 |
Q:
I had a patient finish treatment four months ago for Acanthamoeba keratitis and then inquire about having LASIK or PRK performed. Her eye is quiet, and she has a faint central scar over the visual axis with 20/30 acuity. Do I offer her surgery? If so, which procedure?
A:
“Before offering refractive surgery, one must understand the life cycle of Acanthamoeba,” says Paymaun Asnaashari, OD, who practices in northern California. It has two distinct stages—a trophozoite stage and a dormant cyst stage.1 Under favorable conditions, an active organism remains in the trophozoite stage and produces an infection.1 Under harsh conditions, such as cell-crowding, reduced pH and no food source, Acanthamoeba can transform into a dormant cyst.1
The Cyst Risk
Dormant cysts are highly resistant and may subsequently reactivate, Dr. Asnaashari notes, prolonging the infection and necessitating further aggressive treatment. He adds that even once a patient has completed treatment for Acanthamoeba keratitis, a risk still remains. He suggests consulting with a corneal specialist and waiting six to 12 months after a patient is taken off Acanthamoeba treatment medications before performing refractive surgery. He also says examination with confocal microscopy may help detect any residual activity since the infection can be quite stealthy and appear to be completely eradicated but still be present in some form.
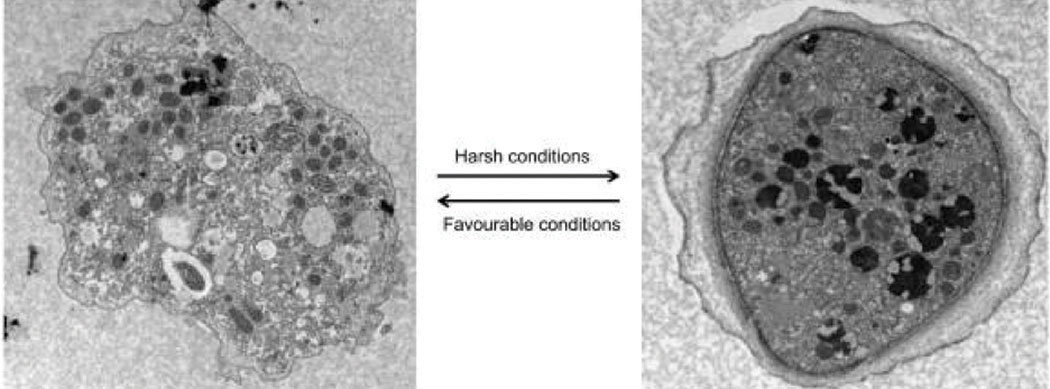 |
The trophozoite stage (left) and the dormant cyst stage. Click image to enlarge. |
One or the Other
The corneal wound healing response to injury is a critical determinant of the outcome of corneal refractive procedures, including LASIK and PRK, according to Dr. Asnaashari. The central concerns in corneal biology are the factors that promote normal tissue regeneration rather than scarring.2 The highly organized and ordered collagen fibril network in the stroma accounts for the cornea’s mechanical strength and transparency, therefore, the disruption of the epithelium and Bowman’s layer due to an injury can cause keratocytes in the anterior stroma that create a fibrotic response, which leads to scarring.2-4 He adds that the onset of corneal scarring can create loss of stromal tissue and visual acuity, weakening stromal integrity and corneal strength. Therefore, he notes that deciding whether LASIK or PRK is the best option for a patient remains a challenge.
Weaker corneal scar tissue can increase the risk of refractive surgery complications, according to Dr. Asnaashari. Scar tissue may lead to an abnormal lamellar cut during the creation of a LASIK flap, leading to flap irregularities and complications, which can reduce postoperative best-corrected visual acuity.5 If the scar is central, he recommends exercising caution with LASIK, as visual acuity can still be affected following the procedure. In addition, he says scarring can cause a patient to develop a thin cornea, in which LASIK is contraindicated.
In patients with central corneal scars, PRK could be the best option.6 PRK may decrease corneal scar depth or even remove the scar entirely and avoids flap complications characteristic of LASIK.6 However, the healing time and infection risk associated with PRK are mildly increased in comparison with LASIK.5
Clinicians should weigh the pros and cons of LASIK and PRK in each of their cases and use their clinical expertise and experience to guide them in their treatment decision.
| 1. Siddiqui R, Khan NA. Biology and pathogenesis of Acanthamoeba. Parasit Vectors. 2012;5:6. 2. Torricelli AAM, Santhanam A, Wu J, et al. The corneal fibrosis response to epithelial-stromal injury. Exp Eye Res. 2016;142:110-8. 3. Ljubimov AV, Saghizadeh M. Progress in corneal wound healing. Prog Retin Eye Res. 2015;49:17-45. 4. Wilson SL, El Haj AJ, Yang Y. Control of scar tissue formation in the cornea: strategies in clinical and corneal tissue engineering. J Funct Biomater. 2012;3(3):642-87. 5. Shovlin JP. Scars: not All doom and gloom. RO. 2015;152(7):82. 6. Rathi VM, Vyas SP, Sangwan VS. Phototherapeutic keratectomy. Indian J Ophthalmol. 2012;60(1):5-14. |

