheumatol. 2021;73(8):1349-65. 15. Jiang Z, Ji H, Dong J. Temporal artery biopsy for suspected giant cell arteritis: A mini review. Indian J Ophthalmol. 2023;71(10):3299-304. 16. Hauenstein C, Reinhard M, Geiger J, et al. Effects of early corticosteroid treatment on magnetic resonance imaging and ultrasonography findings in giant cell arteritis. Rheumatology (Oxford). 2012;51(11):1999-2003. |

