 |
A 34-year-old male presented to the ophthalmic emergency department with acute loss of vision in his right eye. He had been using a circular saw to cut a piece of wood at work and, although he endorsed wearing sunglasses at the time, he felt something hit his right eye. He proceeded to rinse the eye with water to remove any particulate matter.
On presentation, his visual acuity was 20/60 OD and 20/25 OS. Intraocular pressures (IOPs) were 17mm Hg OD and 15mm Hg OS. The pupils were noted to react briskly and equally to light without afferent pupillary defect. Extraocular motility testing was normal.
On examination, the left eye was unremarkable. There was a small subconjunctival hemorrhage present nasally in the right eye, and within this area of hemorrhage, a very small 1mm conjunctival laceration was identified. Gentle exploration of the conjunctival laceration with a sterile cotton-tipped applicator and topical anesthetic did not reveal any foreign material nor provoke a positive Seidel sign. The cornea was clear aside from an old scar, but there were significant pigmented cells in the anterior chamber. The vitreous appeared quiet without hemorrhage or white blood cells. With further fundus examination via indirect ophthalmoscopy, a small shiny foreign body was seen in the interior vitreous chamber just overlying the retina. There was no retinal tear or detachment appreciable.
Given that the foreign body was likely metallic and the patient did not know the date of his last tetanus vaccination, a TDAP (tetanus, diphtheria and pertussis) vaccine was administered in the emergency department. Upon further discussion, the patient reported he had last eaten about two hours prior to presentation, and therefore surgery to remove the foreign body would need to occur the following day. Throughout the evening and night, the patient instilled topical antibiotic drops to the right eye. Intravitreal antibiotics were considered but held due to the relative lack of intraocular inflammation at the time of his visit.
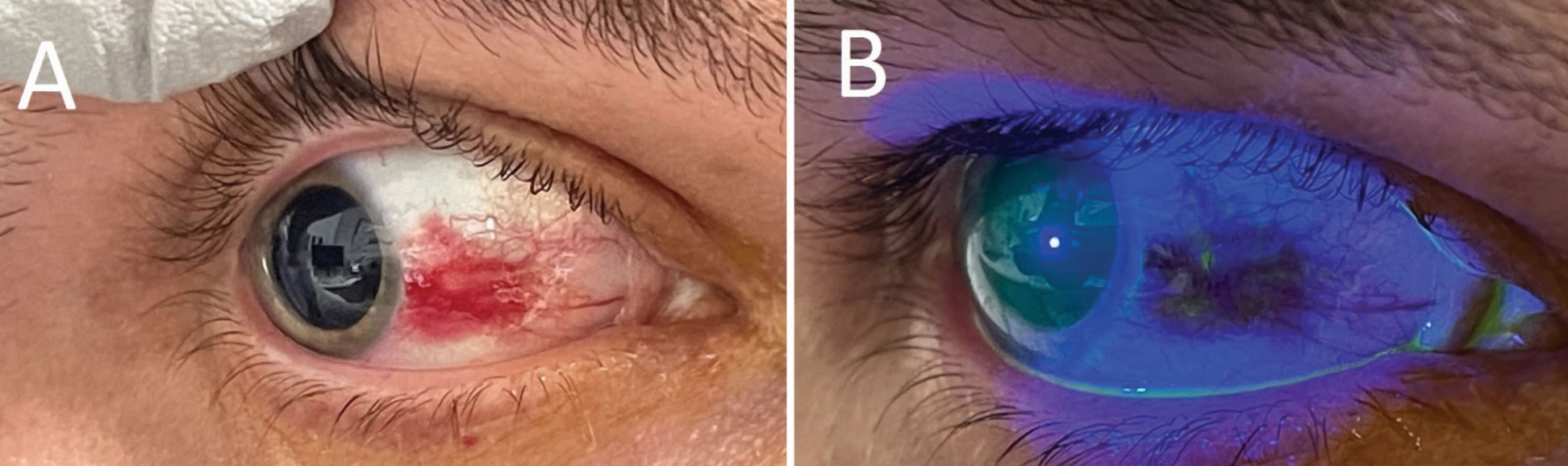 |
(A) Right eye under white light, revealing a focal subconjunctival hemorrhage in an otherwise quiet-appearing eye. (B) After sodium fluorescein application, there was a tiny conjunctival defect appreciable in the area of hemorrhage. Click image to enlarge. |
Verdict
Our patient was diagnosed with an open globe injury with intraocular foreign body (IOFB) of the right eye. At the time of his evaluation in the emergency department, the full thickness combined conjunctival and scleral wound was Seidel-negative and had already self-sealed. It is not uncommon for small, sharp projectile objects to create self-sealing wounds, making them hard to identify clinically.
Eyes with IOFBs are considered to have open-globe injuries due to the penetration of the eye wall. Of all open-globe injuries, it is estimated that anywhere between 18% to 41% have an IOFB present, most of which are in the posterior segment.1 Over 90% of patients who present with an IOFB are young men 29 to 38 years of age, as they are particularly at risk for these injuries due to the kind of workplace environments they commonly dominate. The top causes of IOFBs include hammering, power tool use and weapon-related injuries.2,3 The most commonly encountered IOFB material is metal, followed by organic or vegetative materials, stone, plastic and glass.1,3 Since metallic IOFBs are commonly seen, it is important to recall the complications that can develop from iron (siderosis bulbi) and copper (chalcosis bulbi) degradation inside the eye, including retinal toxicity, severe intraocular inflammation, glaucoma, optic neuropathy and cataract formation.4
The visual outcome in patients with IOFBs varies widely and is related to a number of different factors, including the initial visual acuity, presence of afferent pupillary defect, presence of intraocular hemorrhage, existence of retinal detachment, development of endophthalmitis and location and size of both the IOFB and entrance wound.3
 |
An intraocular metallic shard was seen on binocular indirect ophthalmoscopy OD. Click image to enlarge. |
Discussion
When assessing a patient for any potential globe injury, obtaining a detailed history of the injury is critical. Doctors should inquire about the setting where the injury occurred (e.g., home, work), what the patient was doing when the accident occurred and whether or not the patient was wearing any protective eyewear. It is also helpful to ask whether the patient attempted any interventions themselves and when they last ate or drank something.
Standard measures are taken for patients with ophthalmic trauma, including visual acuity, extraocular motilities, pupillary testing and IOP. In some cases—for example, an obviously open-globe or injury involving extraocular muscles—it may be prudent to avoid checking IOP or assessing ocular motility. Attention should be focused on the adnexa, assessing for any signs of lid laceration or orbital trauma. Then, evaluation of the anterior and posterior segment is completed to the fullest extent possible. In some cases, a view of the posterior segment may be precluded by hemorrhage or cataract formation, so careful ultrasonography should be considered.
At times, especially when clinical exam alone cannot identify or exclude suspected IOFB, additional imaging may be useful. Typically, this would include plain film X-ray, computed tomography (CT) or magnetic resonance imaging (MRI). Of these, the CT orbit without contrast is the most commonly used and recommended study.3 This is likely for a couple of reasons. First, plain film X-ray (radiography) may not capture or identify IOFBs that are very small or not considered radio-opaque.5 Next, MRIs are contraindicated in any patient who is suspected to have trauma with metallic material, as the metal can become superheated and be mobilized by the magnetic field. This could lead to significant intraocular or intraorbital damage. Interestingly, in one rabbit model, researchers found that the size threshold required to demonstrate movement of a ferromagnetic IOFB when exposed to the MRI’s magnetic field is about 3x1x1mm.6 This and another case report series suggest that tiny metallic foreign bodies (<0.5mm) may not actually be mobilized during an MRI scan; however, this type of imaging is still not recommended due to the potential risks.7 Lastly, MRI is generally more time-consuming and expensive to obtain when compared with a CT scan.
Unfortunately, CT imaging has its limitations as well, as not all IOFB materials can be captured easily. Standard CT scan cuts of 3mm are generally too spaced out to capture small foreign bodies, so 1mm cuts should be specified. Additionally, common materials that are not easily visualized with CT scans include wood and some plastics, so caution should be exercised when ruling out these types of IOFBs.8,9
 |
CT of the orbits with 1mm cuts was performed to rule out foreign material that missed on exam. A small, hyperdense body can be seen within the right globe. Click image to enlarge. |
Outcome
The morning following presentation, our patient underwent surgery to remove the IOFB. A vitrectomy was performed, and the metallic shard was gently removed via a 2mm sclerotomy site that had been created with a blade. In cases such as this, a clean and controlled wound made intraoperatively by the surgeon is often ideal compared with the entry site of the IOFB. The eye then underwent an air-fluid exchange and was filled with 20% SF6 gas. Attention was focused on the initial wound to ensure it was still well-sealed. Finally, the sclerotomy sites and conjunctival tissues were closed. At the conclusion of the case, intravitreal vancomycin, ceftazidime and voriconazole were administered.
The patient presented for a one-day postoperative visit, at which point his vision was hand motion in the surgical eye, and the pressure was 18mm Hg. The retina was attached, and the patient was given strict return precautions with restrictions including wearing a protective hard shield over the surgical eye at all times, avoiding heavy lifting or bending and keeping water out of the eye.
By his three-week postoperative follow-up, the patient’s vision had improved to 20/200 with a residual gas bubble, and IOP remained stable. OCT of the retina was completed and confirmed normal macular anatomy, suggesting a good visual prognosis. At this time, the patient, who lived in a different state, was anxious to return home and was advised to do so by driving (rather than flying) due to the retained intraocular gas bubble. He was given recommendations to continue follow-up care locally.
Dr. Bozung currently practices at Bascom Palmer where she primarily sees patients in the hospital's 24/7 ophthalmic emergency department. She also serves as the optometry residency program coordinator. Dr. Bozung is a fellow of the American Academy of Optometry and a member of the Florida and American Optometric Associations. She is a founding board member of Young OD Connect and serves on the editorial board for Review of Optometry. She has no financial interests to disclose.
|
1. Loporchio, D., et al., Intraocular foreign bodies: A review. Surv Ophthalmol, 2016. 61(5): p. 582-96. 2. Greven, C.M., et al., Intraocular foreign bodies: management, prognostic factors, and visual outcomes. Ophthalmology, 2000. 107(3): p. 608-12. 3. Jung, H.C., et al., Intraocular Foreign Body: Diagnostic Protocols and Treatment Strategies in Ocular Trauma Patients. J Clin Med, 2021. 10(9). 4. Casini, G., et al., Ocular siderosis: a misdiagnosed cause of visual loss due to ferrous intraocular foreign bodies-epidemiology, pathogenesis, clinical signs, imaging and available treatment options. Doc Ophthalmol, 2021. 142(2): p. 133-152. 5. Saeed, A., et al., Plain X-ray and computed tomography of the orbit in cases and suspected cases of intraocular foreign body. Eye (Lond), 2008. 22(11): p. 1373-7. 6. Williams, S., et al., Ferrous intraocular foreign bodies and magnetic resonance imaging. Am J Ophthalmol, 1988. 105(4): p. 398-401. 7. Zhang, Y., et al., Tiny ferromagnetic intraocular foreign bodies detected by magnetic resonance imaging: a report of two cases. J Magn Reson Imaging, 2009. 29(3): p. 704-7. 8. Rong, A.J., et al., Multimodal imaging features of intraocular foreign bodies. Semin Ophthalmol, 2019. 34(7-8): p. 518-532. 9 Modjtahedi, B.S., et al., Imaging characteristics of intraocular foreign bodies: a comparative study of plain film X-ray, computed tomography, ultrasound, and magnetic resonance imaging. Retina, 2015. 35(1): p. 95-104. |

